Figure 16.1. Common patterns (and incidences) of facial nerve branching, illustrated. Reprinted with permission from the Journal of the American College of Surgeons, formerly Surgery Gynecology & Obstetrics (Ref. 4).
The frontal and marginal mandibular branches usually are minimally interconnected with the other facial nerve branches, resulting in major sequelae when injured. The frontal nerve is composed of an average of 2.8 branches that become more superficial as they enter the temporal region superior to the zygomatic arch, traveling under the temporoparietal fascia.5 The course of the frontal nerve can be approximated by tracing a line from 5 mm below the tragus to 15 mm above the lateral aspect of the eyebrow.6 The marginal mandibular nerve consists of an average of 2.3 branches and is located within the superficial layer of the deep cervical fascia under the platysma. The marginal mandibular nerve lies superficial to the facial artery and vein. Posterior to the facial vessels, it travels below the inferior border of the mandible in 19% of the population. Anterior to the facial vessels, it is located above the inferior border of the mandible.7
The facial nerve innervates the facial musculature used for facial movement and expression (emotion, psychosocial functioning, and social interaction), eye function and protection (blinking, tear production and distribution, and lacrimal pumping action), nasal airway patency, and oral competence (speaking, eating, and drinking) (Figure 16.2).
16.3 Facial Musculature
The muscles of facial expression innervated by the different branches of the facial nerve consist of multiple paired muscles and the single orbicularis oris muscle (Figure 16.3). The mentalis, levator anguli oris, and buccinator are the deepest of the facial muscles and receive innervation superficially. The remaining facial muscles receive their innervation along their deep surfaces. The frontalis, orbicularis oculi, zygomaticus major, orbicularis oris, and depressor labii inferioris have key roles in facial animation. Knowledge of their function and their respective neural innervation helps determine the affected facial nerve branch (Table 16.1). The modiolus represents the point of common attachment for the zygomaticus major and minor, orbicularis oris, buccinator, risorius, levator anguli oris, and depressor anguli oris. It is often considered an anchor point when performing reanimation or static elevation procedures.
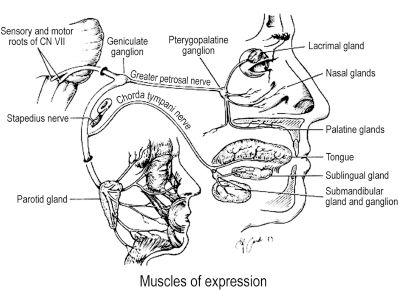
Figure 16.2. Facial nerve innervation and functions, illustrated. Reprinted with permission from Elsevier (Jackson CG, et al. The facial nerve: current trends in diagnosis, treatment, and rehabilitation. Med Clin North Am 1999;83:179–195). Copyright © 1999 Elsevier.
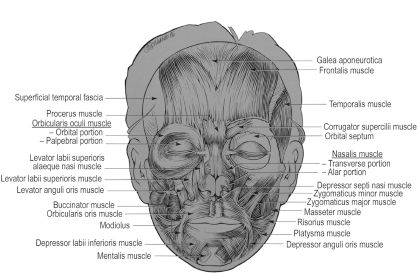
Figure 16.3. Muscles of facial expression. Reprinted with permission from The McGraw-Hill Companies (Salasche SJ, Bernstein C, Senkarik M. Surgical Anatomy of the Skin. Chapter 7. Norwalk, CT: Appleton & Lange; 1988:69).
Table 16.1. Innervation and Actions of Facial Mimetic Muscles.
| Branch of CN VII |
Facial muscle |
Actions |
|
Temporal |
Frontalis Corrugator supercilii |
Elevates eyebrow Pulls eyebrow medially and downward |
|
|
Procerus |
Pulls medial eyebrow downward |
|
Temporal and zygomatic |
Orbicularis oculi |
Closes eyelids and contracts skin around eye |
|
Zygomatic and buccal |
Zygomaticus major |
Elevates corner of mouth |
|
Buccal |
Zygomaticus minor |
Elevates upper lip |
|
|
Levator labii superioris |
Elevates upper lip and mid-portion nasolabial fold |
|
|
Levator labii superioris alaeque nasi |
Elevates medial nasolabial fold and nasal ala |
|
|
Risorius |
Aids smile with lateral pull |
|
|
Buccinator |
Pulls corner of mouth backward and compresses cheek |
|
|
Levator anguli oris |
Pulls angles of mouth upward and toward midline |
|
|
Orbicularis oris |
Closes and compresses lips |
|
|
Nasalis, dilator naris |
Flares nostrils |
|
|
Nasalis, compressor naris |
Compresses nostrils |
|
Buccal and marginal mandibular |
Depressor anguli oris |
Pulls corners of mouth downward |
|
|
Depressor labii inferioris |
Pulls lower lip downward |
|
Marginal mandibular |
Mentalis |
Pulls skin of chin upward |
|
Cervical |
Platysma |
Pulls down corners of mouth |
The action and specific vector orientation created by the facial musculature must be analyzed in the non-symptomatic face before attempting reconstruction on the affected side.
