Oral and maxillofacial surgeons play a very important role in the primary surgical management of patients with obstructive sleep apnea syndrome (OSAS). Patients with anatomic abnormalities that contribute to narrowing or obstruction of the pharyngeal airway during sleep will benefit from surgery to normalize the hard- and soft-tissue structures.
OSAS is a common disorder, with an incidence of 4% and 2% of middle-aged men and women, respectively, which increases significantly in both sexes past the age of 60. The prevalence of sleep-disordered breathing, which is defined as an apnea-hypopnea index (AHI) of at least 5, is 24% of adult men and 9% of adult women. If these patients complain of daytime sleepiness, then by definition they have OSAS.
The physiologic changes that accompany each obstructive event in patients with OSAS include hypoxemia, hypercapnia, fluctuations in intrathoracic pressure caused by increased respiratory effort, arousal from sleep, and increased sympathetic tone. On a repetitive basis, these physiologic events are believed to result in the hypertensive, cardiovascular, and neurocognitive consequences that have been associated with OSAS. There is evidence demonstrating an association between OSAS and cardiovascular morbidity and mortality as well as systemic hypertension. This relationship was brought to the public’s attention in December 2004 by the following national headline: “The untimely and tragic death of National Football League legend, Reggie White, serves as a warning of the grave consequences of untreated sleep apnea, which is reported to have contributed in part to Mr. White’s death.” Deficits affecting attention, concentration, vigilance, manual dexterity, visual motor skills, memory, verbal fluency, and executive function have been reportedly associated with OSAS. Excessive daytime sleepiness can undoubtedly influence one’s driving performance. Prospectively gathered motor vehicle accident rates in OSAS patients have been found to be 1.3 to 7 times higher than those in the general population. There is evidence indicating an increased risk of occupational accidents for those with OSAS. OSAS is a life-threatening disease that predisposes the patient to physical harm, significant social discord, and poor quality of life.
A review of the literature on obstructive sleep apnea and treatment produces over 3400 articles. A breakdown of these articles reveals approximately 13 nonsurgical options. These options include tongue and palatal muscle training by intraoral electrical neurostimulation; sleeping in a supine, knees-up position; and oral sprays. In many cases these options are suggested not because they are successful but to give patients an alternative so that they do not have to undergo surgery. The surgical options total approximately 19 procedures and deal with surgery in the following regions and tissues of the head and neck: the pharynx, hyoid, tonsillar region, tongue, palate, nasal turbinates, nasal septum, and nasal valve. When one examines the biologic foundation for many of the treatment options, both surgical and nonsurgical, there is often little basis for achieving a successful outcome. This is because in most articles the criteria for the diagnosis of an anatomic abnormality are not clear.
Treatment options recommended to sleep apnea patients should be based on scientific rationale rather than trial and error. The clinician should look at the biologic foundation of each treatment option to determine the basis for achieving a successful outcome. When surgical treatment is recommended, criteria for diagnosing an anatomic abnormality should be used.
