PART I: TERMINOLOGY
AND SURGICAL TECHNIQUES
5
5.1 Introduction
Orthognathic surgery involves osteotomy, mobilization, and fixation of the maxilla, mandible, and/or chin in an effort to achieve a more anatomic relationship between the upper and lower jaws. The ultimate goal is not only to establish a normal dental relationship, but also, and perhaps more importantly, to achieve an esthetically pleasing facial soft tissue relationship. The diagnosis and treatment planning of all dentofacial deformities is complex and requires thorough knowledge of basic dental occlusion, cephalometric and facial analysis, and orthodontic principles.
5.2 Dental Analysis
Dental anatomy can be confusing initially as it seems to contradict with traditional anatomic terminology, especially with respect to the terms “proximal” and “distal.” In dental anatomy, because the teeth are aligned in arches, the dental midline becomes the point of reference. Think of the dental arch stretched into a straight line to better understand the terminology. The back portion of a tooth would be distal (away from the midline), and the anterior portion of a fractured mandible would be termed the “distal segment.”
•Dental terminology (Figure 5.1).
–Mesial: Toward the midline.
–Distal: Away from the midline.
–Lingual: On the tongue side.
–Palatal: On the palatal side.
–Buccal: On the cheek side.
•Occlusion (how the teeth come together) (Figure 5.2).
–Overjet: The horizontal overlap of the upper and lower incisors (normally 2 mm).
–Overbite: The vertical overlap of the upper and lower incisors (normally 3 mm).
–Openbite: Negative overbite.
–Crossbite: The buccal surfaces of the maxillary teeth are lingual to the buccal surfaces of the mandibular teeth.
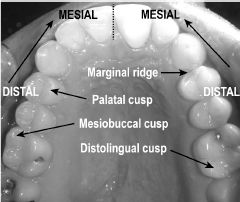
Figure 5.1.
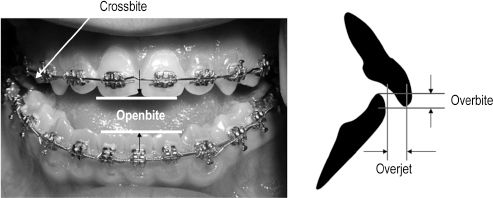
Figure 5.2.
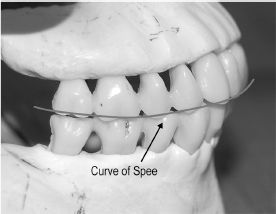
Figure 5.3.
–Curve of Spee: The natural curvature of the mandibular occlusal plane from incisor to molar teeth in the sagittal plane (Figure 5.3).
–Curve of Wilson: The natural curvature of the occlusal plane of the molar and premolar teeth in the coronal plane (Figure 5.4).
–Sphere of Monson: The 3-dimensional construct of the curves of Spee and Wilson (Figure 5.4).
 Note: These terms have significance when orthodontic leveling of the arches is performed with arch wires; the curve of Spee is typically leveled (made flat) before orthognathic surgery.
Note: These terms have significance when orthodontic leveling of the arches is performed with arch wires; the curve of Spee is typically leveled (made flat) before orthognathic surgery.
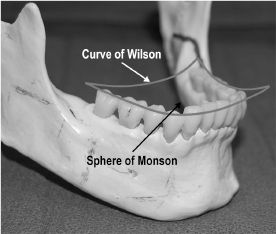
Figure 5.4.
•Described by Edward Angle, MD, DDS, in 1898, the Angle Classification of Occlusion describes the relationship of the upper first molar to the lower first molar (Figure 5.5):
–Class 1: The mesiobuccal cusp of the maxillary first molar is in the buccal groove of the lower first molar.
–Class 2: The distobuccal cusp of the maxillary first molar is in the buccal groove of the lower first molar.
 Division 1: The maxillary incisors are proclined.
Division 1: The maxillary incisors are proclined.
 Division 2: The maxillary central incisors are retroclined and the lateral incisors are proclined.
Division 2: The maxillary central incisors are retroclined and the lateral incisors are proclined.
–Class 3: The mesiobuccal cusp of the maxillary first molar is in the distobuccal groove of the lower first molar:
 Note: Keep in mind that the same patient may have different molar relationships on each side of the arch.
Note: Keep in mind that the same patient may have different molar relationships on each side of the arch.
•Bolton analysis: This is a method to determine tooth size discrepancies between upper and lower arches (Figure 5.6). The added width of the anterior six teeth of the upper arch is slightly longer than the added width of the anterior six teeth of the lower arch by a constant ratio. If this ratio deviates, there is a tooth size discrepancy; for example, a patient with peg (narrow) lateral incisors has an anterior upper arch width that is too small relative to the lower anterior teeth. This has significance when coordinating upper and lower arches for surgery. Spacing or filing of teeth (stripping) by the orthodontist might be necessary or segmental osteotomies might be needed at surgery.
