Tooth ankylosis during adolescence and early adulthood can lead to infraocclusion and several interrelated, adverse sequelae at the intra-arch and interarch levels. An orthosurgical treatment modality that includes surgical luxation and immediate orthodontic traction is recommended as a conservative approach in many patients. The key to success in this approach is the timely delivery of relatively heavy and continuous forces to the luxated tooth to prevent its reankylosis. Because high reactive forces are inevitably generated, it is crucial to create a reliable source of anchorage. This report describes the successful use of an osseointegrated orthodontic implant to reinforce the anchorage during the orthosurgical repositioning of an infraoccluded molar in a young adult.
Cessation of tooth eruption occurs without an apparent physical barrier and can lead to several side effects on the interarch and intra-arch levels. Although the mechanism that causes the cessation of tooth eruption has yet to be found, the consequences are well known: infraocclusion of the tooth with lessened development of the alveolar process, tipping of the adjacent teeth, overeruption of the opposing tooth, and midline shift. The earlier these phenomena occur, the more severe the consequences, especially when they occur in the permanent dentition during adolescence, a critical period for facial and dental development. Some researchers have described localized areas of ankylosis to explain the cessation of the tooth eruption, but others disagree and believe that there might not be ankylosis. Whatever the reason, it is believed that these teeth will not respond to conventional orthodontic forces.
This report describes the successful orthosurgical treatment of a severely infraoccluded maxillary first molar in an adolescent patient, by using skeletal anchorage and continuous forces.
Diagnosis and etiology
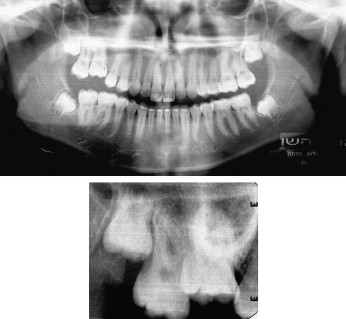
A 16-year-old girl was referred by her family dentist to the Department of Orthodontics of the Hebrew University-Hadassah School of Dental Medicine in Jerusalem, Israel, because of submergence of the maxillary right first molar. The patient had completed her orthodontic treatment 2 years before the referral. She had a well-balanced and symmetrical face, with a slightly convex profile. Intraorally, she had a Class I occlusion, with normal overbite and overjet. Several white spot lesions, observed on the labial side of the teeth in both arches and on the palatal side of the maxillary incisors, were presumed to have been related to the fixed appliances and the removable maxillary retainer during the first orthodontic treatment. The maxillary right first molar showed vital signs, but it emitted a sharp, solid sound on percussion. The occlusion showed marked disturbances that could be attributed to the influence of the ankylosed molar ( Fig 1 ): (1) there was a vertical height discrepancy of about 5 mm between the first molar and its neighboring teeth, (2) the adjacent teeth were tilted toward the affected tooth (especially the second premolar), (3) there were small spaces between the premolars mesial to the affected molar, and (4) the opposing molar showed only slight overeruption because of its occlusal contact with the tipped second premolar. The radiographic examination showed a vertical defect in the alveolar process in the immediate area of the affected tooth, caused by the cessation of molar eruption during the recent period in which significant vertical growth of the face and the jaws had occurred ( Fig 2 ).

Treatment objectives
The treatment objectives for this patient included (1) reopening space for the infraoccluded maxillary right first molar by distally tipping the mesially inclined second molar and closing the maxillary premolar spaces, (2) correcting the axial inclination of the adjacent teeth, (3) erupting the infraoccluded molar while maintaining its vitality, (4) generating alveolar bone in the area, and (5) improving the axial inclination of the maxillary incisor area.
Treatment objectives
The treatment objectives for this patient included (1) reopening space for the infraoccluded maxillary right first molar by distally tipping the mesially inclined second molar and closing the maxillary premolar spaces, (2) correcting the axial inclination of the adjacent teeth, (3) erupting the infraoccluded molar while maintaining its vitality, (4) generating alveolar bone in the area, and (5) improving the axial inclination of the maxillary incisor area.
