Autotransplantation is an option for tooth replacement when a suitable tooth is available and anatomic circumstances are favorable. This case report describes successful orthognathic treatment that was combined with autotransplantation of a maxillary third molar. A 20-year-old woman had mandibular protrusion and facial asymmetry. Five years previously, her mandibular right first molar had been extracted because of dental caries. After preoperative orthodontic treatment, we performed a LeFort I procedure and a bilateral intraoral vertical ramus osteotomy to correct the patient’s mandibular protrusion and facial asymmetry. During the postoperative orthodontic treatment, the maxillary left third molar was autotransplanted into the mandibular right first molar site. The total treatment period was 24 months. As a result of these therapeutic treatments, the patient’s facial appearance was improved, and an implant was unnecessary. The autotransplanted tooth effectively supported the adjacent teeth and maintained her chewing ability.
Teeth can be lost from periodontal disease, severe caries, agenesis, trauma, or endodontic failure. This problem can be treated in various ways, including orthodontic space closure, fixed or removable partial dentures, dental implants, or tooth autotransplantation. Among various treatment options, autotransplantation can lead to shorter treatment times and improved treatment results when a suitable tooth is available and anatomic circumstances permit.
In 1950, Apfel and Miller first described the transplantation of immature third molars to first molar positions. Since then, autotransplantation of immature third molars has become a common procedure for replacing missing teeth. Recently, several studies have reported that third molars with complete root formation can also be used as donor teeth. Watanabe et al reported a survival rate of 86.8% over a mean observation time of 9.2 years. Sugai et al reported an overall 5-year survival rate of 84%. Although the current success rates are lower than the rates with dental implants, autotransplanted teeth result in good utilization and maintenance of alveolar bone and attached gingiva. Furthermore, they provide superior esthetic results, are less expense, and have the potential for orthodontic movement.
This case report demonstrates a successful orthognathic treatment that included autotransplantation of a maxillary left third molar in a patient with a missing mandibular right first molar, mandibular protrusion, and facial asymmetry.
Diagonsis and etiology
A 20-year-old woman visited the orthodontic department at Yonsei University Dental Hospital in Seoul, Korea. Her chief complaint was mandibular prognathism and facial asymmetry. On the pretreatment questionnaire, the patient reported a strong desire to improve her facial appearance. She had received orthodontic camouflage treatment because of an anterior crossbite 3 years previously, and she had used a temporary denture after the extraction of her mandibular right first molar from dental caries 5 years previously. She had no serious medical history, and no habits were reported.
Pretreatment facial photographs showed a mandibular deviation toward the right, and the patient’s eyebrows were at noticeably different levels. Her lips were incompetent, and the incisor-stomion distance was 6.0 mm ( Figs 1-3 ). Intraorally, she exhibited an Angle Class III malocclusion on the left side and an unknown molar relationship on the right side, caused by the missing mandibular first molar. The maxillary dental midline had a 1.0-mm deviation toward the left, and the mandibular dental midline had a 1.0-mm deviation toward the right. A lateral cephalometric analysis showed an SNA of 86.9°, an SNB of 86.2°, and an ANB of 0.7°. The mandibular plane angle was 35.3°, the ramus height was 58.3 mm, and the gonial angle was large, at 134.3°.

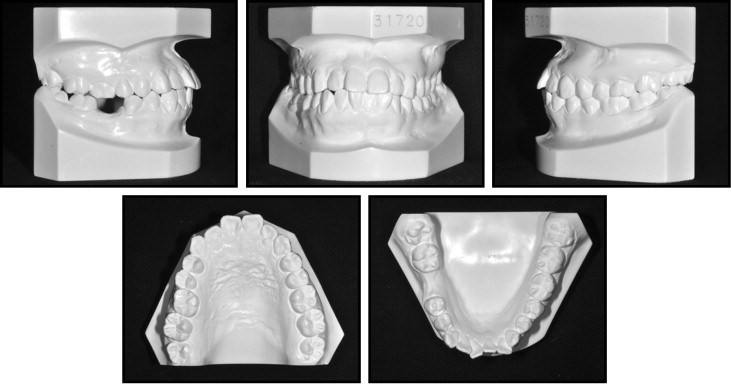
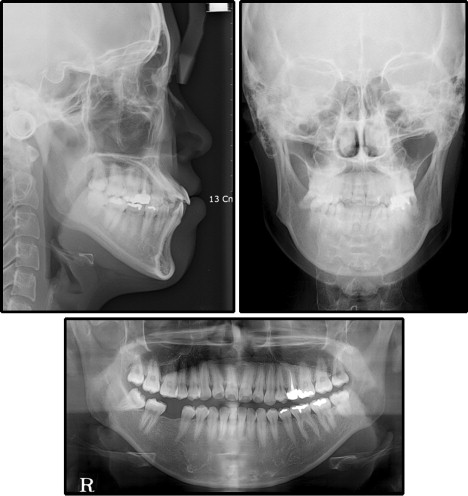
The maxillary incisors were labially inclined at an angle of 128.0° toward the SN plane, and the mandibular incisors were lingually inclined at an angle of 82.0° toward the mandibular plane. The lower lip was protrusive with respect to the E-line, and an acute nasolabial angle was noted. A posteroanterior cephalometric analysis indicated that the maxillary molars had extruded on the left side by 3.0 mm more than on the right side, and the chin was deviated by 5.0 mm toward the right. A panoramic radiograph showed that all 4 third molars had complete root formation and were fully erupted, and the periodontal tissues were healthy ( Figs 1 and 3 , Table ).
