10. Why do teeth discolor from ingestion of tetracycline during odontogenesis?
Tetracycline binds with the calcium component of bones and teeth and is deposited at sites of active mineralization, causing a yellow-brown endogenous pigmentation of the hard tissues. Because teeth do not turn over the way bone does, this stain becomes a permanent label that fluoresces under ultraviolet light.
11. Which teeth are most commonly missing congenitally?
Third molars, maxillary lateral incisors, and second premolars are the most common.
12. What conditions are associated with multiple supernumerary teeth?
Gardner’s syndrome and cleidocranial dysplasia are two important conditions.
13. What are the most common sites for supernumerary teeth?
Midline of the maxilla (mesiodens), posterior maxilla (fourth molar or paramolar), and mandibular bicuspid areas.
Intrabony Lesions
14. A 40-year-old black woman presents with multiple periapical radiolucencies and radiopacities. What is the diagnosis?
The U.S. black population is prone to developing benign fibro-osseous lesions of various types. They range from localized lesions, such as focal cemento-osseous dysplasia, usually involving the apex of a mandibular molar, to periapical cemento-osseous dysplasia, usually involving the mandibular anterior teeth, to florid (multi-focal) cemento-osseous dysplasia, involving all four quadrants. The term cemento-osseous is preferred to cemental because a combination of cementum droplets and woven bone are usually present (Fig. 4-1).
15. Are fibrous dysplasias of bone premalignant lesions?
Fibrous dysplasia, a malformation of bone, is of unknown cause and is not premalignant, although a gene (GNAS) has been identified for this condition. The monostotic form often affects the maxilla unilaterally. The polyostotic form is associated with various other abnormalities, such as skin pigmentations and endocrine dysfunction (Albright and Jaffe-Lichtenstein syndromes). Cherubism, which used to be termed familial fibrous dysplasia, is probably not a form of fibrous dysplasia and is associated with a different gene mutation (SH3BP2). In the past, fibrous dysplasia was treated with radiation, which sometimes caused the development of osteosarcoma. The best way to treat cherubism is by recontouring the bone after the teenage growth spurt and when lesions become quiescent.
16. True or false: The globulomaxillary cyst is a fissural cyst.
False. Historically, the globulomaxillary cyst was classified as a nonodontogenic or fissural cyst thought to result from the entrapment of epithelial rests along the line of fusion between the lateral maxillary and nasomedial processes. Current thinking puts it into the category of odontogenic cysts of a) developmental origin, and possibly related to the development of the lateral incisor or canine (if the teeth are vital), or of b) inflammatory origin (radicular cyst) if the teeth are nonvital. The two embryonic processes mentioned do not fuse. The fold between them fills in and becomes erased by mesodermal invasion so that there is no opportunity for trapping of epithelial rests. This cyst occurs between the roots of the maxillary lateral incisor and cuspid.
17. True or false: The median palatal cyst is a true fissural cyst.
True. The epithelium of this intrabony cyst arises from proliferation of entrapped epithelium when the right and left palatal shelves fuse in the midline. This should be distinguished from a nasopalatine duct cyst, which arises from remnants of the duct in the area of the nasopalatine foramen. The soft tissue counterpart, which also occurs in the midline of the palate and is known as the palatal cyst of the newborn (Epstein pearl), is congenital and exteriorizes on its own.
18. A neonate presents with a few white nodules on the mandibular alveolar ridge. What are they?
They are most likely dental lamina cysts of the newborn (Bohn nodules). The epithelium of these cysts arises from remnants of dental lamina on the alveolar ridge after odontogenesis. Sometimes they appear at the junction of the hard and soft palate. Dental lamina cysts of the newborn tend to involute and do not require treatment.
19. A boy presents to the dental clinic with multiple jaw cysts and a history of jaw cysts in other family members. What syndrome does he most likely have?