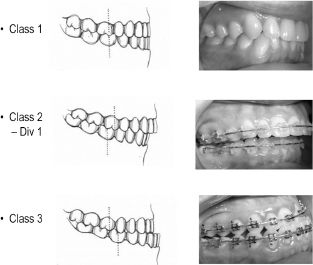
Figure 5.5.

Figure 5.6. Segmental osteotomies between the lateral incisor and canine on both sides to increase upper arch length relative to the lower arch (Bolton discrepancy).
•Dental compensations: Patients with skeletal disharmonies before surgical/orthodontic treatment have teeth that are abnormally angulated or positioned to make up for malaligned skeletal structures. The teeth are not aligned over the basal bone. These abnormal positions need to be reversed before orthognathic surgery, often making the patient’s facial esthetics worse just before surgery (Figure 5.7).

Figure 5.7. Cephalometric view. A class 3 skeletal patient with severely proclined upper incisors that will require orthodontic uprighting before orthognathic surgery. Extraction of upper premolars will be necessary to allow space for protraction of the upper teeth, making the patient’s facial appearance and negative overjet worse.
5.3 Facial Analysis
•Of critical importance in treatment planning in orthognathic surgery is the relationship of the upper incisor teeth to the upper lip. The patient should be assessed with the lips relaxed and in repose. It is in this position that treatment-planning decisions are made, not in the animated state (Figure 5.8).
–Normally, 2–4 mm of upper incisor crowns should be visible below the upper lip at rest.
–While smiling, 100% of the upper incisors should be visible, with some gingival display considered acceptable.
–If excess upper incisor display is apparent at rest, either the maxilla is vertically long and/or the upper lip is short (Figure 5.9).
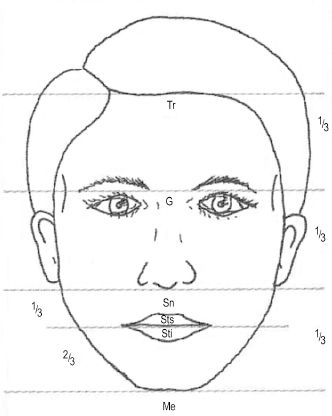
Figure 5.8. Facial thirds analysis is important in revealing facial disharmonies, such as vertical maxillary excess. Reprinted with permission from Quintessence Publishing Co., Inc (Ref. 1). Copyright © 2003 Quintessence Publishing Co., Inc.
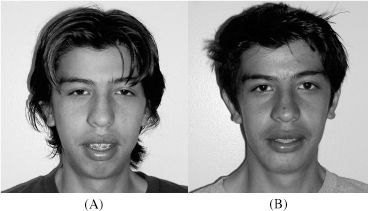
Figure 5.9. Patient with (A) excessive incisor show at rest (vertical maxillary excess) before surgery and (B) with normalization after Le Fort I impaction.

Figure 5.10. Patient exhibiting mentalis strain to obtain lip closure.
–Patients with vertical maxillary excess will often strain the mentalis muscle of the lower lip to facilitate lip closure (Figure 5.10).
•Upper and lower dental midlines should be compared with the facial midline.
•Asymmetries should be assessed with aid of a tongue blade (Figure 5.11).
•Although the angle classification describes occlusal relationships, the same terminology can be used to classify skeletal relationships in the sagittal plane (Figure 5.12):
–Class 1 skeletal: normal relationship of the upper and lower jaws. (ANB angle: 0° to 4.5°. The ANB angle is the relationship of the maxilla to the mandible.)
–Class 2 skeletal: the lower jaw is deficient (ANB angle >4.5°).
–Class 3 skeletal: the lower jaw is prognathic and/or the upper jaw is deficient (ANB angle <0°).
–Note: Skeletal and dental angle classifications do not always correlate. A patient may have a class 1 occlusion but a class 2 skeletal relationship if he or she has had orthodontics to camouflage a class 2 malocclusion. This has relevance when planning for treatment of genioplasty: a class 1 occlusion does not necessarily mean the patient has a mandible of normal length and simply needs advancement genioplasty.

Figure 5.11. Biting on tongue blade reveals significant asymmetry and occlusal canting.

Figure 5.12.
5.4 Cephalometrics
Cephalometric analysis, or the study of specific points and angles of the craniofacial skeleton on a standardized lateral or anterior/posterior (AP) skull film, should be considered an adjunct to the treatment planning of various dentofacial deformities. Cephalometric analyses are based on population norms; what may be considered normal for one patient may not be for the next. The ultimate ideal soft tissue appearance (“soft tissue paradigm”) should be sought for each patient, not based on a numeric analysis aimed at “normalizing” a patient’s radiograph. Below is a list of commonly plotted points on a lateral cephalogram (Figure 5.13):
•S = sella: center of sella turcica.
