Fig. 6.1
A deep probing defect on the buccal aspect of the root in an endodontically treated maxillary central incisor. The radiograph (a) shows lateral radiolucencies in the mesial and distal aspect of the root. The extracted tooth (b) shows the inflammatory tissue attached to the root
Fig. 6.2
(a–f) Patient presented to the dental office with a complaint of a “loose bridge” and “suppuration from the gingivae.” The maxillary first premolar was used as an abutment together with the maxillary canine (a). The probing defect was not contributory. The periapical radiograph (b) revealed widening of the PDL on the mesial aspect of root. Since the diagnosis of VRF was not conclusive, it was decided to perform surgical flap procedure for diagnosis and treatment. When the flap was performed, a large bony dehiscence was seen (c) filled with granulation tissue. After removal of the inflammatory tissue, a VRF was seen from the coronal part to the apical (d). The dehiscence of the buccal bone which was facing the fracture can be seen very clearly (e). The fracture was a typical buccolingual fracture, and the root was extracted in two parts (f) (Courtesy Prof. A. Tamse)
Why is the destruction so profound? Currently, there is one published study [9] that examined fractured roots and adherent tissues histologically. Specimens were studied to ascertain the pattern of the fractures and to clarify the nature and the location of irritants that were associated with the fracture. In addition, the inflammatory lesions were examined as to the nature and pattern of inflammation. These findings from this study [9] are the primary basis of information for this chapter. In this study [9], roots with clinically identified fractures were obtained following tooth extraction or during exploratory surgery (Figs. 6.3 and 6.4).
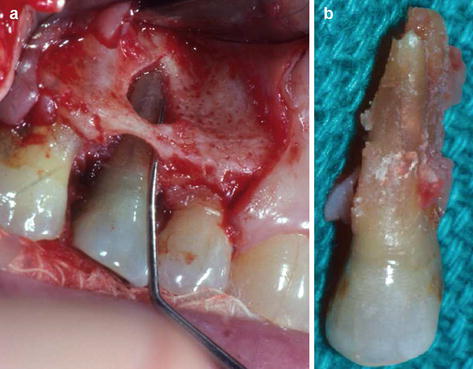
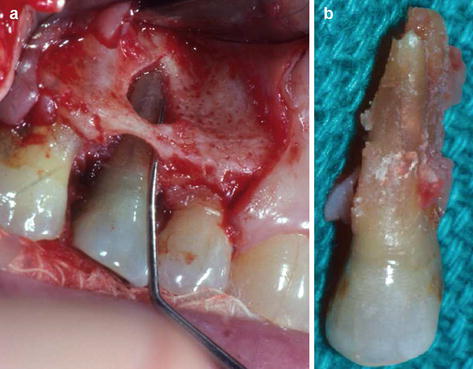
Fig. 6.3
(a, b) A large fenestration can be seen upon flap procedure performed on a maxillary lateral incisor (a). The inflammatory tissue can be seen attached to the fractured root (b)
Fig. 6.4
(a, b) Patient’s chief complaint in this case was “I have an abscess that comes and goes for nearly a year.” The tooth was endodontically treated 4 years earlier and a crown placed. Upon examination, a 10 mm probing defect was measured in the mesiobuccal aspect. The radiograph (a) shows a previously treated maxillary first molar and a large lateral radiolucency along the mesiobuccal root. Since there was no sinus tract and VRF diagnosis was inconclusive, a surgical flap procedure was performed (b). A complete bony dehiscence can be seen which was the result of a long-standing inflammation in the area facing the fracture (Courtesy Prof. A. Tamse)
More about the surgery flap procedure as a clinical adjunct to help diagnose VRF is described in Chapter 4.
The specimens were fixed in formalin, decalcified, embedded in paraffin, and cross sectioned. Histological sections were stained with H&E to identify general characteristics; alternate sections were stained for bacteria. Regions studied with the light microscope were from the cervical, middle, and apical thirds.
The histology showed patterns of the fractures in the root. Also demonstrated was that the canal and fracture spaces contained combinations of irritants that were etiologies for the inflammatory lesions that overlaid the root surface.
The characteristics of the fractures were important and followed a general pattern but with variations. These types are demonstrated in Chap. 2 on categorization.
All were in a buccolingual plane. Most extended to both surfaces (complete fractures), but some were to one surface only (incomplete fractures) (Figs. 6.5a–c and 6.6a, b).
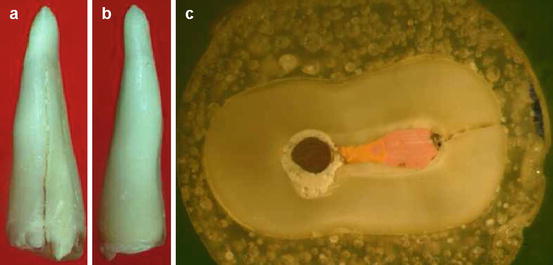
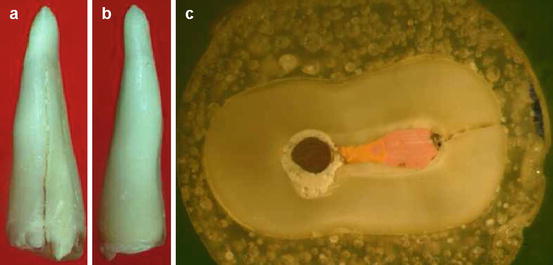
Fig. 6.5
An incomplete VRF in an extracted maxillary premolar due to a VRF. The fracture can be seen in the buccal aspect of the root (a) but not in the palatal one (b). Cross section of the root (c) demonstrates the incomplete fracture from the root canal to the external buccal surface (Courtesy Prof. A. Tamse)
Fig. 6.6
(a, b) A histological section of a vertically fractured single-rooted maxillary premolar showing the complete buccal to palatal fracture. Areas of resorptions and appositions of bone can be seen along the fracture border with vital tissue penetrating between the fragments. See the white and black arrows (a, b), These are an indication that the fracture had occurred in the past
All the fractures communicated with a canal or canals. Most fractures were likely “old” because they contained an ingrowth of vital tissue. Another indicator that the fracture had occurred in the past was resorptions and appositions of cementum-like tissue on the walls of the fracture (Fig. 6.6). The contents of the fractures were generally associated with potential and actual irritants. Bacteria were always present (Fig. 6.7).
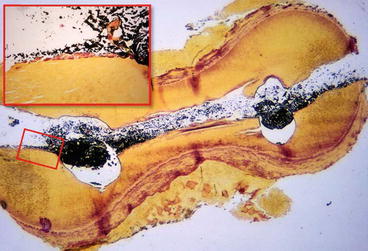
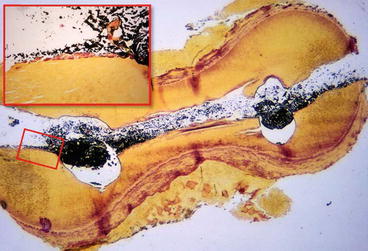
Fig. 6.7
VRF in mesial root of a mandibular molar. Although a very wide separation of the segments can be seen, it is due to an artifact. A complete buccolingual fracture is evident. Colonies of eosinophilic bacteria (red stained) are visible on the fracture surface (box insert). Sealer and gutta-percha are black because they block transmitted light and can be seen throughout the canal (Brown and Brenn. Mag × 60)
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