•Lip elevator vector:
a.Zygomaticus major and minor muscles: 45° superior lateral
b.Levator anguli oris: superior and medial
c.Levator labii superioris: superior and lateral
d.Levator labii superioris nasi alaeque: superior
•Lip depressor vector:
a.Depressor labii inferioris: inferior and lateral with eversion of the vermilion
b.Depressor anguli oris: depresses the angle of the mouth
The mentalis muscle is not a lip depressor; it elevates the lip indirectly since it arises from the anterior mandible and inserts into the skin of the chin in a downward direction.
16.4 Causes of Facial Paralysis
Approximately 127,000 cases of permanent facial paralysis occur annually.8 The differential diagnosis of facial paralysis constitutes a myriad of medical conditions. Etiologies may be classified in the following categories: idiopathic, traumatic, neoplastic, infectious, congenital/genetic/metabolic, neurologic, and toxic (Table 16.2).
16.4.1 Idiopathic (Bell’s palsy)
The most common cause of facial paralysis is Bell’s palsy with an annual incidence of 11 to 40/100,000.9,10 It is usually unilateral, can be complete or partial, and accounts for 85% of all cases of facial paralysis. Bell’s palsy is primarily a diagnosis of exclusion with a proposed viral and inflammatory etiology.11 The resulting edema of the nerve within the fallopian canal (labyrinthine segment), the canal with the smallest diameter, causes nerve compression and disruption of the neural microcirculation. The incidence is increased during pregnancy (last trimester) and in patients suffering from diabetes mellitus.12 It manifests as a unilateral palsy and may be associated with other CN neuropathies.
Table 16.2. Causes of Facial Paralysis.
|
Causes |
Conditions |
|
Idiopathic |
Bell’s palsy, sarcoidosis, Melkersson–Rosenthal syndrome, systemic lupus erythematosus, multiple sclerosis, temporal arteritis, eosinophilic granuloma, amyloidosis, immunization |
|
Infection |
Otitis media, herpes simplex, varicella-zoster, syphilis, poliomyelitis, botulism, mastoiditis, coxsackievirus, encephalitis, tetanus, diphtheria, HIV/AIDS, tuberculosis, meningitis, Lyme disease, cryptococcal meningitis, mononucleosis, leprosy, pregnancy |
|
Neoplastic |
Schwannoma, teratoma, parotid tumor, cholesteatoma, glomus jugular tumors, neurofibromas (von Recklinghausen’s disease), germ cell tumors, meningioma, hemangioma, sarcoma and carcinoma (metastasis) |
|
Congenital/genetic/ metabolic |
Möbius syndrome, craniofacial (hemifacial) microsomia, diabetes mellitus, pregnancy, hyperthyroidism, hypothyroidism |
|
Neurologic |
Guillain-Barré syndrome, pontine glioma, opercular syndrome, Wernicke–Korsakoff syndrome, pseudotumor cerebri, cerebrovascular accident (lacunar infarct), myasthenia gravis |
|
Trauma |
Traumatic delivery, forceps delivery, head injury, facial skeleton and soft-tissue injuries, barotrauma (scuba diving), surgery complication, anesthetic nerve block, postembolization |
|
Toxins |
Thalidomide, interferon, linezolid, ethylene glycol, ethanol |
HIV/AIDS = human immunodeficiency virus/acquired immune deficiency syndrome. Conditions shown in bold are frequently associated with bilateral facial nerve palsy.22,23
The following signs and symptoms exclude a diagnosis of Bell’s palsy13:
•simultaneous bilateral facial palsy
•slowly progressive unilateral facial weakness beyond 3 weeks
•slowly progressive unilateral facial weakness associated with facial hyperkinesis
•no improvement in facial nerve function within 6 months after an abrupt onset of palsy
•ipsilateral lateral rectus palsy (CN VI — abducens nerves)
The prognosis is usually good, with 86% of patients recovering within 3 weeks. Therefore, diagnostic testing is deferred until that time.10 The recurrence risk of Bell’s palsy has been reported to be as high as 10%, with women carrying a higher risk.14
16.4.2 Traumatic
The second most common cause of facial paralysis is trauma, which can be further divided into accidental and surgical causes. Accidental trauma includes temporal bone fracture, sharp injuries, avulsion, and burns. Head injury may result in a temporal bone fracture that usually affects the facial nerve within the labyrinthine segment. The junction of the labyrinthine and tympanic segments forms an acute angle and is therefore at risk for shearing injury. Computed tomography (CT) is helpful in localizing the injury, and immediate exploration is recommended in the setting of acute onset of paralysis.
