This case report describes the treatment of an 18-year-old man with a skeletal Class III pattern and a full-step Class III malocclusion. The orthodontic treatment included distal movement of the mandibular dentition with temporary skeletal anchorage devices. The total active treatment time was 30 months. His occlusion and facial appearance were significantly improved by the orthodontic treatment. Posttreatment records 2 years later showed excellent results with good occlusion and facial balance.
Distal movement of the mandibular molars is much more difficult than distal movement of the maxillary molars. Extraoral appliances, such as mandibular headgear, do not cause adverse side effects, but they are seldom used because of the pressure they place on the condyles. Several intraoral treatment approaches have been proposed to move mandibular molars distally. Franzulum appliances, lip bumpers, Jones jigs, and multiloop edgewise archwires can be used as intraoral appliances; however, most of them are not popular in adult treatment because of the limited amount of molar distalization, the type of tooth movement (tipping rather than bodily movement), anchorage loss, protrusion of the anterior teeth, and patient cooperation issues.
To correct anterior crossbite, mandibular anterior crowding, and mandibular dental asymmetry without extracting premolars, distalization of the mandibular teeth is a treatment option. Currently, distal movement of mandibular teeth is possible without anchorage loss with temporary skeletal anchorage devices (TSADs), but so far, there has been limited clinical research relating to the distalization of mandibular teeth and little information regarding boundaries of distal movement, type of tooth movement, and posttreatment relapse.
This case report presents a young man who had a Class III skeletal pattern with anterior and unilateral posterior crossbites and a midline deviation. His orthodontic treatment included distalization of the mandibular dentition using TSADs as anchorage to correct the anterior crossbite, mandibular anterior crowding, and mandibular dental asymmetry without extracting premolars.
Diagnosis and etiology
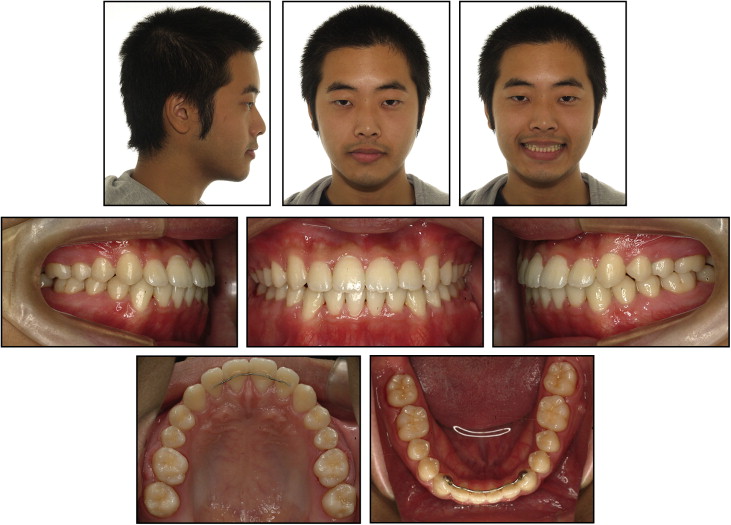
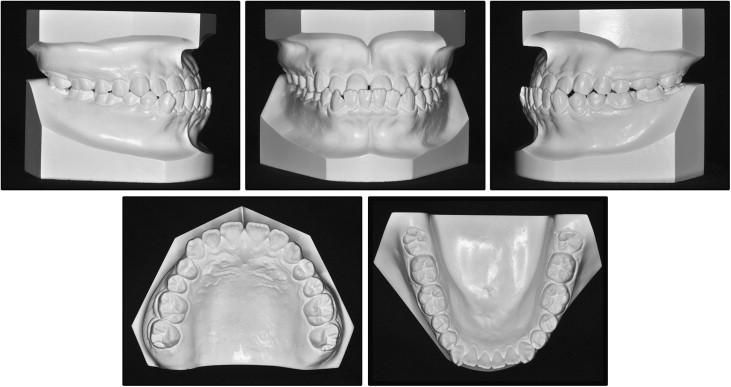
The patient, age 18 years 4 months, was referred for orthodontic evaluation by the third author. He was healthy with no specific medical problems. His chief complaint was his anterior crossbite. He had a mesofacial, symmetrical face and a prognathic mandible with a Class III appearance ( Fig 1 ). In a temporomandibular joint evaluation, he did not show muscle or joint pain or other symptoms typically associated with temporomandibular disease.