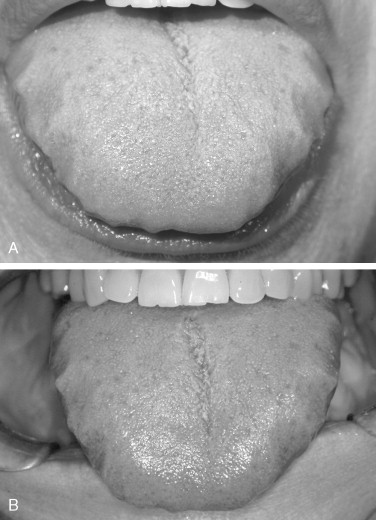
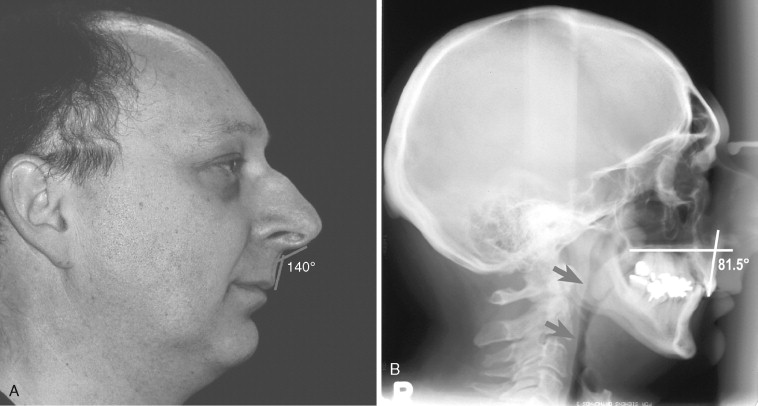
Because OSAS is caused by an underlying abnormality that narrows or obstructs the airway, it is logical to identify an anatomic variant from normal before instituting treatment, surgical or otherwise. For many recommended surgical procedures, such as uvulopalatopharyngoplasty (UPPP), tongue reduction, and hyoid advancement, accepted parameters have not been established to allow the surgeon to identify abnormalities in the size or position of the tongue and soft palate. The decision to perform surgery on either of these two structures becomes very subjective, and success is based on trial and error. This approach does not favor a predictable outcome ( Figures 14-1 and 14-2 ). The oral and maxillofacial surgeon’s experience in diagnosing hard- and soft-tissue abnormalities based on clinical examination, radiographs, and cephalometric analysis allows the development of a treatment plan in an objective fashion using set criteria. This approach results in a more predictable outcome and a much higher rate of success.

PATHOPHYSIOLOGY
For the best treatment options to be determined, an understanding of the underlying pathology is necessary. Obstructive sleep apnea is characterized by recurrent episodes of partial and/or complete closure of the upper airway (UAW) during sleep. A fundamental problem associated with obstructive sleep apnea (OSA) is the inability to maintain UAW patency when sleeping, which can result in reduction (hypopnea) and/ or cessation (apnea) of breathing. The obstruction can occur at any level of the airway, and it is critical to diagnose where the problem is.
Overnight polysomnography conducted in a sleep laboratory remains the gold standard for the diagnosis of sleep apnea and identifies apnea caused by obstructive or central events. Central sleep apnea (CSA) is characterized by a lack of drive to breathe during sleep, resulting in insufficient or absent ventilation and compromised gas exchange. In contrast to OSA, in which ongoing respiratory efforts are observed, central apnea is defined by a lack of respiratory effort during cessations of airflow. CSA, like OSA, is associated with important complications including frequent nighttime awakenings, excessive daytime sleepiness, and increased risk of adverse cardiovascular outcomes. CSA is relatively uncommon and may affect less than 5% of patients referred to a sleep clinic. Typically, CSA is considered to be the primary diagnosis when greater than 50% of apneas are scored as central in origin (i.e., greater than 10 seconds’ cessation of breathing and the absence of respiratory effort) . Typically these patients are thinner and snore less than patients with OSA, although male predominance is likely a common trait. The underlying mechanisms for this disorder are not fully understood. Given the range of pathophysiologic factors contributing to the varied forms of CSA, treatment approaches also vary considerably. Noninvasive ventilation such as nasal continuous positive airway pressure (CPAP) has been shown to be effective in some patients with CSA. The mechanism for improvement in these patients is not clear but may relate to prevention of inhibitory reflex mechanisms that arise during airway closure and potentially CPAP-induced increases in lung volume and O 2 stores. Respiratory stimulants such as acetazolamide and theophylline have been shown to improve CSA in patients with heart failure; however, long-term trials exploring the efficacy and safety of these medications are not yet available.