Penetrating sharp injuries have a more favorable prognosis than crush injury. Injuries located anterior to an imaginary vertical line at the lateral canthus do not require surgical repair because of the extensive arborization between the different facial nerve branches, especially the zygomaticobuccal branches. The most distal nerve ends are also very difficult to identify. If the injury is located posterior to this imaginary vertical line at the lateral canthus, immediate repair should be done within 72 h. In cases of infection or inadequate soft-tissue coverage, identification of the nerve ends should be attempted for delayed repair. Facial nerve stimulation resulting in movement of the facial muscles is possible only within 72 h post injury. Repair of the frontal and mandibular branches should be attempted regardless of the location of the injury because of the morbidity associated with injury to these branches.
Trauma during delivery occurs at an incidence of 1.8 per 1,000 births annually; 91% are associated with forceps delivery, and 89% have complete recovery.15 Surgical causes of CN VII paralysis may be secondary to resection of a tumor at the cerebellopontine angle, such as a schwannoma (acoustic neuroma). Parotid gland manipulation secondary to a superficial parotidectomy often results in a transient neuropraxia that improves over several months.
16.4.3 Neoplastic
Presentation may be quite variable depending on the tumor; however, a prolonged, relapsing, or slowly progressive onset of facial paralysis suggests a neoplasm.16 Hearing loss, either conductive or sensorineural, is often an associated symptom. A schwannoma is the most common neoplasm of the facial nerve. The index of suspicion for a neoplastic process should be high in cases of slowly progressive facial paralysis lasting more than 3 weeks, abrupt onset with no return of function within 6 months, or facial weakness associated with hyperkinesis (twitching).13 Imaging studies such as CT or magnetic resonance imaging (MRI) are mandatory if suggestive signs or symptoms are present.
16.4.4 Infectious
Varicella-zoster presenting as Ramsay Hunt syndrome (herpes zoster oticus) is one of the more common causes in this category. It is generally severe. Signs and symptoms include peripheral facial paralysis, ear pain, vesicular rash in the external auditory canal, and possible tinnitus and hearing loss. Treatment consists of steroid and antiviral therapy.
Lyme disease (caused by Borrelia burgdorferi) presents with cutaneous (erythema chronicum migrans), musculoskeletal, cardiovascular, and neurologic symptoms after a tick bite. Bilateral facial paralysis is common and often resolves within 2 months with antibiotic therapy consisting of doxycycline or erythromycin.
16.4.5 Congenital/genetic/metabolic
Craniofacial (hemifacial) microsomia, which is a first and second branchial arch disorder, is the most common congenital cause of unilateral paralysis. It may also be present in Goldenhar’s syndrome, which is a variant of craniofacial microsomia associated with epibulbar dermoids and vertebral anomalies.
Congenital unilateral lower lip palsy (also known as asymmetric crying facies) is found in 1 in 160 births and involves the depressor angularis oris.17,18 There is isolated paralysis of the marginal mandibular branch of the facial nerve (Figure 16.4). These patients may be associated with a 22q11.2 deletion and have cardiac anomalies.19 Genetic/chromosomal workup should be considered in patients with this disorder.
