This case report demonstrates the interdisciplinary treatment of an adult patient with a Class II malocclusion, convex profile, incompetent lips, gummy smile, and advanced periodontal loss. Initial periodontal-endodontic treatment was followed by orthodontic and orthognathic surgical therapies. An esthetic facial profile, a pleasing smile, an appropriate occlusion, and overall good treatment outcomes, including the periodontal condition, remained stable 11 years after active orthodontic treatment.
Advanced periodontal disease is primarily characterized by severe attachment loss and reduction of alveolar bone support. Since the numbers of adults seeking orthodontic treatment are increasing, orthodontists are becoming more likely to manage patients with adult periodontitis. The most common orthodontic problems in periodontally affected patients include proclination of the maxillary anterior teeth, rotation, overeruption, migration, tooth loss, irregular interdental spacing, and traumatic occlusion. Those changes in the dentition are a consequence of the diminished support provided by the affected periodontium. Adequate orthodontic and periodontal treatment has been shown to improve the periodontal condition and reestablish a healthy and well-functioning dentition.
The vertical maxillary excess that causes excessive exposure of the gingiva on smiling is an esthetic problem. If this gummy smile were characterized by anterior vertical maxillary overgrowth, the outcome might not always be successful with conventional orthodontic therapy alone. In these patients, surgical therapy, such as that provided by a LeFort impaction or maxillary gingivectomies, is often indicated to achieve a good smile.
This case report describes the management of a gummy smile in a woman with a Class II malocclusion and advanced periodontal disease (horizontal and vertical alveolar bone loss). The outcomes throughout the 11-year follow-up in this periodontally affected patient show successful results, with improvements of esthetics and function through an interdisciplinary approach.
Diagnosis and etiology
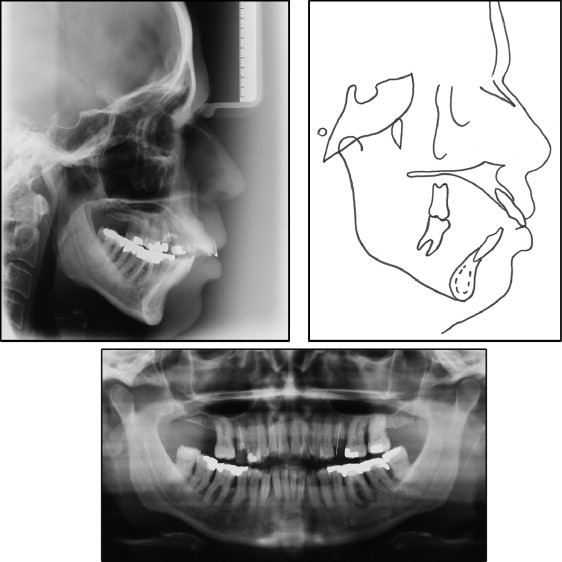
A woman, age 37 years, came for orthodontic treatment with the chief complaint of maxillary anterior dental appearance, and she desired to improve her face. The facial photographs showed an excessive display of gingivae on smiling, a convex profile, and incompetent lips. The intraoral photographs and dental casts evidenced an overjet of 12 mm, an anterior open bite, a negative tooth-size discrepancy in both dental arches, a deviation of the maxillary midline of 2.5 mm to the left, and a complete Class II molar relationship on both sides. The incisors and the canines were crowded, with mild migration and moderate rotation ( Figs 1 and 2 ).