Overnight polysomnography involves the use of electroencephalogram (EEG), electrooculogram (EOG), electromyogram (EMG), electrocardiogram (ECG), microphone measurement of snoring, pulse oximetry, respiratory inductance plethysmography, air flow measurement, and recording of body position by infrared imaging. The stage of sleep is determined by a combination of EEG, EOG, and EMG. Episodes of apnea and hypopnea are determined from a reduction in air flow in combination with oxygen desaturation. The severity of OSAS is determined by the AHI. Apnea is defined as the cessation of air flow for at least 10 seconds. Obstructive apnea is apnea despite continued respiratory effort. Hypopnea is defined as a substantial reduction in air flow (greater than 50%) or moderate reduction in air flow (less than 50%) with oxygen desaturation of greater than 3% or EEG evidence of arousal during the sleep study. AHI is defined as the number of apneas and hypopneas per hour of sleep. An AHI of 5 to 15 is regarded as mild, 15 to 30 as moderate, and more than 30 as severe OSAS. The highest AHI recorded in the literature is 111; however, we have performed maxillomandibular advancement (MMA) surgery on patients with AHIs of 123 and 129.
The patency of the UAW is maintained mostly by activation of pharyngeal muscles in the underlying soft-tissue structures. This is dependent on the facial skeleton and muscle tone. The fact that patients with a retropositioned maxilla and/or mandible are predisposed to pharyngeal narrowing is well documented in cephalometric studies.
Studies to localize the site of functional obstruction in the UAW have shown there is rarely a single anatomic site of occlusion but more commonly multiple sites of UAW obstruction during episodes of hypopnea and apnea. To determine the anatomic cause and level of obstruction, careful UAW assessment is performed. Physical examination, supine endoscopy with Mueller’s maneuver, and cephalometric radiographs are the primary clinical methods used to identify anatomic abnormalities. Endoscopic evaluation of the UAW is best performed with the patient in the supine position. Both respiratory phase variation and head and neck position may affect UAW size. Endoscopic characteristics of the retropalatal airway include the highest level of retropalatal collapse, soft palate length, prominence of the salpingopharyngeal fold, and prominence of the uvular muscle bulge. Findings of generalized muscle hypertrophy are observed in severe OSA. Anatomic size of the retropalatal volume can be subjectively assessed, along with the area and shape of the velopharynx. Anatomic causes of tongue base prominence can be visualized. Retroglossal and hypopharyngeal airway shape and volume can be estimated during quiet respiration at end expiration. Sagittally directed elliptic shape to the airway implies lateral wall hypertrophy, obesity, and lateral wall collapse. A transversely oriented airway suggests more primary and anatomic abnormalities of anterior structures such as the tongue base and palate. Endoscopic Mueller’s maneuver has been postulated to mimic the collapsibility of UAW during sleep. Mueller’s maneuver is performed by first positioning the endoscope above the epiglottis. The patient is asked to expire against the closed nostrils. The degree and pattern of collapse are then assessed. Because results from Mueller’s maneuver must be subjectively interpreted and because patient respiratory effort varies, verbal description of size, collapsibility, and shape is important to note, rather than just a numeric score.
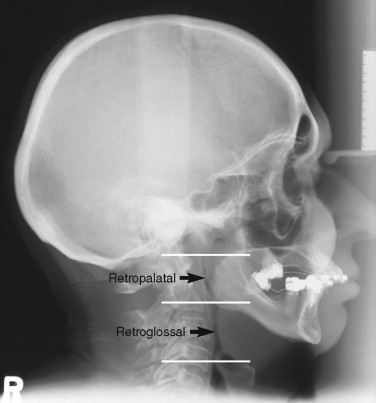
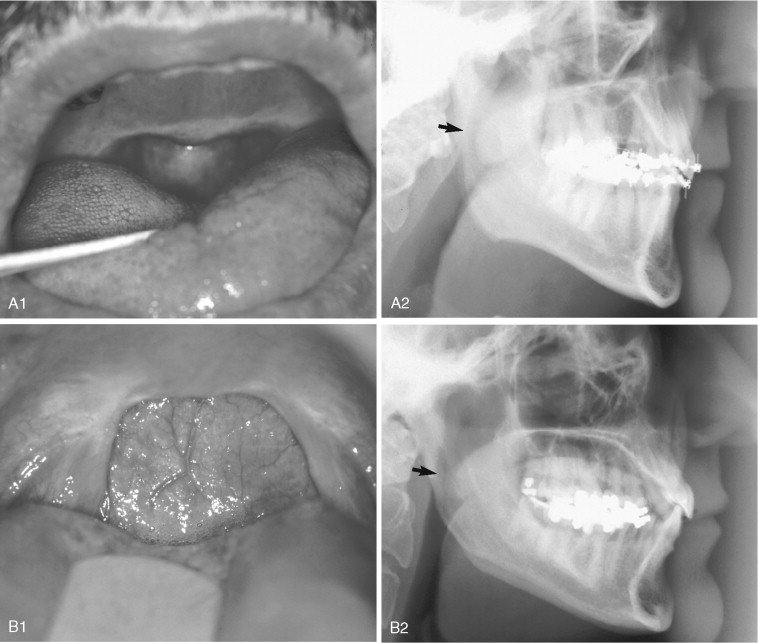
The two major sites of obstruction are in the retropalatal and retroglossal regions ( Figure 14-3 ). Surgical treatment that addresses only one site is predisposed to a low success rate when a multisite problem is being treated.