The boy most likely has the bifid rib–basal cell nevus syndrome, which is inherited as an autosomal dominant trait. The cysts are odontogenic keratocysts, which have a higher incidence of recurrence than other odontogenic cysts. The new name for keratocyst is keratocystic odontogenic tumor because they are now considered to be cystic neoplasms. Other findings include palmar pitting, palmar and plantar keratosis, calcification of the falx cerebri, hypertelorism, ovarian tumors, and neurologic manifestations, such as mental retardation and medulloblastomas. Mutation in the PTCH gene is responsible for this condition.
20. Are all jaw cysts that produce keratin considered odontogenic keratocysts?
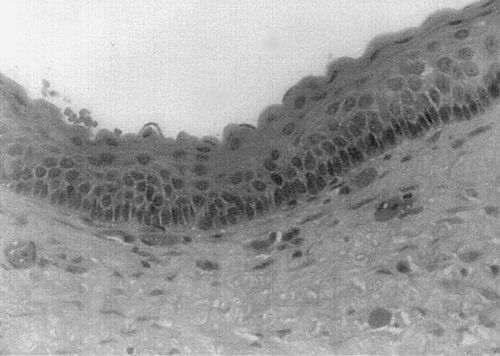
No. The odontogenic keratocyst–keratocystic odontogenic tumor is a specific histologic entity. There is some controversy as to whether this is a cyst or cystic tumor, with the new terminology favoring the latter. The epithelial lining exhibits corrugated parakeratosis, uniform thinness (unless altered by inflammation), and palisading of the basal cell nuclei. The recurrence rate is high, and the condition is associated with the basal cell carcinoma–bifid rib (Gorlin-Goltz) syndrome. Odontogenic cysts that produce orthokeratin do not show the basal cell nuclei changes, do not have the same tendency to recur, and are not associated with the syndrome. These cysts are referred to as orthokeratinized odontogenic cyst. The histologic distinctions are important because they have clinical and prognostic implications.
21. What neoplasms may arise in a dentigerous cyst?
Ameloblastoma, mucoepidermoid carcinoma and, least commonly, squamous cell carcinoma may arise in a dentigerous cyst. Odontogenic tumors that may arise in a dentigerous relationship, although not within a dentigerous cyst, include adenomatoid odontogenic tumor, calcifying cystic odontogenic tumor (Gorlin cyst) and calcifying epithelial odontogenic tumor (Pindborg tumor). The odontogenic keratocyst or keratocystic odontogenic tumor, formerly classified as a cyst and now as a cystic neoplasm, are often seen in a dentigerous relationship with an impacted tooth (Fig. 4-2).
22. What is the difference between a lateral radicular cyst and a lateral periodontal cyst?
A lateral radicular cyst is an inflammatory cyst in which the epithelium is derived from rests of Malassez (like a periapical or apical radicular cyst). It is in a lateral rather than an apical location because the inflammatory stimulus is emanating from a lateral accessory canal. The associated tooth is always nonvital. The lateral periodontal cyst is a developmental cyst in which the epithelium probably is derived from rests of dental lamina. It is usually located between the mandibular premolars, which are vital.
23. What is the incidence of cleft lip and/or cleft palate?
Cleft lip and cleft palate should be considered as two entities, (1) cleft palate alone and (2) cleft lip, with or without cleft palate. The former is more common in females and the latter in males. The incidence of cleft palate alone is 1 in 2000 to 3000 births, whereas the incidence of cleft lip with or without cleft palate is 1 in 700 to 1000 births (highest in Asians and Native Americans). Of all cases, 25% are cleft palate alone and 75% are cleft lip with or without cleft palate.