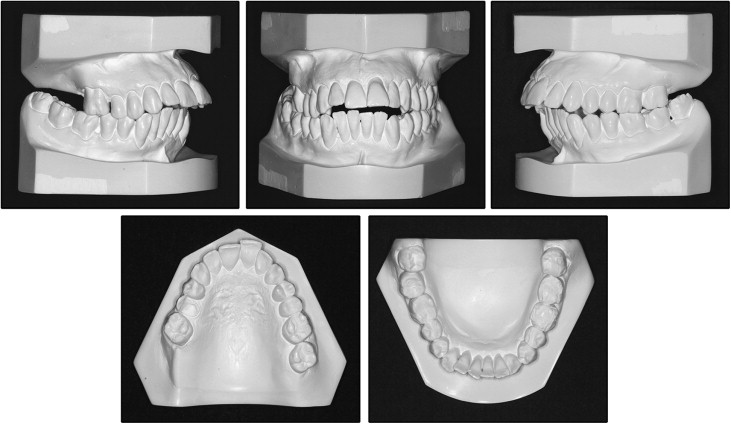
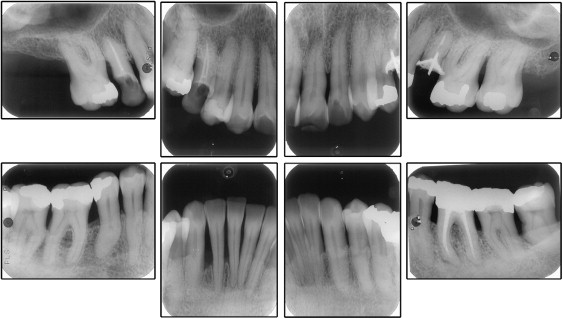
The cephalometric analysis showed a Class II jaw-base relationship, an ANB angle of 7°, labially tipped incisors, biprotrusion (1:NA, 14 mm and 35°; 1:NB, 12 mm and 38°; IMPA, 100°), a mandibular plane angle of 33°, and an occlusal plane angle of 13°. The McNamara analysis showed mandibular retrusion in relation to the cranial base. Panoramic and periapical radiographs showed all permanent teeth, except for the maxillary right second molar and right and left third molars. An apical radiolucent area suggested a periapical lesion of the mandibular left first molar. The patient suffered from advanced periodontal disease with generalized horizontal bone loss in both arches and vertical bone defects between the maxillary left first and second molars and in the mandibular right canine area ( Figs 3 and 4 ; Table ).
| Measurement | Pretreatment | Posttreatment | 11 years posttreatment |
|---|---|---|---|
| SNA (°) | 85 | 86.5 | 86.5 |
| SNB (°) | 78 | 82 | 81 |
| ANB (°) | 7 | 4.5 | 5.5 |
| 1-NA (mm) | 14 | 6 | 5.5 |
| 1:NA (°) | 35 | 20 | 19 |
| 1-NB (mm) | 12 | 8 | 9 |
| 1:NB (°) | 38 | 28 | 25 |
| 1:1 (°) | 104 | 128 | 131 |
| Occl:SN (°) | 13 | 15 | 17 |
| GoGn.SN (°) | 33 | 29 | 30 |
| S-LS (mm) | 2 | −2 | −2 |
| S-LI (mm) | 6 | −2 | −2 |
| Y-axis to FH (°) | 63 | 58 | 58 |
| NPog.FH (°) | 85 | 90 | 90 |
| Angle of convexity (°) | 15 | 9 | 10 |
| Wits appraisal (mm) | +7 | −1 | −1 |
| FMA (°) | 29 | 24 | 25 |
| FMIA (°) | 52 | 63 | 65 |
| IMPA (°) | 100 | 93 | 89 |
| Nasolabial angle (°) | 95 | 118 | 122 |
| A-Nperp (mm) | +2 | +4 | +4 |
| Co-A (mm) | 84 | 85 | 85 |
| Co-Gn (mm) | 108 | 111 | 111 |
| AIFH (mm) | 76 | 70 | 71 |
| Pog-Nperp (mm) | −10 | +2 | +2 |
| Z-angle (°) | 61 | 86 | 81 |
| Ls to (Sn-Pg′) | 6.5 | +2 | +2 |
| Li to (Sn-Pg′) | 7 | +1 | +1 |
The primary cause for the onset and progression of gingival inflammation and periodontitis is bacterial plaque. Inflammation can lead to rapid and irreversible breakdown of the periodontium. Excessive gingival display or a gummy smile can be divided into several categories according to etiologic factors. In this patient, it occurred by overgrowth of the maxillary anterior dentoalveolar height.