TREATMENT OPTIONS
To assist the patient in making an informed decision regarding treatment choices, the oral and maxillofacial surgeon must be familiar with the risks and benefits of common treatment options. OSAS can be managed nonsurgically or surgically. The recommended treatment should target the potential contributing factors identified by the history, physical examination, and UAW imaging. The severity of the patient’s condition should also be considered when treatment options are reviewed.
The three main nonsurgical management treatment options include diet, CPAP devices, and oral appliances. Because obesity is a risk factor for OSAS, a reduction in body weight can reduce the number of obstructive apneas. In the Wisconsin Sleep Cohort Study, a 10% weight gain predicted a 32% increase in AHI, whereas a 10% weight loss predicted a 26% decrease in AHI. However, it should be noted that the recurrence of OSAS has been reported after surgically induced weight loss even though the weight was not regained. Although patients may be advised to lose weight, they will have difficulty doing so, particularly in the more severe cases, because excess daytime somnolence and fatigue may discourage the patient from exercising. It is also important to note that approximately 30% of people with OSAS are not obese, and this group of patients most often have an underlying craniofacial deformity.
The most successful nonsurgical treatment is CPAP. This was first reported in 1981, and since that time it has become the gold standard of nonsurgical treatment. Positive pressure is continuously delivered through a sealed nasal mask that the patient wears while sleeping. The positive pressure pneumatically splints the pharyngeal airway open by preventing the soft palate and tongue from making a seal with the posterior pharyngeal mucosa. The pressure required to achieve this is titrated at a sleep laboratory during polysomnography. CPAP is a sound, evidence-based treatment option that has been shown to be effective in decreasing daytime sleepiness and improving mood and quality of life. Unfortunately, because of physical discomfort associated with wearing the unit, drying of the nasal and oral mucous membranes, dislodgement during sleep, noise, and the inconvenience of transporting the unit, the long-term compliance with CPAP use on a nightly basis can be as low as 25%. It is prudent to advise all patients to undergo a trial of CPAP therapy before considering a surgical option.
Oral appliances can also be used in the treatment of sleep apnea. These mandibular advancement devices are similar in design to an orthodontic functional appliance that is worn by the patient during sleep. The objective of these appliances is to stabilize the mandible in a protruded position while the patient sleeps. A review of 19 studies involving 304 patients revealed that oral appliances were effective in 51% of cases as defined by a respiratory disturbance index (RDI) of less than 10. Since this review was published, several randomized controlled trials using either CPAP or an inactive oral appliance have evaluated the effectiveness of mandibular advancement appliances in treating OSAS. Using as a definition of success a posttreatment AHI of 10, the mandibular advancement appliances were between 30% and 54% successful in these studies. Overall, oral appliances are felt to be successful in cases of mild OSAS but relatively less effective in more severe cases. One of the factors limiting wider application of oral appliance treatment is the inability to identify those patients who will have a successful outcome before investing the time and resources necessary to implement this treatment. The significant negative long-term effects of oral appliances are temporomandibular joint pain and detrimental changes in the patient’s occlusion. Almeida and colleagues reviewed 70 patients who used an oral appliance to treat snoring or sleep apnea for more than 5 years and found that 44.3% had unfavorable occlusal changes. An important concern is that a dental appliance may eliminate or decrease snoring in certain patients but their sleep apnea persists, and the patient is not aware of the need to seek further treatment.