| Measurement | Norm | Pretreatment (19 y 8 mo) | Posttreatment (21 y 8 mo) |
|---|---|---|---|
| Skeletal | |||
| SNA (°) | 81.6 ± 3.2 | 86.9 | 86.4 |
| SNB (°) | 79.2 ± 3.0 | 86.2 | 81.0 |
| ANB (°) | 2.5 ± 1.8 | 0.7 | 5.4 |
| SN-GoGn (°) | 33.4 ± 5.0 | 35.3 | 38.5 |
| Gonial angle (°) | 118.6 ± 5.8 | 134.3 | 146.7 |
| Ramus height (mm) | 51.6 ± 4.2 | 58.3 | 58.7 |
| Go-Me (mm) | 76.0 ± 4.0 | 85.3 | 66.5 |
| Dental factors | |||
| U1-SN (°) | 106.0 ± 5.0 | 128 | 112.5 |
| U1-NA (°/mm) | 24.0/6.0 | 35.4/12.1 | 25.5/4.6 |
| L1-NB (°/mm) | 27.0/6.0 | 25.3/8.3 | 29.6/10.4 |
| L1-GoGn (°) | 94.0 ± 5.0 | 82 | 90.2 |
| Soft tissues | |||
| Nasolabial angle (°) | 92.9 ± 7.4 | 80 | 96 |
| E-line (mm) | −1.0 ± 2.0 | −1.5 | −2.8 |
| Upper lip/lower lip | 1.0 ± 2.0 | 3.2 | −2.5 |
Treatment objectives
Based on the cephalometric findings, this patient was diagnosed with mandibular protrusion and facial asymmetry. The following treatment objectives were planned.
- 1.
Maxilla. A total impaction of the maxilla was planned to correct the canted occlusal plane and the excessive display of gingivae and to create sagittal coordination with the mandible.
- 2.
Mandible. We planned to set back the mandible to correct the prognathism and the midline deviation. In addition, rotation of the maxillomandibular complex would reshape the bilateral gonial angle because of the bony ledge.
- 3.
Maxillary dentition. We planned to coordinate the facial and maxillary dental midlines, relieve the proclined incisor position, and achieve an ideal overbite and overjet relationship.
- 4.
Mandibular dentition. We planned to relieve the dental compensation by straightening the mandibular incisors to an upright position over basal bone; in addition, restoring the missing mandibular right first molar was expected to establish a stable occlusion.
Treatment objectives
Based on the cephalometric findings, this patient was diagnosed with mandibular protrusion and facial asymmetry. The following treatment objectives were planned.
- 1.
Maxilla. A total impaction of the maxilla was planned to correct the canted occlusal plane and the excessive display of gingivae and to create sagittal coordination with the mandible.
- 2.
Mandible. We planned to set back the mandible to correct the prognathism and the midline deviation. In addition, rotation of the maxillomandibular complex would reshape the bilateral gonial angle because of the bony ledge.
- 3.
Maxillary dentition. We planned to coordinate the facial and maxillary dental midlines, relieve the proclined incisor position, and achieve an ideal overbite and overjet relationship.
- 4.
Mandibular dentition. We planned to relieve the dental compensation by straightening the mandibular incisors to an upright position over basal bone; in addition, restoring the missing mandibular right first molar was expected to establish a stable occlusion.
Treatment alternatives
One treatment option for correcting the skeletal problems was single-jaw surgery, with only a mandibular setback. However, this would have compromised the facial esthetics. The patient had maxillary occlusal canting and excessive maxillary incisor exposure. A single-jaw surgery would not have fulfilled her expectations.
Various treatment options for the missing mandibular right first molar were considered, including orthodontic space closure, a fixed or a removable partial denture, a dental implant, and autotransplantation. A removable partial denture was not ideal because of the patient’s age; also, adjacent abutment tooth reduction would have been necessary for placing a fixed partial denture.
An orthodontic treatment approach, such as closing the edentulous space left by the missing tooth, would have been difficult and would have involved a long treatment time because it would have required protracting the mandibular right second molar by approximately 10 mm mesially. Furthermore, it was assumed that the antagonist tooth of the maxillary right second molar had disappeared. In contrast, an implant or autotransplantation was considered advantageous because it could improve the occlusion by prosthesis alone. In this patient, the maxillary left third molar had an appropriate crown size, and we expected that root canal treatment would not be difficult because the root shape was not abnormal. The patient agreed to transplantation of the maxillary left third molar into the mandibular right first molar space.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


