Fig. 4.1
Common findings: (a) A highly located sinus tract in a mandibular molar. (b) A highly located sinus tract and deep probing in midbuccal area of another mandibular molar. The periapical radiograph (c) shows a combined bony lesion in the bifurcation area and along the lateral aspect of the mesial root which is typical for VRF in mandibular molars. The combination of the clinical signs in the endodonyically treated tooth is considered pathognomonic for VRFs
Probing Patterns
These are more diagnostic although not absolute. There is a common assumption that VRFs produce narrow and deep defects on the facial and/or lingual surfaces representing the periodontal breakdown and inflammatory process facing the fracture [10, 13, 14]. Although this may occur, patterns are not predictable. Significantly, some teeth with vertical root fractures have normal probing depths. In a recent clinical prevalence study [15], in less than 24 % of the VRF cases was a deep probing defect found. However, most do show significant deep defects with narrow or rectangular patterns (Figs. 4.1b, c and 4.2). These also are often indicative of endodontic-type lesions. When present, these deep defects are not necessarily on both the facial and lingual aspects. When they are deep on the facial and lingual, VRF is strongly suspected, but if this is the only clinical sign, it is not pathognomonic. In summary, probing patterns are not in themselves totally diagnostic. However, these deep defects in association with other findings strongly suggest the presence of a fracture. In 2008 [16], the Guidelines of the American Association of Endodontists stated that when there is a combination of a probing defect coupled with a sinus tract in an endodontically treated tooth (with or without a post), this is often pathognomonic for a VRF (Figs.4.1b, c and 4.3).
Fig. 4.2
Deep probing defects may occur on different surfaces but mostly in the buccal aspect as the buccal cortical plate is much thinner than the lingual and the palatal ones. (a) Mesiobuccal probing defect in a maxillary lateral incisor. (b) Periapical radiograph of a maxillary molar, showing the large bone loss along the MB root causing deep probing defects in the buccal as well as in the palatal. (c) A sinus tract can be seen as well on the attached gingivae at the palatal aspect
Fig. 4.3
A “pathognomonic combination” for VRF. A deep probing defect on the mesiobuccal aspect of the tooth and gutta-percha tracing cone through a highly located sinus tract (a) is directing to a “halo” radiolucency surrounding endodontically treated and restored mandibular premolar (b) (Courtesy Dr. S. Taschieri)
Often, this “pathognomonic combination” does not exist, resulting in a high percentage of misdiagnoses [4].
Radiographic Findings
Radiographs show a very wide variation of patterns of bone resorption [7, 12]. These resorptive lesions are adjacent rather than within the tooth itself. Very rarely can a tiny hair-like radiolucent fracture line be demonstrated in a root.
There are no specific radiographic pathognomonic findings because there is an assortment of patterns that often resemble other entities such as periodontal or endodontic inflammatory resorptive lesions [16]. Importantly, a vertical root fracture may demonstrate no radiographic changes [4, 10]. In a recent publication [15], it was shown that many of the VRF cases did not show any pathological bony changes (Fig. 4.4). The clinician must rely on other suggestive findings to help make a correct and timely diagnosis.
Fig 4.4
A common finding: (a) there are no significant radiographic changes. (b) A deep probing defect suggests a VRF
A most frequent radiographic feature of VRF is the “halo” (“J shaped”) (Figs. 4.5 and 4.6) appearance. This is a combined periapical and lateral radiolucency along the side of the root or a lateral radiolucency on one or both sides of the root. It may also present as an angular radiolucency from the crestal bone terminating on the side of the root (Fig. 4.7).

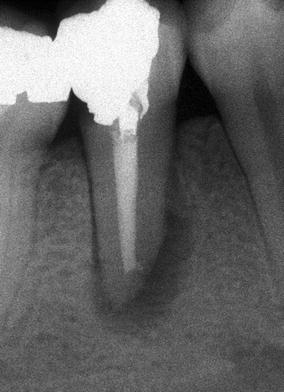
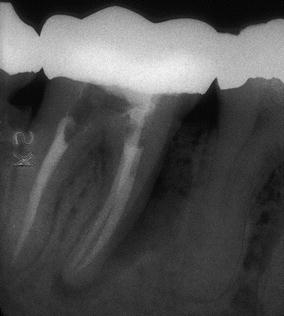