Surgical treatment options include tracheostomy, UPPP, isolated hard- and/or soft-tissue surgery, and MMA. Tracheostomy was the first successful surgical treatment for OSAS and has virtually a 100% success rate because it bypasses the obstruction of the UAW completely. Medical and obvious social problems associated with tracheostomy stimulated the search for alternative treatment.
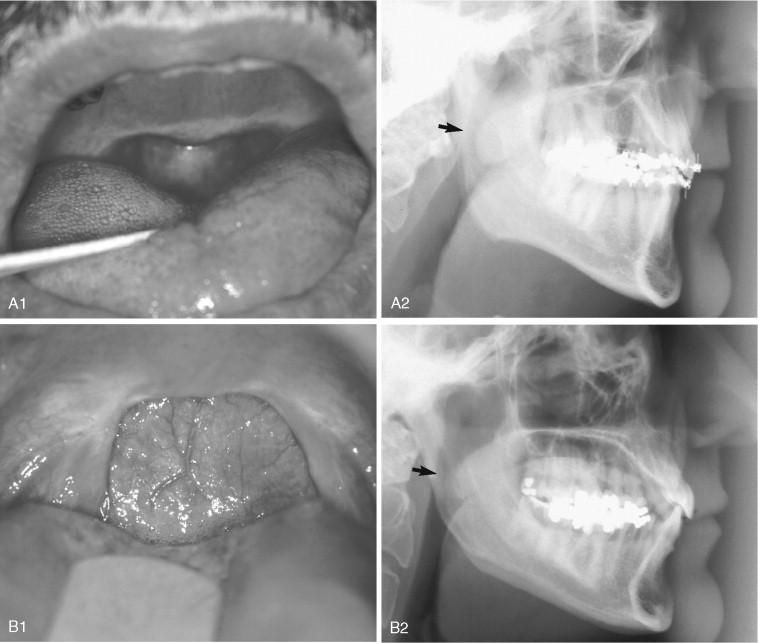
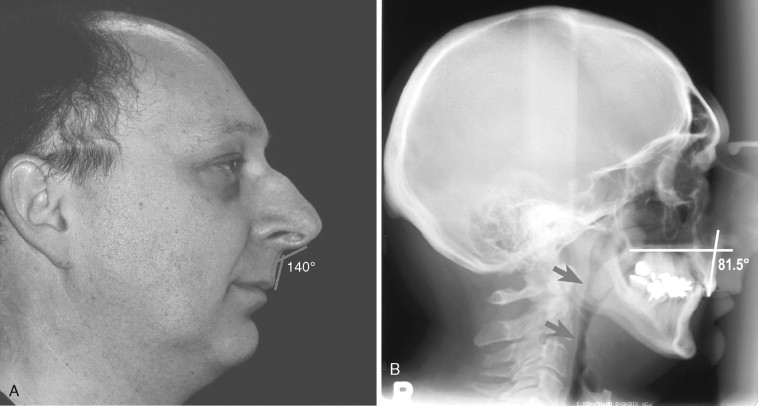
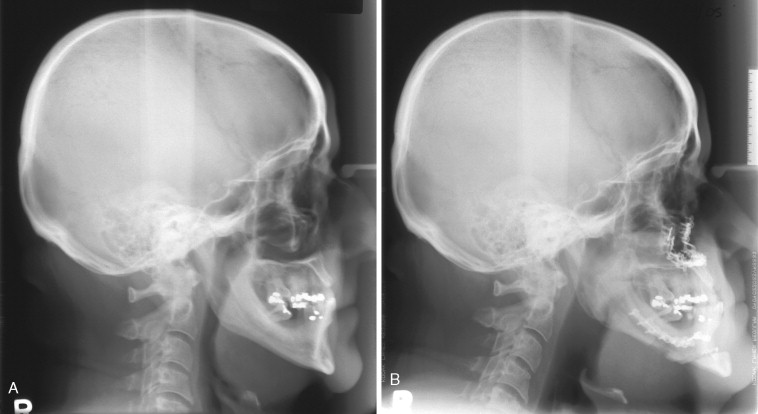
A common surgical treatment is the UPPP originally described in 1981 by Fujita and recommended as a sole treatment for OSAS. It continues to be popular despite reviews that report improvement in less than 50% of patients and complete control of OSAS in less than 25% of patients. The reason for the very low success rate of this procedure is because it addresses only one site of a multisite problem. The soft-tissue changes are unpredictable, and in fact the changes can be detrimental because they cause narrowing of the pharyngeal airway. Clinical examination of the UPPP patient reveals a soft palate that appears shorter and has a firm scar band on the inferior surface. More important, however, is that lateral cephalometric radiographs reveal that although the soft palate is much shorter, it is also much thicker, and this can result in a narrower retropalatal pharyngeal airway as seen on cephalometric radiographs ( Figure 14-4 ). This would explain why the AHI increases in approximately 30% of patients after UPPP. Oral and maxillofacial surgeons obtain extensive information regarding hard and soft tissue of the pharynx using cephalometric radiographs. Review of the literature and clinical experience suggest that many of the other surgical specialties performing soft palate surgery do not use this diagnostic tool either as an aid to rule out an underlying skeletal deformity or to help in analyzing treatment outcomes ( Figure 14-5 ).
The presence of tonsillar or adenoid hypertrophy physically reduces the dimensions of the pharyngeal airway, and surgery to remove this excess tissue should be considered as first-stage treatment when present. If septal deviation or exostosis and turbinate enlargement are present, these abnormalities can be addressed at the same time as a maxillary advancement procedure is performed. Treatments isolated to these areas in the nasal cavity have not proven to significantly benefit the patient, and ultimately the patient requires additional surgical procedures including orthognathic surgery.