Soft Tissue Conditions
24. Name some conditions in the mouth that may appear yellow.
Sebaceous material—Fordyce granules
Fat—lipoma or other fatty tumors
Keratin—oral lymphoepithelial cyst (yellow nodules on the base of the tongue, floor of the mouth, or tonsils), epidermoid cyst, dermoid cyst
25. Is benign migratory glossitis (“geographic tongue”) associated with any systemic conditions?
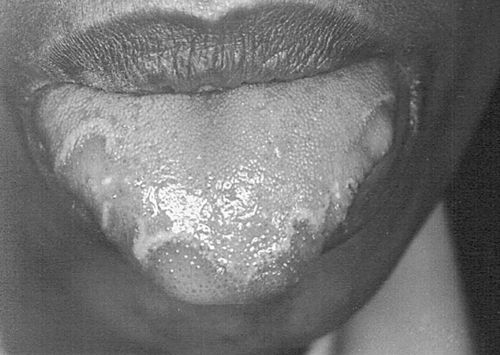
Most cases of benign migratory glossitis are associated with atopy (history of hay fever, asthma, and eczema) and some human leukocyte antigen (HLA) types. Some cases have been associated with fissured tongue and patients with psoriasis, especially generalized pustular psoriasis, have a higher incidence of benign migratory glossitis. (Fig. 4-3).
26. What predisposes to the formation of a coated or hairy tongue?
Hairy tongue is not a developmental lesion but a benign reactive condition. It is caused by reduced shedding and increased buildup of the keratin of the filiform papillae of the tongue. Factors that predispose to this include dehydration, smoking, and reduced intake of coarse foods, fresh foods, and vegetables. Most patients have a history of a recent illness and have been on antibiotics, systemic steroids, and oxygenating mouth rinses. The papillae are putatively colonized by chromogenic bacteria, so the tongue may appear black, brown, or even green. It does not represent candidiasis.
Infections
Fungal Infections
27. Discuss the main clinical forms of candidiasis.
• Pseudomembranous candidiasis (the typical type, with curdy white patches, also known as thrush, tends to have an acute onset)
• Atrophic or erythematous candidiasis often seen under dentures (referred to as denture sore mouth or denture stomatitis); usually present for a long time because the denture often acts as a fomite; may be acute or chronic
• Angular cheilitis presenting as cracked, weepy red areas at the corners of the mouth; tends to be chronic and recurrent
• Median rhomboid glossitis presenting as a red plaque in the midline of the posterior tongue, just anterior of the circumvallate papillae
• Chronic hyperplastic candidiasis presenting as leukoplakia-like patches that do not wipe off easily
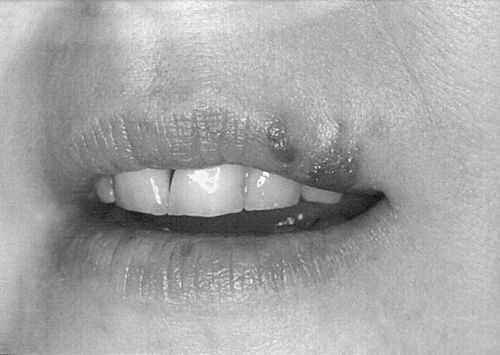
• Chronic mucocutaneous candidiasis (associated with skin candidiasis and an underlying systemic condition such as an endocrinopathy; Fig. 4-4)
28. What factors predispose to candidal infection?
Predisposing factors include the following: (1) poor immune function, which may be related to age (very young and very old), malignancies, immunomodulating medications (topical or systemic), endocrine dysfunction, or human immunodeficiency virus (HIV) infection; (2) malnutrition; (3) antibiotics that upset the normal balance of flora; (4) dental prostheses, especially dentures that act as fomites; and (5) alteration in saliva flow and constituents.
29. A culture performed on an oral ulcer grows Candida spp. Does this mean that the patient has candidiasis?
No. Approximately one-quarter to one-third of the adult population harbors Candida spp. in the mouth. Swabs from patients who are carriers for candida who do not have candidiasis, will grow candida.
30. How do you make a diagnosis of candidiasis?
1. Good clinical judgment. Pseudomembranous plaques of candidiasis usually wipe off with difficulty, leaving a raw, bleeding surface.
