and Neil Agnihotri, DMD, MD
6.1 Definition and Prevalence of Dentofacial Deformities
The term dentofacial deformity refers to significant deviations from normal proportions of the maxillomandibular complex that also have a negative impact on the interrelationship of maxillary and mandibular dentition. The affected individual will have varied degrees of compromise in head and neck functions, including breathing, swallowing, speech articulation, chewing, lip closure/posture, and facial aesthetics. Effects on the temporomandibular joints (TMJs), the periodontium, and the teeth themselves may also occur. The presenting facial dysmorphology will in general have at least some effect on psychosocial health.
Surgery to reposition the jaws (orthognathic procedures) as part of a team approach for the correction of dentofacial deformities is recommended to manage the skeletal, dental, and soft tissue dysmorphology. Speech therapy, dental work, orthodontics, or surgical procedures alone are inadequate as isolated treatment modalities. For the experienced surgeon and orthodontist, the accurate diagnosis of a dentofacial deformity will usually be clear after the initial examination and review of standard records.1–7 The favorable correction through a combination of effective orthodontic alignment of the teeth combined with precise surgical repositioning of the jaw (or jaws) will be beneficial.
According to published epidemiologic studies in both the United States and the United Kingdom, it seems as though 5% of the population at a minimum will have a dentofacial deformity with a severe malocclusion requiring jaw surgery for full correction.8–10 It is likely that as many as 20% of individuals presenting for orthodontic assessment would ideally require not just orthodontics but jaw straightening procedures.8–10
6.2 Heredity, Developmental Influences, and Other Etiologic Factors
Knowing the etiology of a dentofacial deformity can be important in the fundamental understanding of how and when to treat the problem. Knowledge of any associated conditions (e.g., hemifacial micro-somia with cervical spine anomalies) is useful both to limit complications during treatment and for the family’s planning issues. With an understanding of the natural history of the condition, occasionally an opportunity to prevent or at least lessen the deformity may arise. Knowing how the muscles within the neck and face affect the development of a dentofacial deformity as well as head and neck function is also important.11,12 Factors that are known to both cause and alter dentofacial deformities can be subdivided as follows:
•Known syndromes and anomalies with dentofacial deformities;
–deficiencies of midline structures
–deficiencies/anomalies of neural crest origin
–clefting of the lip and palate
–achondroplasia
–premature suture closure of the cranial vault and skull base
–overgrowth syndrome or anomalies
•environmental and neuromotor effects on skeletal growth;
•muscle and soft tissue effects on skeletal growth;
•respiratory patterns and effects on skeletal growth;
•congenital myopathies and effects on skeletal growth;
•hereditary tendencies in the development of dentofacial deformities;
•effects of trauma on skeletal growth;
•effects of tumors/growths on skeletal growth.
6.3 Nasal Airway Considerations
At the time of orthognathic surgery, the surgeon has an opportunity to further contribute to the patient’s quality of life by simultaneously addressing long-standing breathing and sinus drainage difficulties that may coexist with the jaw deformity. Preexisting breathing difficulties may range from isolated symptomatic nasal airway obstruction to obstructive sleep apnea (OSA), and should not be overlooked.13–19 The frequency of combined nasal obstruction and maxillary deformity has been recognized and discussed in the published literature for more than 100 years.20
Nasal airway deformities (septal deviation, inferior turbinate enlargement, constricting pyriform apertures, and elevated nasal floor) commonly coexist with maxillary deformity.17 Favorable access to the nasal septum, inferior turbinates, pyriform apertures, and nasal floor to correct these airway obstructions/deformities is possible through the Le Fort I (down-fracture) osteotomy commonly used in orthognathic surgery.17 There is both animal experimental and human clinical research to support a link between oral (mouth) respiration, open-mouth posture, and the development of maxillomandibular disharmonies.11,12,19,20 Using rhesus monkeys as an experimental model, Harvold et al. completely blocked the nares in newborn monkeys.11,12 They observed consistent facial morphologic changes that gradually occur with growth in the presence of a constant open-mouth, protruding-tongue mandibular posture.11,12 In human children who have significant nasal obstruction, clinical observational studies document a similar chronic downward and backward posture of the mandible.19 Over several years, the affected children develop what we now recognize as a long face growth pattern.21 This is documented by a measurable vertically long and horizontal retrusive maxillomandibular dysmorphic growth.22