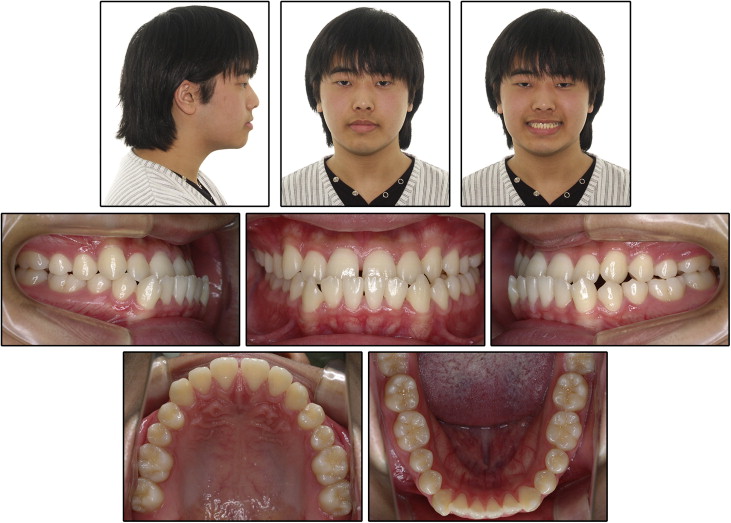
Intraorally, he showed anterior and unilateral left posterior crossbites. He had an overjet of −3 mm and a 30% overbite. He had full-step Class III canine and molar relationships on both sides, and small maxillary second premolars. He had mild spacing in the maxillary anterior dentition and mild crowding in the mandibular anterior dentition with a moderate curve of Spee on his left side. Compared with his facial midline, the maxillary dental midline was shifted 1.5 mm to the right, and the mandibular dental midline was deviated 2 mm to the left. When his mandible was guided into centric relation, a functional shift was detected because of the anterior and posterior crossbites. He also had a tongue-thrust habit when swallowing ( Figs 1 and 2 ).
A panoramic radiograph showed no caries or pathologies. His maxillary right third molar was developing, and the mandibular third molars were erupting ( Fig 3 , A ).
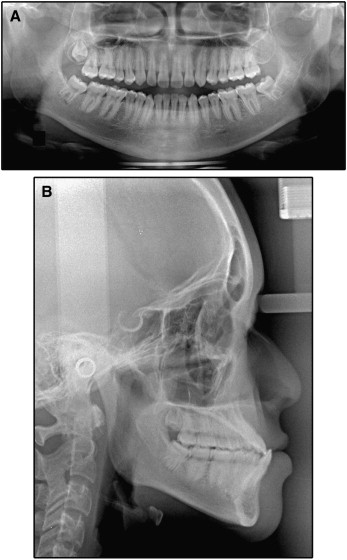
The lateral cephalometric analysis indicated a skeletal Class III pattern (ANB, −3.2°; Wits appraisal, −8.4 mm) with a hypodivergent growth pattern (SN-MP, 31.3°). The maxillary and mandibular incisors were proclined (U1-SN, 116.6°; IMPA, 93.2°) ( Fig 3 , B ; Table ). His brother also had a skeletal Class III pattern. The etiology of the Class III malocclusion appeared to be a combination of heredity and environmental factors.
| Measurement | Norm | Pretreatment | Posttreatment | 2 years posttreatment |
|---|---|---|---|---|
| SNA (°) | 82.0 | 80.9 | 81.3 | 81.2 |
| SNB (°) | 80.0 | 84.1 | 82.1 | 82.0 |
| ANB (°) | 2.0 | −3.2 | −0.9 | −0.8 |
| Wits (mm) | 1.1 | −8.4 | −2.8 | −3.0 |
| SN-MP (°) | 34.0 | 31.3 | 32.5 | 32.3 |
| FH-MP (°) | 28.2 | 22.0 | 23.3 | 23.0 |
| LFH (ANS-Me/N-Me) (%) | 55.0 | 54.4 | 54.7 | 54.1 |
| U1-SN (°) | 104.0 | 116.6 | 118.2 | 117.5 |
| U1-NA (°) | 22.0 | 35.8 | 37.0 | 36.5 |
| IMPA (°) | 90.0 | 93.2 | 90.4 | 90.7 |
| L1-NB (°) | 25.0 | 28.6 | 24.1 | 24.2 |
| U1/L1 (°) | 124.0 | 118.9 | 119.6 | 119.7 |
| Upper lip (mm) | 1.2 | −3.1 | −0.8 | −0.6 |
| Lower lip (mm) | 2.0 | 2.7 | −0.2 | −0.1 |
Treatment objectives
The following treatment objectives were established: (1) correct jaw deformities of the maxilla and the mandible, (2) correct anterior and unilateral posterior crossbites, (3) eliminate the functional shift and correct the dental midline, (4) establish Class I canine and molar relationships, (5) obtain normal overjet and overbite, (6) correct irregularities in the teeth, (7) level the curve of Spee, (8) obtain a stable occlusal relationship, and (9) improve facial and dental esthetics by establishing an esthetic smile.