Orthognathic surgery has been considered in the treatment of sleep apnea since the later 1970s, and its success has been proven. The biologic basis of this treatment relates to how MMA improves the pharyngeal airway. When a mandibular advancement is performed, the anterior belly of the digastric, the mylohyoid, the genioglossus, and the geniohyoid muscles help pull the tongue upward and forward away from the pharynx ( Figure 14-6 ). Performing a maxillary advancement pulls the soft tissue of the palate forward and upward and also pulls the palatoglossal muscles, which increases tongue support. Both movements have a positive influence on the pharyngeal airway ( Figure 14-7 ). Fiberoptic nasopharyngoscopy after MMA reveals a decrease in airway collapsibility secondary to improvement in lateral pharyngeal wall stability.

TREATMENT OPTIONS
To assist the patient in making an informed decision regarding treatment choices, the oral and maxillofacial surgeon must be familiar with the risks and benefits of common treatment options. OSAS can be managed nonsurgically or surgically. The recommended treatment should target the potential contributing factors identified by the history, physical examination, and UAW imaging. The severity of the patient’s condition should also be considered when treatment options are reviewed.
The three main nonsurgical management treatment options include diet, CPAP devices, and oral appliances. Because obesity is a risk factor for OSAS, a reduction in body weight can reduce the number of obstructive apneas. In the Wisconsin Sleep Cohort Study, a 10% weight gain predicted a 32% increase in AHI, whereas a 10% weight loss predicted a 26% decrease in AHI. However, it should be noted that the recurrence of OSAS has been reported after surgically induced weight loss even though the weight was not regained. Although patients may be advised to lose weight, they will have difficulty doing so, particularly in the more severe cases, because excess daytime somnolence and fatigue may discourage the patient from exercising. It is also important to note that approximately 30% of people with OSAS are not obese, and this group of patients most often have an underlying craniofacial deformity.