Posnick et al. documented that, when indicated, simultaneous management of the maxillary jaw deformity (Le Fort I osteotomy) and intranasal pathology (septoplasty, reduction of inferior turbinates, widening the nasal aperture, and recontouring of the nasal floor) is effective for the symptomatic relief of nasal airway obstruction.17 The complication rate for the intranasal procedures and Le Fort I osteotomy when completed simultaneously are minimal and not higher than expected when each procedure is carried out as an isolated event.17
6.4 Temporomandibular Disorders: Effects of Occlusion, Orthodontics, and Surgery
The prevalence of temporomandibular disorders (TMDs) in the general population as reported in the literature varies widely. It is estimated that an average of 32% of the population reports at least one symptom of TMD, and an average of 55% demonstrates at least one clinical sign.22–24 TMD includes various symptoms and signs of the TMJ, masticatory muscles, and related structures. This may include a spectrum of referred head and neck pain, joint noise (popping, clicking, crepitus), reduced or altered mandibular movement (muscle spasm or disk displacement with or without reduction), condylar head erosion, and pain on direct palpation of either the TMJ or the masticatory muscles. Occlusal factors (degrees of malocclusion) are often claimed to be associated with TMD.22–24 Interestingly, studies document that correcting a baseline jaw deformity with malocclusion through orthodontics and orthognathic surgery improves the presenting TMD in most treated patients, although a minority get worse.25
6.5 Psychosocial Considerations
Individuals presenting with a dentofacial deformity are not a monolithic group. They might arrive for evaluation in childhood, adolescence, or any time in adulthood. The etiology of the jaw deformity may be congenital, developmental, posttraumatic, or post-tumor resection with or without combined radiation therapy. A combination of orthodontic treatment and orthognathic (jaw straightening) surgery, often in conjunction with additional dental rehabilitation, may be required to correct the dysmorphology, improve head and neck function, enhance facial aesthetics, or restore the dentition.
The initial discussion concerning the need for orthognathic surgery may come as a shock to a patient and the family. They may have inaccurate preconceived ideas about the surgery and expected convalescence. The decision-making role of the parents and compliance (attitude) of the adolescent will also be important. Any dysfunctional family interactions at this moment of stress will also come into play. From the adolescent patient’s point of view, social interactions with his or her peers and concerns about the interpretation (by others) of any change in their appearance as well as their evolving self-image and identity will also carry weight in ways that are ongoing and somewhat unpredictable.26
6.6 Treatment Planning: Achieving Form and Function and the Importance of the Direct Visual Examination
Clinicians who are asked to correct a dentofacial deformity must direct their attention to both form and function. As Buckminster Fuller stated, rarely are the two objectives (i.e, form and function) divergent. In the achievement of a harmonious face, attention must also be directed toward the practical objectives of improving the upper airway, occlusion, speech, and deglutination. Facial aesthetic perfection is not a specific millimeter distance or degree of angulation but a visual impression at conversational distance in 3-dimensional life. At the same time, neither “divine proportions” as described by Euclid nor biologic realities (circulation requirements for wound healing) nor the individual’s personal preferences can be ignored in the process.27–29
At the time of the preoperative face-to-face planning examination of the patient by the operating surgeon, several evaluations will have already been carried out. Review of all relevant medical and dental records, photographic, radiographic, and dental studies and analysis should be fresh in mind. The patient is examined while upright and sitting in the natural head position (NHP). The teeth are in centric relation and the lips are relaxed. The NHP is considered the most rational, physiologic, and anatomic orientation for evaluating the face, jaws, and teeth.28 The patient is also viewed by the surgeon from different perspectives during facial animation. In a patient with a dentofacial deformity, a global overview of the head and neck should include consideration of:
1.Symmetry and harmony of the upper facial skeleton (i.e, cranial vault, orbits, nasofrontal process, and zygomatic arches).