Treatment objectives
The following treatment objectives were established: (1) correct jaw deformities of the maxilla and the mandible, (2) correct anterior and unilateral posterior crossbites, (3) eliminate the functional shift and correct the dental midline, (4) establish Class I canine and molar relationships, (5) obtain normal overjet and overbite, (6) correct irregularities in the teeth, (7) level the curve of Spee, (8) obtain a stable occlusal relationship, and (9) improve facial and dental esthetics by establishing an esthetic smile.
Treatment alternatives
Because of this patient’s stage of development, he did not have significant maxillomandibular growth potential left to assist in reaching the treatment goals with orthodontics alone. Orthognathic surgery to set back the mandible with the possibility of maxillary protraction, combined with fixed orthodontic treatment, was discussed with him. Skeletal discrepancy correction, maximum facial and dental esthetics, and establishment of an ideal occlusion would all be possible with this approach.
Orthodontics alone would help camouflage some skeletal and dental aspects of the malocclusion, improving esthetics and function. The orthodontic options included (1) maxillary expansion to correct the posterior crossbite, a protraction facemask at night to correct the anterior crossbite, and, if necessary, mandibular incisor extraction to correct the overjet and the anterior crossbite ; (2) extraction of 2 mandibular first premolars to upright the mandibular incisors and to correct the mild anterior crowding and the anterior crossbite; and (3) distalization of the mandibular dentition with TSADs to establish Class I canine and molar relationships.
The patient declined orthognathic surgery and the wearing of a facemask. He did not want extractions, except for the third molars. Because of this, we decided on distal movement of the mandibular dentition with TSADs to correct the full-step Class III malocclusion.
Treatment progress
Before orthodontic treatment, the patient was referred to a general dentist to verify that he had no periodontal problems and for extraction of the mandibular third molars. Preadjusted appliances with 0.022 × 0.028-in slots were bonded on both arches for leveling and alignment. The maxillary arch was leveled with continuous archwires, starting with 0.014-in nickel-titanium and working up to 0.019 × 0.025-in beta-titanium. The unilateral posterior crossbite was corrected during the leveling stage.
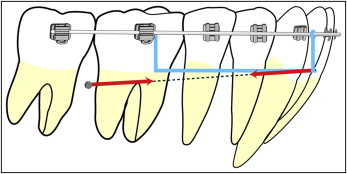
Two TSADs (OSAS, Tuttlingen, Germany) were placed in the mandibular arch after the leveling stage; one (diameter, 1.6 mm; length, 8.0 mm) in the interradicular bone between the mandibular right second premolar and first molar, and the other (diameter, 1.6 mm; length, 8.0 mm) in the interradicular bone between the mandibular left first and second molars. The right and left TSADs were placed in different interradicular areas to prevent root damage during installation. Bone quality in the mandible was good, and the TSADs were loaded immediately. A 0.016 × 0.022-in stainless steel archwire was used for distalization of the mandibular dentition. Elastic materials were applied from the neck of the TSADs to the ligature wires connected to the continuous archwire with hooks between the lateral incisors and canines for distalization of the mandibular dentition. To distalize the mandibular right quadrant further, a TSAD (diameter, 1.6 mm; length, 8.0 mm) was relocated between the mandibular right first and second molars, and a sliding jig was placed. This allowed additional distal movement in the mandibular right quadrant ( Figs 4 and 5 ). During the finishing stage, final detailing of the occlusion was accomplished with 0.016 × 0.022-in steel archwires in conjunction with posterior vertical elastics with Class III vectors.

Fixed retainers were attached on the maxillary and mandibular anterior teeth. Wraparound removable retainers were also delivered to secure the stability of both arches. Total treatment time for this patient was 30 months.
Treatment results
The posttreatment records showed that the treatment objectives were achieved. The facial photographs showed improved profile esthetics ( Fig 6 ). The anterior and unilateral posterior crossbites were corrected, acceptable overbite and overjet were achieved, and the dental midlines were aligned with the facial midline. Class I canine and molar relationships were established with a canine-protected occlusion ( Figs 6 and 7 ).