Möbius syndrome is a rare congenital disorder with a multifactorial pathogenesis that includes genetic, vascular, and toxic causes. It occurs in 0.002% of births.20 It is characterized by unilateral or bilateral developmental impairment of CN VI and VII. It may also involve CN V, IX, and XII and, less frequently, CN III, IV, and VIII. Other abnormalities associated with this syndrome include orofacial malformations (epicanthal folds, micrognathia, ear anomalies), limb malformations (brachydactyly, syndactyly, talipes equinovarus), musculoskeletal defects (absence of pectoralis and trapezius muscles), and mental retardation (Figure 16.5). Feeding and respiratory problems are frequent in the newborns due to lack of respiratory drive, insufficient sucking, uncoordinated swallowing, and regurgitation.
Treatment of Möbius syndrome is very challenging in these masklike faces. It usually consists of a dynamic reconstruction with free tissue transfer, such as a bilateral gracilis muscle with masseteric branch innervation. Speech may be improved with direct tongue neu-rotization with CN VII or CN XI used in combination with a sural nerve graft.21
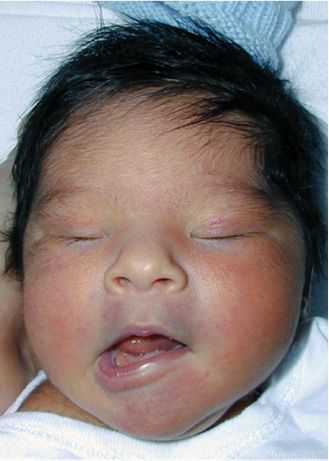
Figure 16.4. Photograph of an infant who has congenital unilateral lower lip palsy, exhibiting paralysis of the left marginal mandibular branch of the facial nerve.
16.5 Evaluation and Treatment of Acute Facial Paralysis
The goal in evaluating a patient afflicted with acute facial paralysis is to identify the site of the lesion, the degree of dysfunction and, ideally, the cause. The history and physical examination are of paramount importance and should include a detailed history of the onset, progress, and associated signs and symptoms of the CN VII dysfunction as well as a careful head and neck examination. The House–Brackmann classification provides an overall facial-function grading scale with measurements of range of motion of the eyebrows and a quantification of the ability to close the eye and to lateralize the oral commissure (Table 16.3).24 Several new scales such as the Sunnybrook, Yangihara, and Sydney have been introduced with various degrees of objectivity. However, the House–Brackmann grading scale remains to be the gold standard.
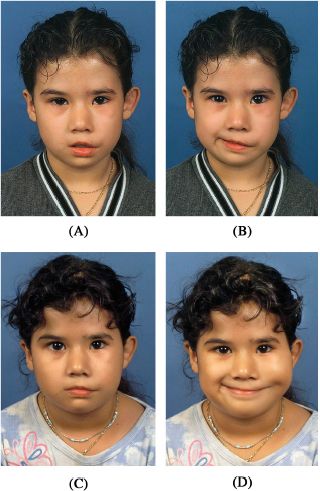
Figure 16.5. Photographs of a 6-year-old girl with Möbius syndrome associated with congenital bilateral abducens and a left facial paralysis in repose (A), and in an attempted smile (B). Photographs taken 1 year after she underwent free gracilis muscle transfer to the motor nerve of the masseter at rest (C), and smiling (D).
Radiologic imaging consisting of MRI and CT may be helpful in determining the location of a disease process affecting the facial nerve. Gadolinium-enhanced MRI is ideal for detecting soft-tissue inflammation and tumors. CT provides detailed anatomy of the temporal bone including the course of the facial nerve, which can be particularly useful after trauma.
Table 16.3. The House–Brackmann Classification.
|
Grade |
Description |
Characteristics |
|
I |
Normal |
Normal functioning in all branches of the facial nerves |
|
II |
Slight |
Gross: Slight weakness on close inspection, slight synkinesis At rest: Normal tone and symmetry Motion Forehead: Moderate to good function Eye: Complete closure with minimal effort Mouth: Slight asymmetry |
|
III |
Moderate |
Gross: Clear facial asymmetry but not complete or disfiguring, synkinesis or mild hemifacial muscular spasms noticeable in the area of the facial nerve At rest: Normal tone and symmetry Motion Forehead: Slight to moderate movement Eye: Complete closure with moderate effort Mouth: Slight weakness with maximal effort |
|
IV |
Moderately severe |
Gross: Total facial asymmetry that is disfiguring with obvious facial weakness At rest: Normal tone and symmetry Motion Forehead: No movement Eye: Incomplete closure Mouth: Asymmetric weakness with maximal effort |
|
V |
Severe |
Gross: Minimal, barely perceptible movement At rest: Asymmetric facial appearance Motion Forehead: No movement Eye: Incomplete closure Mouth: Slight, barely perceptible movement |
|
VI |
Total |
No facial function |
Modified with permission from Sage (Ref. 24).