2.Quality of the overlying soft tissue envelope of the head and neck (i.e, hypoplasia, hyperplasia, effects of trauma and aging); recognition of distortions versus intrinsic anomalies of the soft tissues.
3.The unique facial aesthetic units (i.e, external nose, external ears, periorbital soft tissues).
4.Symmetry and harmony of the lower facial skeleton (maxilla, mandible, chin).
5.History of cervical spine symptoms and signs and current neck range of motion.
6.History of TMJ symptoms and signs (TMDs) and current mandibular range of motion.
7.Dental rehabilitative needs including but not limited to orthodontic progress.
6.7 Detailed Maxillomandibular Surgical Planning
Confirming that the upper facial skeleton and the soft tissue envelope of the head and neck do not require surgical attention and that the neck and mandibular range of motion are intact without significant limitations is essential before focusing on detailed maxillomandibular surgical planning. Qualitative decisions concerning which components of the maxillomandibular skeleton are asymmetric or disproportionate, or both, and thus require surgical repositioning, will have already been discussed with the patient/family and other treating clinicians but are now reconfirmed.
Assuming that both the maxilla and mandible are part of the dentofacial deformity that requires surgical reconstruction (two-jaw surgery), quantitative decisions (to the millimeter) of the preferred aesthetic and desired functional repositioning of the upper jaw (at the time of Le Fort I osteotomy) must first be made. When thinking through the details of maxillary (surgical) repositioning, it is understood that the upper jaw (in two-jaw surgery) will serve as the platform on which the mandible is to be placed. The outcome for the lower jaw will then depend entirely on the new (surgical) position of the maxilla and the orthodontic alignment of the teeth. Concerning the maxilla, the surgeon makes eight basic quantitative (to the millimeter) decisions (assessments):
1.Assess current and preferred horizontal position of the maxillary incisor crown.
2.Assess current and preferred vertical position of the maxillary incisor crown.
3.Reconfirm advantage of (need for) segmentation of the maxilla to achieve preferred arch form.
4.Assess current and preferred A-point to B-point relationship of the jaws. Determine the need to alter the posterior (vertical) maxillary height (maxillary plane change) to achieve objectives (pitch orientation).
5.Assess the baseline chin morphology. Anticipate location of pogonion after jaw repositioning. Consider advantages of genioplasty and the preferred horizontal and vertical position of the chin.
6.Assess the baseline pyriform rims/floor of the nose/anterior nasal spine morphology. Anticipate their location after maxillary repositioning and any advantages of recontouring the pyriform rims/ floor of the nose/ANS to achieve objectives.
7.Assess the presence of any maxillary cant (role orientation) in comparison with the upper face. Determine the preferred upper jaw repositioning to correct a baseline cant.
8.Assess current and preferred position of the maxillary dental mid-line in comparison with the upper facial midline (yaw orientation). Anticipate any potential yaw effect of the new (surgical) maxillary position on the mandible and face.
