Introduction
Temporary skeletal anchorage devices now offer the possibility of closing anterior open bites and decreasing anterior face height by intruding maxillary posterior teeth, but data for treatment outcomes are lacking. This article presents outcomes and posttreatment changes for consecutive patients treated with a standardized technique.
Methods
The sample included 33 consecutive patients who had intrusion of maxillary posterior teeth with a maxillary occlusal splint and nickel-titanium coil springs to temporary anchorage devices in the zygomatic buttress area, buccal and apical to the maxillary molars. Of this group, 30 had adequate cephalograms available for the period of treatment, 27 had cephalograms including 1-year posttreatment, and 25 had cephalograms from 2 years or longer.
Results
During splint therapy, the mean molar intrusion was 2.3 mm. The mean decrease in anterior face height was 1.6 mm, less than expected because of a 0.6-mm mean eruption of the mandibular molars. During the postintrusion orthodontics, the mean change in maxillary molar position was a 0.2-mm extrusion, and there was a mean 0.5-mm increase in face height. Positive overbite was maintained in all patients, with a slight elongation (<2 mm) of the incisors contributing to this. During the 1 year of posttreatment retention, the mean changes were a further eruption of 0.5 mm of the maxillary molars, whereas the mandibular molars intruded by 0.6 mm, and there was a small decrease in anterior face height. Changes beyond 1 year posttreatment were small and attributable to growth rather than relapse in tooth positions.
Conclusions
Intrusion of the maxillary posterior teeth can give satisfactory correction of moderately severe anterior open bites, but 0.5 to 1.5 mm of reeruption of these teeth is likely to occur. Controlling the vertical position of the mandibular molars so that they do not erupt as the maxillary teeth are intruded is important in obtaining a decrease in face height.
Highlights
- •
Moderate anterior open bites can be corrected with an occlusal splint and TADs.
- •
Maxillary first molars relapsed/extruded 0.5-1.5 mm in retention, but AOB stayed closed.
- •
The anterior face height decrease was minimized due to eruption of mandibular molars.
- •
Eruption of mandibular posterior teeth should be controlled during open-bite treatment.
- •
Surgery may be necessary to obtain a larger decrease in anterior face height.
Skeletal open bite, often called the long-face syndrome or condition, is regarded as a challenging orthodontic problem to correct. Many orthodontic treatment modalities have been used to close anterior open bites, such as extractions, multiloop edgewise archwires, high-pull headgear, chincups, bite-blocks, and functional appliances, but relapse is common, and even the combination of headgear and a functional appliance is ineffective in changing the skeletal pattern. Orthognathic surgery to reposition the maxilla superiorly has been the only way to create significant rotation of the mandible upward and forward, decreasing anterior face height along with correction of the open bite. Recently, temporary anchorage devices (TADs), including miniplates and miniscrews, have been used to intrude the maxillary posterior teeth to allow autorotation of the mandible to close an anterior open bite.
There have been only a few reports of outcomes with this approach beyond individual case reports. Kuroda et al concluded in an early article on this method that molar intrusion with TADs is as successful as surgery, but this was based on a small sample of 10 subjects. In a case series of 9 patients treated with maxillary posterior intrusion who had open bites that remained closed, Sugawara et al reported a 27% to 30% relapse of the maxillary molars within 1 year. Baek et al reported a maxillary molar relapse of 23% and an overbite relapse of 17% over 3 years in a case series of 9 anterior open-bite patients. Deguchi et al reported a 22% maxillary molar relapse and an overbite relapse of 13% over 2 years in a study comparing 15 patients treated with TADs and premolar extractions with 15 patients treated with conventional edgewise treatment and premolar extractions. In a report using an earlier intrusion sample from the University of North Carolina with a mixture of lingual arch and splint stabilization during intrusion, Profitt et al noted that clinically significant reeruption of intruded maxillary molars occurred in about half the patients by 1 year postsurgery. There have been no other previous reports of stability longer than 1 year that included more than 10 consecutively treated patients with the same treatment protocol.
The purposes of this study were to (1) document in a series of consecutively treated patients the amounts of molar intrusion, open-bite correction, and decrease in anterior face height obtained with TADs (miniplates or miniscrews) at the base of the zygomatic buttress and delivery of the intrusion force to a splint covering the maxillary posterior teeth; and (2) evaluate the stability of the intrusion from the completion of active intrusion to the end of orthodontic treatment, at 1 year posttreatment, and at 2 years or longer posttreatment.