The most successful nonsurgical treatment is CPAP. This was first reported in 1981, and since that time it has become the gold standard of nonsurgical treatment. Positive pressure is continuously delivered through a sealed nasal mask that the patient wears while sleeping. The positive pressure pneumatically splints the pharyngeal airway open by preventing the soft palate and tongue from making a seal with the posterior pharyngeal mucosa. The pressure required to achieve this is titrated at a sleep laboratory during polysomnography. CPAP is a sound, evidence-based treatment option that has been shown to be effective in decreasing daytime sleepiness and improving mood and quality of life. Unfortunately, because of physical discomfort associated with wearing the unit, drying of the nasal and oral mucous membranes, dislodgement during sleep, noise, and the inconvenience of transporting the unit, the long-term compliance with CPAP use on a nightly basis can be as low as 25%. It is prudent to advise all patients to undergo a trial of CPAP therapy before considering a surgical option.
Oral appliances can also be used in the treatment of sleep apnea. These mandibular advancement devices are similar in design to an orthodontic functional appliance that is worn by the patient during sleep. The objective of these appliances is to stabilize the mandible in a protruded position while the patient sleeps. A review of 19 studies involving 304 patients revealed that oral appliances were effective in 51% of cases as defined by a respiratory disturbance index (RDI) of less than 10. Since this review was published, several randomized controlled trials using either CPAP or an inactive oral appliance have evaluated the effectiveness of mandibular advancement appliances in treating OSAS. Using as a definition of success a posttreatment AHI of 10, the mandibular advancement appliances were between 30% and 54% successful in these studies. Overall, oral appliances are felt to be successful in cases of mild OSAS but relatively less effective in more severe cases. One of the factors limiting wider application of oral appliance treatment is the inability to identify those patients who will have a successful outcome before investing the time and resources necessary to implement this treatment. The significant negative long-term effects of oral appliances are temporomandibular joint pain and detrimental changes in the patient’s occlusion. Almeida and colleagues reviewed 70 patients who used an oral appliance to treat snoring or sleep apnea for more than 5 years and found that 44.3% had unfavorable occlusal changes. An important concern is that a dental appliance may eliminate or decrease snoring in certain patients but their sleep apnea persists, and the patient is not aware of the need to seek further treatment.
Surgical treatment options include tracheostomy, UPPP, isolated hard- and/or soft-tissue surgery, and MMA. Tracheostomy was the first successful surgical treatment for OSAS and has virtually a 100% success rate because it bypasses the obstruction of the UAW completely. Medical and obvious social problems associated with tracheostomy stimulated the search for alternative treatment.
A common surgical treatment is the UPPP originally described in 1981 by Fujita and recommended as a sole treatment for OSAS. It continues to be popular despite reviews that report improvement in less than 50% of patients and complete control of OSAS in less than 25% of patients. The reason for the very low success rate of this procedure is because it addresses only one site of a multisite problem. The soft-tissue changes are unpredictable, and in fact the changes can be detrimental because they cause narrowing of the pharyngeal airway. Clinical examination of the UPPP patient reveals a soft palate that appears shorter and has a firm scar band on the inferior surface. More important, however, is that lateral cephalometric radiographs reveal that although the soft palate is much shorter, it is also much thicker, and this can result in a narrower retropalatal pharyngeal airway as seen on cephalometric radiographs ( Figure 14-4 ). This would explain why the AHI increases in approximately 30% of patients after UPPP. Oral and maxillofacial surgeons obtain extensive information regarding hard and soft tissue of the pharynx using cephalometric radiographs. Review of the literature and clinical experience suggest that many of the other surgical specialties performing soft palate surgery do not use this diagnostic tool either as an aid to rule out an underlying skeletal deformity or to help in analyzing treatment outcomes ( Figure 14-5 ).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