Treatment objectives
The treatment objectives were to (1) correct the vertical and maxillomandibular discrepancies to obtain a normal occlusion, thus improving (2) function and (3) facial esthetics; (4) eliminate crowding; (5) reduce biprotrusion, achieving ideal overjet and overbite; (6) acquire good plaque control and clinically healthy gingivae by periodontal treatment; and (7) reduce or keep the defects at the same level and fixed retention between teeth with bone loss.
Treatment objectives
The treatment objectives were to (1) correct the vertical and maxillomandibular discrepancies to obtain a normal occlusion, thus improving (2) function and (3) facial esthetics; (4) eliminate crowding; (5) reduce biprotrusion, achieving ideal overjet and overbite; (6) acquire good plaque control and clinically healthy gingivae by periodontal treatment; and (7) reduce or keep the defects at the same level and fixed retention between teeth with bone loss.
Treatment alternatives
The occlusal analysis, cephalometric findings, facial analysis, and dental casts were the determining factors for a periodontal-endodontic-orthodontic-surgical approach to the treatment of this patient.
The initial periodontal conditions needed improvement. From discussions involving the periodontist, endodontist, and orthodontist, it was decided to extract the maxillary second and mandibular first premolars in order to upright the proclined incisors. Afterward, maxillary superior repositioning with LeFort I surgery, combined with mandibular advancement and advancement genioplasty, would be necessary.
Treatment progress
Before placement of the orthodontic appliances, the patient received treatment from a periodontist for 3 months, consisting of scaling, root planing, and oral hygiene instructions. A 4-month observation period confirmed patient cooperation and the stability of the periodontal results. During this period, endodontic retreatment of the mandibular left first molar was performed, followed by extractions of the mandibular third molars, maxillary second premolars, and mandibular first premolars.
The maxillomandibular tooth axes were improved during preoperative orthodontic treatment by fixed edgewise appliances with 0.022 × 0.028-in slot brackets in both arches. In the maxillary arch, a typical sequence of archwires, starting with 0.0175-in coaxial, followed by 0.016-in, 0.018-in, 0.020-in, and 0.019 × 0.025-in stainless steel archwires (3M Unitek, Monrovia, Calif), was used. Afterward, a high-pull J-hook headgear was used as anchorage against the maxillary first premolars during distalization of the canines.
In the mandibular arch, segmented archwires with vertical loops were used to upright the mandibular canines, followed by the same sequence of archwires as in the maxillary arch, to eliminate crowding and provide alignment and leveling. The J-hook was used against the canines until complete distalization was achieved.
Retraction of the anterior maxillary teeth was performed with 0.019 × 0.025-in stainless steel archwires with sliding mechanics supported by a high-pull J-hook headgear. This contributed to torque control, bodily movement, and intrusion of the maxillary anterior teeth. The J-hook headgear was adapted to the closing loop archwire at 100 g per side, and the patient was instructed to use it at least 14 hours per day. The force was checked monthly to adjust and keep it continuous. Anterior retraction was conducted for 8 months.
Subsequent impressions were obtained to evaluate the intercuspation and simulate the surgical movements. After cast surgery and predictive tracing, a 5-mm maxillary superior repositioning, mandibular advancement of 5 mm with a bilateral sagittal split ramus osteotomy, and advancement genioplasty of 5 mm were planned. The patient received 0.020 × 0.025-in rectangular archwires with clipped hooks and postoperative recommendations.
The patient was monitored closely for 1 month and was then referred for postoperative orthodontic treatment. The postoperative stage aimed at finalization. Active treatment lasted 48 months. After that, a removable circumferential retainer was placed in the maxillary arch, and a canine-to-canine lingual retainer was bonded in the mandibular arch. The patient was placed in a retention control program with periodic visits. During the active phase of treatment, she had monthly speech rehabilitation and myofunctional therapy sessions to promote correct lingual function. Clinical evaluations by her periodontist were made at 3-month intervals.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