6.8 Analytic Model Planning and Splint Construction
Orthognathic reconstruction, unlike most surgical procedures, involves precise preoperative dental and aesthetic preparation. The surgeon carries out a detailed face-to-face examination combined with a facial photographic and radiographic analysis. Immediate presurgical records include current and accurate dental impressions of the maxilla and mandibule, bite registration in centric relation, face bow registration for transfer to a semiadjustable articulator, and specific facial measurements. The dental models are placed on a semiadjustable articulator using the face bow and centric relation bite registrations. This information is used for further analysis and completion of the model planning. Acrylic splints are fabricated and used intraoperatively to further ensure the reliable execution of predetermined facial aesthetic and functional objectives. Although clinical decisions concerning the preferred aesthetic positioning of the jaws in the operating room remains both an art and a science, the technical aspect of model planning should be precise and consistent. Model planning with the use of prefabricated splints continues to be the standard of care for bimaxillary and segmental maxillary osteotomies.30
6.9 The Basic Orthognathic Procedures
Maxillofacial surgeons and orthodontists are the primary clinicians caring for individuals with jaw deformities/malocclusion and the associated facial dysmorphology. When orthognathic reconstruction is indicated, the surgeon generally uses a limited number of surgical techniques to facilitate the 3-dimensional repositioning of the skeletal units (maxilla, mandible, and chin) to achieve improvements in head and neck function and to enhance facial aesthetics.31,32 By and large, these options include the Le Fort I (type) osteotomy with or without segmentation of the down-fractured maxilla, sagittal split osteotomies of the ramus of the mandible, and an oblique osteotomy of the chin. These three basic procedures and fixation techniques were described by Hugo Obwegeser and Hans Luhr respectively and have evolved gradually to their current usage.31
By understanding details for the safe execution of maxillary (Le Fort I), mandibular (sagittal splitting of the ramus), and chin (osteoplastic genioplasty) osteotomies, each skeletal unit may be precisely repositioned during one operation.31,32 Other simultaneous adjunctive procedures, such as septoplasty, reduction of inferior turbinates, recontouring of the pyriform rims, removal of wisdom teeth, or neck soft tissue procedure (i.e, cervical flap elevation, neck deflattening, and platysma muscle placation), are routinely and safely performed when indicated to improve head and neck function (e.g., occlusion, chewing, speech articulation, swallowing, breathing, lip closure) and to achieve the desired facial refinements.17,31,33,34 Special circumstances and unusual anatomy require variations in these techniques, but developing a standard surgical approach limits morbidity and increases the efficiency of treatment.29,35
6.10 Complications Associated with Orthognathic Surgery
An unavoidable fact of clinical practice is that no matter how accurate the diagnosis and how meticulous the surgeon, complications will occur after orthognathic procedures.29,35,36 By understanding the nature of the presenting dentofacial deformity, the patient-specific risk factors, any associated conditions/malformations, unique psychosocial aspects, and any current head and neck dysfunction, complications can be minimized. The probability of perioperative problems can be understood and should be presented to the patient and family for consideration before treatment. In addition to executing precise orthognathic procedures, achieving informed consent and accomplishing patient education are also essential components of comprehensive care.
6.11 Malocclusion After Orthodontics and Orthognathic Surgery
There are inherent limitations to both orthodontic tooth movement and surgical repositioning of the jaws (and jaw segments) imposed by the alveolar bone and the soft tissue envelope surrounding the facial skeleton.29,35 Malocclusion after orthognathic surgery and orthodontic treatment is one potential adverse consequence if the biologic boundaries are not respected. This includes mechanical/technical aspects of the tooth and bone repositioning, initial healing requirements, and difficulties associated with a long-term stability of the mechanically relocated teeth, jaws, and jaw segments. Adhering to basic biomechanical principles and with clinical experience, the frequent patterns of dentofacial deformities with malocclusion can be safely and reliably corrected and maintained in most cases. The vector changes of the jaws, jaw segments, and teeth that are more prone to relapse are known, and so are many of their reasons.37,38 Each orthodontic tooth movement and maxillary and/or mandibular osteotomy and proposed vector change has unique nuances that may require special considerations (e.g., flap design, osteotomy design, flap mobilization, interpositional grafting needs, fixation requirements, splint management and retention options) to achieve and maintain the results. These and other considerations should be incorporated into the treatment plan from the outset.
6.12 Common Patterns of Dentofacial Deformities
6.12.1 Primary mandibular deficiency growth pattern with or without arch-width discrepancy
Mandibular deficiency is the most prevalent form of dentofacial deformity (Case study: Patient 1; Figure 6.1).10 It is more common in whites than in blacks or Asians, suggesting that a hereditary component is a predominant part of the etiology. Mandibular deficiency frequently presents with a degree of maxillary constriction that will also require correction.39 Functional aspects may include articulation errors in speech and swallowing difficulties resulting from the Angle class II excess overjet malocclusion. Difficulties with chewing during the day and upper airway obstruction at night (retropositioned tongue) also occur.13,14 A higher incidence of TMD resulting from the mandibular deficiency class II malocclusion is also common.25 Clinical characteristics include a curled and everted lower lip with an accentuated labiomental fold. The angles of the mandible tend to be relatively square. There is a retruded weak chin with a convex profile. The deficient mandible gives the illusion of a large nose. There is a short chin-to-neck length and angle. This patient’s clinical concerns tend to center on the unattractive lower lip contours and lack of prominence of the chin (weak profile).39–41
Case Study: Patient 1
A 33-year-old woman presented to the surgeon (J.C.P.) for evaluation of a long-standing dentofacial deformity with malocclusion. By the early teenage years, it was known that she had a jaw deformity characterized by mandibular deficiency with a class II excess overjet malocclusion. She was treated by an orthodontist with growth modification techniques (twin block) but without successful “stimulation” of the mandible. She then underwent camouflage orthodontics, including maxillary bicuspid extractions with retraction of the anterior dentition and proclination of the mandibular incisors to improve the overjet relationship. Despite several years of treatment, a molar class II excess overjet malocclusion remained.