Material and methods
The initial sample consisted of 33 consecutive patients with open bite and long face treated by intrusion of the maxillary posterior teeth in the private orthodontic practice of the senior author (N.R.S.) in Boone, NC, from September 21, 2005, to September 26, 2012. The routine clinical protocol included lateral cephalometric radiographs at the beginning of intrusion (T1), at its completion when the maxillary splint was removed (T2), at the completion of orthodontic treatment (T3), at the 1-year recall (T4), and at 2 or more years posttreatment (T5).
All open-bite patients who accepted treatment with this protocol (TADs and intrusive force to an occlusal splint) were included in the initial sample. This was a retrospective observation study, not a randomized clinical trial; the consecutive-patients approach was to verify that these patients were not selected on the basis of their treatment outcome. Three of the initial 33 patients were dropped because an adequate cephalogram was not obtained at T2 or T3. The final sample consisted of 11 male and 19 female subjects. Three of them did not return for a 1-year cephalogram, so 1-year data were available for 27 patients. Twenty-five of these patients returned for a cephalogram at 2 or more years posttreatment. Their sex distribution, initial open-bite severity, age, and treatment timing characteristics are shown in Table I .
| N (%) | Mean | SD | Range | |
|---|---|---|---|---|
| Female | 19 (63) | |||
| Male | 11 (37) | |||
| Growing patients (<age 20) | 15 (50) | |||
| Age at start of treatment (y) | 30 | 24.1 | 10.7 | 12.7-48.1 |
| Initial overbite (mm) | 30 | −1.2 | 1.7 | −5.0 to 1.8 |
| Time in splint treatment (y) | 30 | 0.5 | 0.1 | 0.3-0.8 |
| Total time in treatment (y) | 30 | 1.6 | 0.6 | 0.5-2.8 |
| Debond to 1-y ceph (T3-T4) (y) | 27 | 1.0 | 0.1 | 0.7-1.3 |
| Debond to >2-y ceph (T3-T5) (y) | 25 | 2.5 | 0.7 | 1.5-4.8 |
The clinical technique used with these patients is described in some detail in a recent publication, and the treatment steps are shown in Figure 1 . In brief summary, all patients had a maxillary intrusion splint (AOB-I buccal splint; AOA Laboratories, Sturtevant, Wis) that was bonded to the maxillary teeth, TADs (miniscrews or miniplates) bilaterally at the base of the zygomatic arch, and nickel-titanium coil springs to deliver the intrusive force to the splint ( Fig 1 , B ). Nickel-titanium coil springs with similar forces were used with both miniplates and miniscrews. After the completion of intrusion and removal of the splint, a continuous edgewise wire was placed in all maxillary brackets, and the molars were ligature-tied to the TADs ( Fig 1 , C ). After completion of orthodontic treatment ( Fig 1 , D ), a suck-down retainer with buttons bonded lingual to the maxillary molars was provided the same day and worn nightly with elastics to the buccal TADs ( Fig 1 , E ). Three weeks later, an occlusal coverage AOB hooked retainer (AOA Laboratories) ( Fig 1 , F ) was provided, with elastics worn nightly to the buccal TADs for the first 6 months. Then the retainer was worn without elastics indefinitely.

For 16 patients, Vector TAS miniscrews (length, 8 mm; diameter, 1.4 mm; Ormco, Orange, Calif) were placed by the orthodontist (N.R.S.) on the buccal side between either the second premolar and the first molar or the first and second molars, and they were loaded immediately. The other 14 patients had miniplates placed by the same surgeon. The choice of miniplates vs miniscrews was based on whether the patient also had a Class II or Class III malocclusion in conjunction with the anterior open bite. Miniplates with screws placed above the maxillary roots were chosen if translation of molars was necessary to correct the malocclusion. Of the 14 patients with miniplates, 12 had Leibinger Skeletal Anchoring miniplates (Stryker, Kalamazoo, Mich) retained by 3 screws and 2 had C-Tube OrthoAnchor miniplates (KLS Martin, Jacksonville, Fla) retained by 2 screws. The miniplates were loaded 18.7 ± 13.9 days later (range, 7-56 days). Intrusion was continued until a positive overbite was obtained. There were no failures of miniplate anchorage; in 1 patient, a miniscrew that was becoming loose was immediately replaced so that there was no interruption in the intrusion force during active intrusion treatment. In another patient, one miniscrew fell out the day after the patient was debanded and was not replaced, and the other miniscrew was not used during retention.
