Conservative treatment of an ameloblastoma often requires an occlusal reconstruction. In this article, we report the successful interdisciplinary treatment of a 14-year-old girl with a unicystic ameloblastoma in the mandible. One year after the marsupialization, enucleation with bone curettage was performed with extraction of the impacted third molar, but the proximal second molar could be maintained. The conservative treatment required long-term use of an obturator, and it caused a total open bite. Additionally, the patient genetically had a Class II malocclusion with severe crowding. Consequently, orthodontic treatment was performed after 4 premolar extractions. There was no recurrence of the ameloblastoma 10 years after the enucleation.
An ameloblastoma is one of the most common odontogenic tumors in the jaw. True ameloblastomas are classified into 3 subtypes: solid and multicystic ameloblastomas, unicystic ameloblastomas, and peripheral ameloblastomas. In the treatment of ameloblastomas, surgical resection with surrounding tissues is still the mainstream approach because of its high recurrence rate. On the other hand, conservative treatment, defined as treatment without a partial or complete resection of the jaw such as an enucleation or a curettage, has been recently recommended to treat unicystic ameloblastomas because they are thought to have recurrence potential but are less aggressive than other subtypes.
After the enucleation, patients are sometimes required to wear an obturator to cover the fenestrated site for several months. In many cases, teeth adjacent to the tumor should be extracted or are displaced by tumor growth, even with conservative treatment. As a result, teeth move unpredictably, and patients with unicystic ameloblastoma often acquire a malocclusion. In such cases, orthodontic occlusal reconstruction can be used.
However, there are few reports describing orthodontic treatment after conservative treatment of ameloblastomas in children and adolescents, since a tumor in a young person is considered a rarity, accounting for approximately 10% to 15% of all reported cases of ameloblastoma. Moreover, only a few reports have shown the long-term observations after enucleation of unicystic ameloblastoma in young patients.
This case report shows 10 years of follow-up of conservative treatment in a young patient with unicystic ameloblastoma and the usefulness of orthodontic occlusal reconstruction.
Diagnosis and etiology
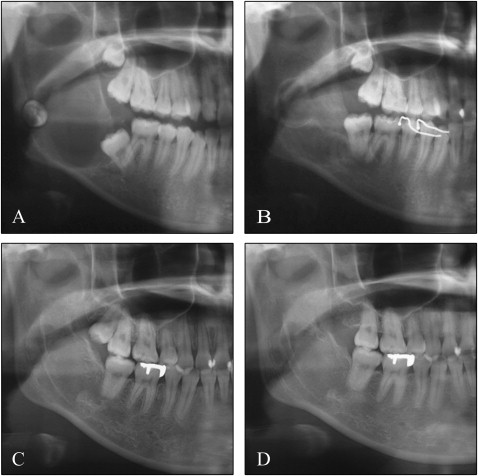
A girl, age 14 years 10 months, consulted the university hospital with a chief complaint of swelling in the mandibular angle and pain on biting. On the panoramic radiograph, the unicystic radiolucent area with the impacted second molar was observed on the right side of mandible ( Figs 1 , A and 2 , A ).

Under general anesthesia, a mucoperiosteal flap was exfoliated along the mandibular right first molar, and a small bone defect appeared at the distal region of the first molar. After aspiration, the pit was enlarged to approximately 20 mm of diameter with a bone forceps. The part of the cyst wall over the second molar was resected, and the crown of the impacted tooth was exposed into the oral cavity. At the same time, an occlusal-splint obturator was placed on the mandible.
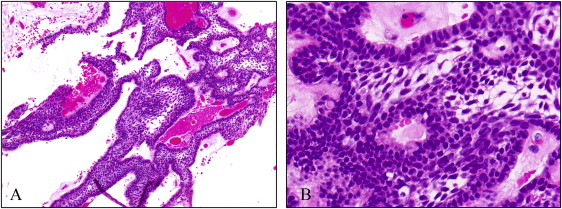
After the biopsy, the lesion was diagnosed as unicystic ameloblastoma. The tumor tissues had proliferation of enamel organ-like structures with a follicular pattern. Neoplastic cells on the stroma looked like ameloblasts, which had cylindrical form with ovoid-shaped nuclei. Some stellate cells were also detected in the internal capsule of the follicle. The stroma consisted of rough connective tissue, and edematous and peripheral hyaline degeneration was also observed. In addition, infiltration of inflammatory cells was found in the stroma ( Fig 3 ).
One year after the marsupialization, the radiolucent area was significantly reduced. Then the enucleation with bone curettage was performed with extraction of the impacted third molar; however, the adjacent impacted second molar could be maintained ( Figs 1 , B and 2 , B ).
Treatment progress
Three years after the surgery, orthodontic treatment was initiated to improve the patient’s genetic and iatrogenic malocclusion ( Fig 4 , A and B ). She was diagnosed as having an Angle Class II malocclusion, with a skeletal Class II jaw-base relationship, severe crowding, and a total open bite from the long-term use of the occlusal splint. Her occlusal contacts were only on the right first molars and the left molars. The mandibular second molar on the affected side was partially erupted with buccal dislocation.