2. Potassium hydroxide (KOH) preparation. The plaque is scraped, and the scrapings are put onto a glass microscopic slide. A few drops of KOH are added, the slide is warmed over an alcohol flame for a few seconds, and a coverslip is placed over the slide. The candidal organisms, if present, can be seen with a microscope. Alternatively, the scraping can be placed on a glass slide, fixed in alcohol, and sent to a cytology or pathology laboratory for staining and identification of the organism by light microscopy.
3. Biopsy. This shows hyphae penetrating the tissues (too invasive for routine use).
4. Cultures. Although cultures are not the ideal way to diagnose candidiasis, the quantity of candidal organisms that grow on culture correlates somewhat with clinical candidiasis. Cultures are particularly important for recalcitrant candidiasis to identify drug-resistant species.
31. What are common antifungal agents for treating oral candidiasis?
• Polyenes: nystatin (topical), amphotericin (topical, systemic)
• Imidazoles: clortrimazole, ketoconazole
• Triazoles: fluconazole, itraconazole, voriconazole
32. True or false: Actinomycosis represents a fungal infection.
False. Actinomycetes is a gram-positive bacteria. Do not be fooled by the suffix -mycosis.
33. What are sulfur granules?
These yellowish granules (hence the name) are seen within the pus of lesions of actinomycosis. They represent aggregates of Actinomyces (usually A. israelii), which are invariably surrounded by neutrophils.
34. Name two opportunistic fungal diseases that often present in the orofacial region.
Aspergillosis and zygomycosis tend to infect immunocompromised hosts; the latter causes rhinocerebral infections in patients with diabetes mellitus.
35. Name the deep fungal infections that are endemic in North America.
Histoplasmosis (caused by Histoplasma capsulatum) is endemic in the Ohio-Mississippi basin, coccidioidomycosis (caused by Coccidioides immitis) is endemic in the San Joaquin Valley in California, and blastomycosis (caused by Blastomyces) dermatitidis is endemic from the Great Lakes basin to the Mississippi valley.
Viral Infections
36. Name the six most common viruses of the Herpesviridae family that often present in the orofacial area.
| Herpes simplex virus types 1 and 2 (HSV-1 and -2) | Varicella zoster virus (VZV) |
| Cytomegalovirus (CMV) | Epstein-Barr virus (EBV) |
| Human herpesvirus 8 |
37. True or false: Antibodies against HSV-1 protect against further outbreaks of the disease.
False. The herpes viruses are unique in that they exhibit latency. Once a person has been infected by HSV-1, the virus remains latent within the sensory ganglia (e.g., trigeminal ganglion) for life. When conditions are favorable (for the virus, not the patient), HSV travels along nerve fibers and causes a mucocutaneous lesion at a peripheral site, such as a cold sore on the lip. A positive antibody titer (immunoglobulin G [IgG]) indicates that the patient has been previously exposed, and at the time of reactivation the titer may rise. Hypersensitivity to recurrent HSV infections may lead to an ulcerative condition called erythema multiforme.
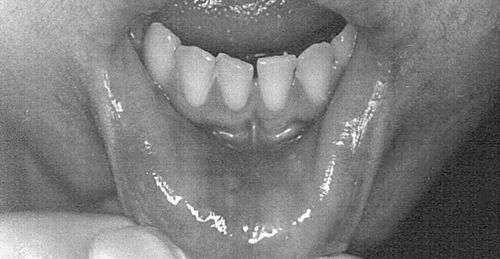
38. How do you differentiate between recurrent aphthous ulcers and recurrent herpetic ulcers?
Clinically, recurrent aphthous ulcers (minor) occur only on the nonkeratinized mucosae of the labial mucosa, buccal mucosa, sulci, ventral tongue, soft palate, and faucial pillars. Recurrent herpetic ulcers occur on the vermilion border of the lips (cold sores or fever blisters) and on the keratinized mucosae of the palate and attached gingiva in immunocompetent individuals. A culture confirms the presence of virus. In immunocompromised hosts, however, recurrent herpetic lesions may occur on the keratinized and nonkeratinized mucosae and may mimic aphthous ulcers (Fig. 4-5).