Treatment alternatives
Six alternative therapeutic modalities for this scenario have been described in the literature: no treatment, surgical removal, prosthetic buildup, localized ostectomy, interalveolar segmental osteotomy, and orthosurgical treatment. After receiving a detailed explanation, the patient chose the orthosurgical approach, which entails surgical luxation of the ankylosed tooth with orthodontic extrusion. The risks are the possibility of tooth loss from crown, root, or alveolar fracture when the attempted luxation does not overcome an extensive ankylotic fusion, reankylosis with loss of anchorage and unwanted movement of the anchor teeth, and loss of vitality. Nevertheless, an important consideration with this option was that failure still left the other options open.
Treatment progress
Oral hygiene was much improved at the start of the second treatment. Nevertheless, the patient was treated under a strict regimen of regular professional fluoride application and mouth rinses to prevent further enamel decalcification.
The treatment stages were the following.
- 1.
A midpalatal implant was placed as the first step in the treatment, because it requires a waiting period of at least 3 to 4 months for osseointegration ( Fig 3 , A ).

Fig 3 A , Midpalatal implant; B , anchorage unit, fabricated from 0.9-mm stainless steel wire; C , intraoral occlusal view. - 2.
During this period, fixed orthodontic appliances (0.022-in slot, GAC International, Bohemia, NY) were placed in the maxillary arch. Orthodontic reopening of the molar space was performed with an open-coil spring, which reciprocally closed the spaces mesial to the first molar.
- 3.
After 6 months of treatment, a silicone pickup impression (wash and putty, Elite Orthodontics, Timbuktu, Del) was taken to prepare an anchorage unit, comprising the maxillary right second molar, second premolar, and the transfer of the midpalatal implant. The teeth and the implant were connected with a heavy 0.9-mm stainless steel wire ( Fig 3 , B and C ). On the labial side, a 0.019 × 0.025-in stainless steel wire was used as the base arch, with a step-down bend at the first molar region to increase the range of action of the elastic thread to be used to extrude the infraoccluded molar.
- 4.
The buccal wire was removed immediately before the surgical procedure to permit surgical luxation of the tooth under local anesthesia. A spread-pointer elevator was used to achieve mesiodistal mobility. Suitable extraction forceps were then applied to exert a force in the buccal and lingual directions, until the tooth reached mobility equivalent to class 3 (severe mobility of up to 1-mm amplitude) on the tooth mobility scale. Then, small eyelets were bonded to the buccal and lingual sides of the affected tooth. The base arch was replaced into the brackets, and the acrylic part of the anchorage unit screwed to the implant, and the bands on the anchor teeth were bonded with adhesive (Fuji I, GC America, Alsip, Ill). While the local anesthetic was still effective, elastic thread was tightly tied between the eyelets and the buccal and lingual wires on the affected molar to provide heavy extrusion forces ( Fig 4 , A ).
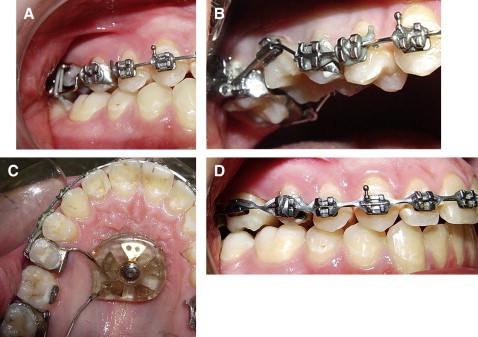
Fig 4 A , Side view showing elastic thread tied tightly between the buccal and lingual eyelets and the buccal and lingual wires of the anchorage unit; B , after 2 months of traction, there was insufficient progress in the leveling process, and space had opened between the maxillary right first and second premolars; C , a new anchorage unit was activated to distalize the second molar and open additional space for the infraoccluded molar; D , progress view after 4 weeks, showing full eruption of the infraoccluded molar and placement of an 0.018-in stainless steel wire.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