Fig. 4.5
A very large “halo”-shaped lesion in a mandibular premolar
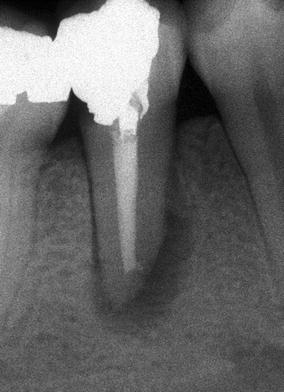
Fig. 4.6
A smaller-size “halo” radiolucent lesion in a mandibular premolar
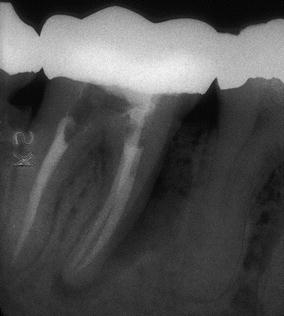
Fig. 4.7
Angular bony defect along the mesial root of a mandibular molar extending from the crestal bone to the apical part
In mandibular molars, a furcal radiolucency is frequently found (Fig. 4.8) and is often coupled with other periapical/lateral changes [4, 12, 14]. The radiolucency may have other more familiar configurations such as the periapical “hanging-drop” shape (Fig. 4.9), thus resembling a lesion of failed root canal treatment [3].
Fig. 4.8
Furcal resorptive lesions coupled with other radiolucencies around vertically fractured mesial roots may be seen often in mandibular molars (a, b)
Fig. 4.9
(a–c) Radiolucent lesions may resemble those of failed root canal treatment with persistent disease. In a mandibular molar (a) and a maxillary premolar (b). The vertical root fracture in the premolar tooth is seen very clearly (c)
Separated root segments are seldom visible on radiographs. If there is obvious separation, this is usually accompanied by a large radiolucency including and between the roots; this is inflammatory tissue separating the segments [17]. Obviously, when visible, these are absolutely diagnostic (Fig. 4.10). Segment separation with the large resorptive lesion indicates a long-standing event probably unnoticed by the patient. Lustig et al. [11] found that in most patients with other signs and symptoms (sinus tract, large osseous defect, mobility), or with acute exacerbations, greater interproximal bone loss was recorded than in patients in whom the VRF diagnosis was made at an early stage.


Fig. 4.10
Separated root fracture segments are an unusual finding and occur in long-standing inflammatory process in the area
Computed tomography has been examined as a means of identifying vertical fractures of the root [18, 19]. Most studies have been in vitro with artificially generated fractures that really cannot be compared to in vivo situations. These are quite different than the actual fracture in situ; the data from these studies may not be useful in clinical situations. Also, the obturating materials that are always present and posts that are often in place may interfere with the beam and cause scattering. This would mask the presence of the fracture anyway. However, an advantage in cone beam computed tomography may be the ability to identify and study more subtle patterns of bone resorption that are not visible on standard digital or analogue radiographs; this has not been thoroughly examined in clinical trials. There have been publications in recent years claiming to demonstrate the superiority of CBCT scans over periapical radiographs to diagnose VRFs [19–21]. However, there is considerable heterogeneity in the experimental design of these studies resulting in a wide variability in the outcomes. At this point of time, there is insufficient evidence to suggest the superiority of CBCT over conventional radiographs to detect VRFs [22]. In fact, the American Association of Endodontists Colleagues for Excellence – Cone Beam Computed Tomography in Endodontics stated [23], “What may be observed is the resultant vertical bone loss in one or more scans” rather than the fracture itself (Fig. 4.11).
Fig 4.11
Digital radiography versus cone beam computed tomography. (a) Bony resorptive lesions are not evident. (b) CBCT scans on different planes clearly show the bony defects (Courtesy Dr M. Feldman)
There is the common error of noting a radiolucent line separating the obturating material from the canal wall [7]. This is likely a radiolucent artifact. This artifact is common and is adjacent to gutta-percha or a post or is an incomplete root canal filling. This thin radiolucent line may also represent an overlying bony pattern or another radiographic structure that is easily confused with a fracture.
Therefore, radiographs (including CBCT) can be helpful in identifying a suspected vertical root fracture but are seldom solely diagnostic except in those few instances when the fracture segment separation is readily visible.
Dental History
Identifying and considering past procedures that impact the root is very helpful in diagnosis. Vertical root fractures do not occur spontaneously. There is a defined history of certain treatment modalities. These procedures have generated lateral wedging forces. All fractured roots have experienced root canal treatment and/or root end surgery as well [15
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