She presented to an orthodontist for further correction of the occlusion and in the hope of achieving an improved profile. She was referred for surgical evaluation (J.C.P.) with a request for a “stronger profile” and relief of the double chin. Jaw, chin, and neck surgery in combination with lower bicuspid extractions and orthodontic decompensation was offered and accepted as a way to alleviate the symptoms and signs, and to enhance facial appearance. The surgery proposed and carried out included:
•bilateral sagittal split ramus osteotomies of the mandible,
•oblique osteotomy of the chin,
•neck liposuction.
The articulated dental casts of the model surgery planning indicate the vector changes planned and carried out:
•mandibular movements
–11-mm advancement at the incisors
•chin movements
–horizontal advancement
Operative time was approximately 1.5 hours. No blood replacement was required. The patient was extubated in the operating room at the end of surgery. She remained in the hospital for 1 night and was then discharged to the care of her husband. At the 2-week postoperative interval, she returned to work. At 5 weeks after surgery, she returned to a normal diet, physical activities (sports and gym), and her orthodontist’s care. After orthodontic detailing, the appliances were removed (7 months postoperatively). She is shown before and 1 year after completion of treatment (Figure 6.1).
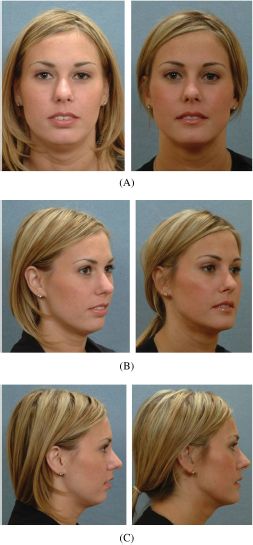
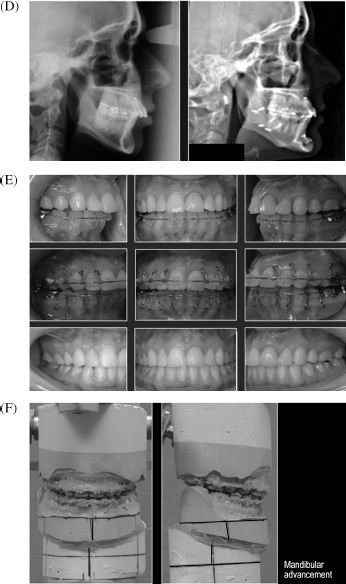
Figure 6.1. Patient 1. (A) Frontal facial views in repose before and after treatment. (B) Oblique facial views before and after treatment. (C) Profile facial views before and after treatment. (D) Lateral cephalometric views before and after treatment. (E) Occlusal views before redo orthodontics, immediately presurgery, and 1 year after completion of treatment. (F) Articulated dental casts of model surgery planning.