•N = nasion: intersection of the frontal and nasal bones.
•Ba = basion: anterior portion of foramen magnum.
•ANS = anterior nasal spine: most projecting point.
•PNS = posterior nasal spine: posterior point of hard palate.
•A = subnasale “A point”: the most concave portion of the central anterior maxilla.
•B = supramentale “B point”: the most concave portion of the anterior mandible.
•Pog = pogonion: the most projecting point of the chin.
•Me = menton: the most inferior point of the mandibular symphysis.
•Gn = gnathion: point halfway between Pog and Me.
•Go = gonion: angle of mandible formed by intersection of tangents from posterior border and lower border of the mandible.
•Or = orbitale: the lowest point of the inferior orbital rim.
•Po = porion: the most cephalic portion of the external auditory canal.
•Co = condylion: the most superior point of the condylar head.
•Ptm = pterygomaxillary fissure: base of the fissure.
•G = glabella: most projecting point of the frontal bone.
•Different reference planes and angles make up the various cephalometric analyses. Commonly used measurements are as follows (Figure 5.14):
–SN = cranial base plane.
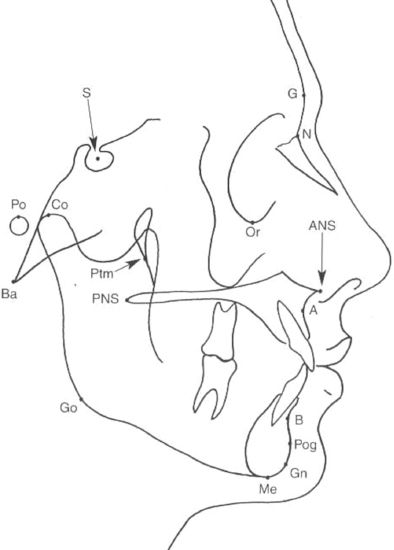
Figure 5.13. Reprinted with permission from Quintessence Publishing Co., Inc. (Ref. 1). Copyright © 2003 Quintessence Publishing Co., Inc.
–Or–Po = Frankfort horizontal plane. This plane parallels the floor in a standard lateral cephalogram.
 Note: Many syndromic patients have an excessively angulated cranial base, thereby making any angle related to SN excessively abnormal. Normally, SN should be at a 6° angle to the Frankfort horizontal plane.
Note: Many syndromic patients have an excessively angulated cranial base, thereby making any angle related to SN excessively abnormal. Normally, SN should be at a 6° angle to the Frankfort horizontal plane.
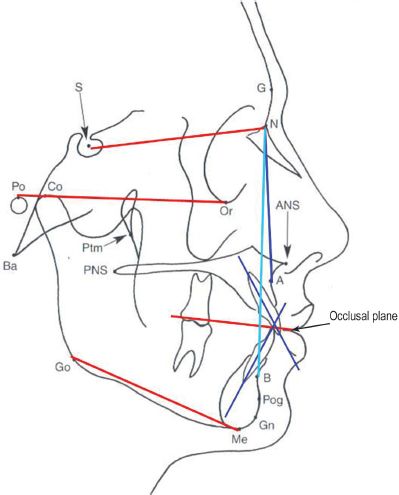
Figure 5.14. Reprinted with permission from Quintessence Publishing Co., Inc. (Ref. 1). Copyright © 2003 Quintessence Publishing Co., Inc.
–Occlusal plane = line bisecting the incisal overbite and molar contacts.
–SN–MP = mandibular plane angle, the angle between the cranial base and the lower border of the mandible (32°). A patient with Treacher Collins syndrome would have a high mandibular plane angle.
–SNA = relationship of the maxilla to the cranium (81°). A patient with a deficient maxilla would have an angle <81°.
–NA = relationship of the nasion to the subnasale A point, the most concave portion of the central anterior maxilla; subset of SNA.
–SNB = relationship of the mandible to the cranium (79°). A prognathic patient would have an SNB > 79°.
–NB = relationship of the nasion to the supramentale B point, the most concave portion of the anterior mandible; subset of SNB.
–SNPog = relationship of the chin to the cranium (80°).
–ANB = relationship of the maxilla to the mandible (0°−4.5°). A class 2 skeletal patient would have an ANB > 4.5°, whereas a class 3 skeletal patient would have an ANB < 0° (or a negative number).
–Maxillary incisor position = the maxillary incisor is related to NA both spatially and in angularity. The incisal edge should be 4 mm anterior to line NA, and the long axis should be angulated 22° relative to NA. These numbers provide information about incisor compensations in various dentofacial deformities. A class 3 skeletal patient may have proclined (> 22° and > 4 mm) upper incisors before orthodontic decompensation.