Numerous electrodiagnostic tools measuring the neurophysiologic status of the facial nerve itself are available to help in the diagnosis, treatment, and prognosis of facial paralysis.25 The most commonly used tests include the following:
•Nerve excitability test (NET) is a subjective minimal stimulation test measuring the current threshold required to elicit minimal muscle contraction on the normal side compared with that of the affected side. An abnormal test result is defined as a difference of 3.0 to 3.5 milliamperes between the two sides of the face.
•Maximal stimulation test (MST) is similar to NET but uses maximal stimulation and is therefore painful and subjective. An abnormal test result consists of any difference in facial movement between the two sides of the face. Both NET and MST rely on percutaneous stimulation of the facial nerve, are subjective, and do not show abnormalities until 72 h after nerve degeneration.
•Electroneuronography (ENOG) records the compound action potential after a supramaximal electrical stimulation of the facial nerve. The percentage of nerve fiber degeneration (amplitude of the compound action potential) compared with the non-paralyzed face is helpful in predicting the prognosis of the facial paralysis and selecting an appropriate treatment plan.26 ENOG is an objective test, and is the most accurate reproducible test to determine the prognosis for return of facial nerve function, although it is expensive and at times impractical.27 A current is delivered percutaneously to the stylomastoid foramen, and the amplitude of evoked compound muscle action potentials (CMAPs) is measured from electrodes on the nasolabial fold. Maximal muscle response is elicited on each side regardless of the electrical current required. Results are analyzed, and in most cases of Bell’s palsy, there is no further decline in CMAP by the 10th day. A 95% decrease in CMAP on the affected side, compared with the normal side, showed 50% of patients had an unsatisfactory return of facial nerve function.28 As such, the threshold for recommending surgical decompression has been a 90% decrease in CMAP within the first 2 weeks postparalysis.
•Electromyography (EMG) evaluates muscle activity and provides an approximate measure of the intensity of denervation when performed early in the paralysis. Fibrillation potentials are observed in the denervated muscle, polyphasic potentials are found in muscle undergoing reinnervation, and complete electrical silence is noted in denervated muscle with significant fibrosis. This test should be performed at least 3 weeks from the onset of paralysis to be reliable.29
16.6 Management of Acute Facial Paralysis
Most patients with Bell’s palsy recover to House–Brackmann I or II function grade without intervention. However, treatment with prednisolone for 10 days within 72 h of symptom onset significantly improves recovery compared with placebo.30 Patients with Bell’s palsy are commonly treated with corticosteroids in the acute setting despite controversy regarding their effectiveness. Another recommended protocol suggests high-dose prednisone, starting with 60 mg/day for the first 5 days and tapered over 10 days.31 Should the paralysis become progressive and complete or if otalgia occurs, recurs, or worsens, a second 10-day course is recommended. Risk factors for incomplete recovery are complete facial weakness, non-ear pain, and hypertension.10 Some patients develop disabling sequelae such as synkinesis or severe facial spasm despite targeted medical treatment.
Surgical decompression for Bell’s palsy is still highly controversial. Facial nerve decompression from the middle cranial fossa through the tympanic segment performed within 12 days of onset has demonstrated modest but statistically significant improvement in severe cases with unfavorable electrodiagnostic profiles.32 The procedure involves removal of the bony covering of the fallopian canal with or without incision of the periosteum/epineurium. The decision for decompression usually depends on data derived from ENOG. This is a time-consuming test, requiring daily evaluation for the first 10 days postparalysis. If the patient cannot comply with daily testing or if a surgeon is unwilling to decompress should the test become positive, ENOG may be of little value.
Patients with acute facial paralysis often experience problems with dry eyes, speech, and oral competence. Medical management of ocular symptoms in facial paralysis includes frequent use of artificial tears and lubricating ophthalmic ointment to prevent and treat exposure keratopathy. Other options include eyelid taping (especially at bedtime), moisture chamber goggles, and patches. Speech therapy can help patients cope with drooling and speech difficulties.
16.6.1 Repair of facial nerve injuries
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