When a combined orthodontic and surgical approach is agreed to, the orthodontist removes dental compensations. Extraction of mandibular first bicuspids to create space for the correction of anterior crowding and avoidance of “flaring” (i.e, incisor procumbency) is frequently required. In addition to mandibular advancement, maxillary surgery is often required primarily to correct arch-width discrepancies.39 Through the Le Fort I osteotomy, improvement in the upper lip–upper tooth relationship by alteration of the vertical height can be carried out simultaneously. Any deficiencies in the horizontal position of the maxilla can also be corrected. Intranasal procedures (septoplasty, inferior turbinate reduction) can be accomplished through the Le Fort I osteotomy if clinically indicated.17 An oblique osteotomy of the chin with horizontal advancement is generally helpful to further improve profile aesthetics and lip position.42
6.12.2 Asymmetric mandibular excess growth pattern
The term asymmetric mandibular excess is useful for name recognition but falls short of explaining the cause and effects of this common pattern of jaw deformity.43,44 It results in an uneven Angle class III malocclusion. The overall effect on mandibular morphology; the secondary deformities that it causes on the maxilla, chin, and teeth; and the distortions that are visually observed in the overlying soft tissue envelope are dependent on multiple factors. They include the intensity of the mandibular hyperactivity; the patient’s age when the abnormal bone growth begins; any underlying hereditary dentofacial deformity tendency; and any treatment previously rendered (orthodontic, dental, or surgical) before the patient arrives to the maxillofacial surgeon for evaluation.
Obwegeser believes that this dentofacial deformity is caused by two different growth regulators.44 The first one causes hemimandibular hyperplasia. This is a more rare form and is clinically characterized by an increasing volume of all parts of the affected side of the mandible but without resulting in a deviation of the midline of the chin to the opposite side. The second growth regulator causes the more common hemimandibular elongation. This dentofacial deformity is characterized by an elongation of all parts of the affected side of the mandible, often with widening at the gonial angle and with clear displacement of the midline of the chin and shifting of the mandibular midline to the opposite side of the face. In patients with asymmetric mandibular excess, skeletal scintigraphy (technetium Tc 99m bone scan) is a useful method to assess the state of residual mandibular excess growth.45
The perioperative orthodontic treatment should achieve the correct positioning of the teeth into the respective basal bone in each jaw. At the completion of presurgical orthodontic treatment, the position of the teeth and the alveolar bone should not hamper the ability of the surgeon to achieve maximum mirror-image skeletal symmetry, Euclidean facial proportions, and a preferred long-term stable condition.1–7 In general, the presenting maxillomandibular deformities are best managed with classic orthognathic techniques carried out at skeletal maturity to improve both head and neck function and to enhance facial aesthetics.31,45,46 This will include, at a minimum, sagittal split ramus osteotomies of the mandible. In general, the maxilla is secondarily deformed and will benefit from a Le Fort I osteotomy with 3-dimensional repositioning. An oblique osteotomy of the chin will likely further improve facial symmetry. The need for a high condylectomy remains limited and is considered only in the presence of significant, progressive, active disease at the time of diagnosis.44
6.12.3 Long face growth pattern: Maxillary vertical excess with mandibular deformity
The prevalence of long face growth patterns within a dentofacial deformity referral pattern is thought to be approximately 20 to 25% (Case study: Patient 2; Figures 6.2 and 6.3).10 The diagnostic criteria for a long face growth pattern includes an excess anterior facial height (primarily with elongation of the lower third) leading to disproportion between facial height and width.21,46,47 This generally results from an excessive eruption of the posterior maxillary dentition. The increased lower facial height causes the mandible to rotate downward and backward. The excessive lower anterior facial height makes any baseline mandibular horizontal deficiency seem worse and any true mandibular excess seem better. Dental compensations result, and an anterior open bite is generally present. There is wide lip separation at rest, resulting in mentalis strain in attempts to achieve lip closure. Consistent radiographic findings in the long face condition include21,46,47:
Case Study: Patient 2
A recent college graduate, aged 21 years, presented for evaluation of a long-standing dentofacial deformity with malocclusion and chronic obstructive nasal breathing. Since early childhood, she was known to have had difficulty breathing through her nose. Through her teenage years, a long face deformity with anterior open bite, significant overjet, and class II malocclusion developed. This was treated with camouflage orthodontics for 6 years (age 9–15), and included four bicuspid extractions in attempts to “close the open bite.” No attention was paid to either the facial disproportion or her difficulty breathing through the nose. After removal of the orthodontic brackets and despite the use of retainers, the dental crowding and the anterior open bite recurred.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