Statistical analysis
All cephalograms were digitized by a skilled technician at the University of North Carolina. Seven measurements were made at each of 5 time points to evaluate the skeletal and dental changes from intrusion and the amount of change after intrusion.
In this study, the outcomes of interest were the 7 cephalometric variables shown in Table II . Each outcome was analyzed separately by a marginal multivariate regression model with covariates (visit, age at initial visit categorized as younger vs older than 20, sex, and the pairwise interactions of age by visit and sex by visit). The interactions were included to assess whether the pattern of change for age and sex was similar over time. Considering the repeated measure property of the outcomes, the general estimating equation method with an autoregressive working correlation matrix was used. Interactions were removed if they were not statistically significant, and a reduced model was run. Significant interactions were assessed using graphic plots. The level of significance was set at 0.05 for all analyses.
| Variable | Initial to splint out (n = 30) | Splint out to debond (n = 30) | Debond to 1 year (n = 27) | Debond to >2 years (n = 25) | ||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| LAFH (ANS-Me) (mm) | −1.6 | 2.2 | 0.5 | 2.1 | −0.2 | 1.4 | −0.3 | 1.4 |
| GoGn-SN (°) | −1.2 | 1.0 | 0.2 | 1.1 | 0.0 | 0.9 | 0.0 | 0.8 |
| Overbite (mm) | 2.2 | 1.6 | 0.9 | 1.3 | −0.3 | 0.8 | −0.4 | 1.1 |
| U1-PP (mm) | 0.3 | 1.8 | 0.7 | 1.9 | −0.3 | 1.0 | −0.3 | 1.2 |
| U6-PP (mm) | −2.3 | 1.4 | 0.2 | 1.1 | 0.5 | 1.1 | 0.5 | 1.2 |
| L6-GoGn (mm) | 0.6 | 1.6 | 0.7 | 0.8 | −0.6 | 1.3 | −0.3 | 1.3 |
| L1-GoGn (mm) | 0.6 | 1.0 | 0.8 | 1.2 | −0.2 | 0.9 | −0.1 | 1.2 |
Results
The analysis showed that the pattern of response over time for the younger and older subjects was statistically significantly different for mandibular incisor to mandibular plane ( P = 0.0002), mandibular molar to mandibular plane ( P = 0.02), mandibular plane angle ( P = 0.01), and anterior face height ( P = 0.03). In all instances, there were greater changes in the younger group. The pattern of response over time was also statistically significantly different for the sexes, with greater changes in the male patients for mandibular incisor to mandibular plane, mandibular molar to mandibular plane, and maxillary molar to palatal plane ( P <0.0001 for all 3). Change in overbite was not linked to age or sex.
The means and standard deviations for changes between T1 and T2 for selected cephalometric variables are shown in Table II . The mean change in the vertical position of the maxillary molar during active intrusion was 2.3 mm, which in turn decreased the mean anterior face height and the mandibular plane angle by 1.6 mm and 1.2°, respectively. The mean change for the mandibular molar was 0.6 mm of extrusion, and the mean change in overbite was an increase of 2.2 mm.
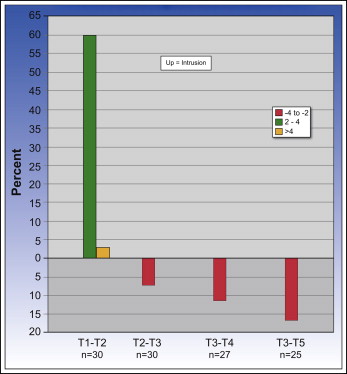
The response in a group of patients to what seemed to be identical treatment often is understood better by looking at the percentage of the patient population who had clinically significant (>2 mm) or highly clinically significant (>4 mm) changes. During active intrusion (T1-T2), 18 of the 30 patients (60%) had 2 to 4 mm of intrusion of the maxillary first molars, and 1 patient (3%) had greater than 4 mm of intrusion ( Fig 2 ). Two patients (7%) had greater than 4 mm of extrusion of the mandibular molars, and 1 patient had 2 to 4 mm of extrusion (ie, the mandibular molars erupted that much while the maxillary molars were being intruded) ( Fig 3 ). Twelve patients (40%) experienced 2 to 4 mm of decrease in anterior face height, and 3 (10%) had a decrease greater than 4 mm ( Fig 4 ). The percentage with change in overbite was similar to that for anterior face height: 12 patients had 2 to 4 mm of increase in overbite, and 5 had a greater than 4-mm increase.

Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