–Mandibular incisor position = the mandibular incisor is related to NB both spatially and in angularity. The incisal edge should be 4 mm anterior to NB, and the long axis should be angulated 25° relative to NB. Before orthodontic decompensation, a class 3 skeletal patient might have retroclined lower incisors (< 25° and < 4 mm), whereas a class 2 patient might have proclined incisors (> 25° and > 4 mm).
•Chin analysis: Although many analyses have been described including the E line, S line, Merrifield Z line, and Holdaway ratio, we prefer the Ulloa-Gonzalez–Stevens line (zero meridian line): a line dropped from the soft tissue nasion perpendicular to the Frankfort horizontal plane should meet soft tissue pogonion ± 2 mm (Figure 5.15).
5.5 Treatment Sequence
A new patient with a dentofacial deformity should be seen by both the orthodontist and surgeon before treatment is started. Both must agree on a treatment plan before surgery, as the orthodontic setup can be quite different depending on the planned surgery. Many times, a surgeon will be referred to a patient by an orthodontist who attempted orthodontic correction of a skeletal problem only to find that surgery was the only option to correct the problem. At this point in treatment, much dental compensation are present and the surgical plan is compromised.
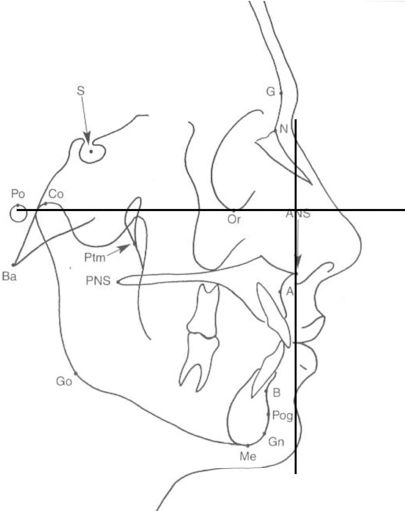
Figure 5.15. Reprinted with permission from Quintessence Publishing Co., Inc. (Ref. 1). Copyright © 2003 Quintessence Publishing Co., Inc.
•Phase 1 (6 months–2 years).
–Surgical.
 Possibly extract teeth (usually premolars) to relieve dental crowding and allow for arch alignment and leveling. Typical extraction patterns in a class 3 skeletal case with dental crowding are upper first and lower second premolars, and in a class 2 skeletal case, upper second and lower first premolars. These extraction patterns are completely opposite to those in a case that will be treated with orthodontics alone.
Possibly extract teeth (usually premolars) to relieve dental crowding and allow for arch alignment and leveling. Typical extraction patterns in a class 3 skeletal case with dental crowding are upper first and lower second premolars, and in a class 2 skeletal case, upper second and lower first premolars. These extraction patterns are completely opposite to those in a case that will be treated with orthodontics alone.
 Remove wisdom teeth (this may also be done at the time of orthognathic surgery).
Remove wisdom teeth (this may also be done at the time of orthognathic surgery).
–Orthodontic.
 Level and align arches (eliminate curve of Spee and “straighten” teeth).
Level and align arches (eliminate curve of Spee and “straighten” teeth).
■Exception: In an openbite case, it may be desirable to leave a step in the maxillary occlusal plane either between canine and lateral or canine and premolar teeth and level the occlusal plane surgically with a segmental osteotomy.
■Exception: In a class 2 skeletal case with short lower anterior facial height, it is desirable to maintain the lower-arch curve of Spee such that as much vertical anterior height as possible is maintained. The arch can be leveled postoperatively.
 Eliminate dental compensations.
Eliminate dental compensations.
 Coordinate arches so that the upper and lower models occlude maximally.
Coordinate arches so that the upper and lower models occlude maximally.
•Phase 2.
–Surgical (see below for specific surgical procedures).
 At what age? At the end of facial growth (determined with serial cephalograms, hand film, or cervical-spine film). For girls, this is around the age of 15 years and for boys, around 18 years.
At what age? At the end of facial growth (determined with serial cephalograms, hand film, or cervical-spine film). For girls, this is around the age of 15 years and for boys, around 18 years.
•Phase 3 (6 months–1 year).
–Postsurgical orthodontics.
•Note: This is the most accepted and standard treatment sequence. Currently, after careful analysis, some perform surgery before orthodontics in an attempt to shorten treatment time.
5.6 Commonly Encountered Dentofacial Deformities
Although grouped separately here, the commonly encountered dentofacial deformities described below often coexist. It is difficult to discuss sagittal discrepancies (profile analysis) without also analyzing vertical relationships, as the following changes in the vertical position of the maxilla will affect mandibular position:
•Mandibular deficiency (class 2 skeletal) (Figure 5.16
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