39. An older patient with long-standing rheumatoid arthritis presents with a history of upper respiratory tract infection, ulcers of the right hard palate, right facial weakness, and vertigo. What does this patient have?
The patient has herpes zoster infection, which typically is unilateral. The patient also has Ramsay-Hunt syndrome, which is caused by infection of cranial nerves VII and VIII with herpes zoster, leading to facial paralysis, tinnitus, deafness, and vertigo.
40. What lesions associated with the Epstein-Barr virus may present in the orofacial region?
41. How does infectious mononucleosis present in the mouth?
Infectious mononucleosis usually presents as multiple, painful, punctate ulcers of the posterior hard palate and soft palate in young adults or adolescents. It is often associated with regional lymphadenopathy and constitutional signs of a viral illness, such as fever and malaise.
42. What oral lesions have been associated with infection by human papillomavirus (HPV)?
The benign conditions are usually associated with HPV-6 and -11; the malignant ones are usually associated with HPV-16 and -18. Heck’s disease is associated with HPV-13 and HPV-32.
43. What oral conditions does coxsackievirus cause?
Herpangina and hand-foot-and-mouth disease are caused by the type A coxsackievirus and generally affect children, who then develop oral ulcers associated with an upper respiratory tract viral prodrome. Lymphonodular pharyngitis is also caused by coxsackievirus.
44. What are Koplik spots?
Koplik spots are early manifestations of measles or rubeola (hence they also are called herald spots). They are 1- to 2-mm, yellow-white ulcers with surrounding erythema that occur on the buccal mucosa, usually a few days before the body rash of measles is seen. Koplik spots are not usually seen in German measles.
Other Infections
45. What are the organisms responsible for noma?
Noma, which is a gangrenous stomatitis resulting in severe destruction of the orofacial tissues, is usually encountered in areas in which malnutrition is rampant. The bacteria are similar to those associated with acute necrotizing ulcerative gingivitis—namely, spirochetes, fusiform bacteria, and others. It is sometimes seen in patients with AIDS.
46. What are the oral findings in syphilis?
Primary: oral chancre
Secondary: mucous patches, condyloma lata
Tertiary: gumma (ulcerated nodules), glossitis
Congenital: enamel hypoplasia, mulberry molars, notched incisors
47. What is a granuloma?
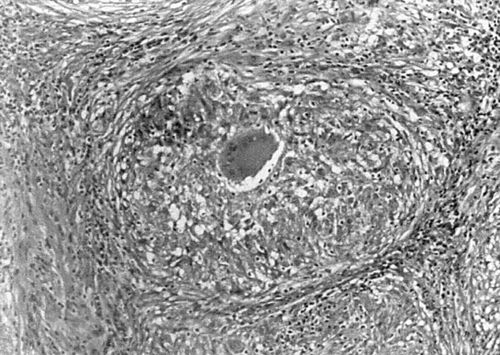
Strictly speaking, a granuloma is a collection of epithelioid histiocytes that is often associated with multinucleated giant cells such as the Langhans-type giant cells seen in granulomas of tuberculosis (caused by Mycobacterium tuberculosis). Many infectious agents, including fungi (e.g., Histoplasma spp.) and those causing tertiary syphilis (Treponema pallidum) and cat scratch disease (Bartonella henselae), can produce granulomatous reactions. Foreign body reactions are often granulomatous. Orofacial granulomatosis may be related to hypersensitivity to foods, flavorings, and preservatives. Crohn’s disease and sarcoidosis are granulomatous diseases of unclear etiology (Fig. 4-6).
48. What are Langhans cells?
Langhans cells are multinucleated giant cells seen in granulomas, usually those caused by M. tuberculosis. Their nuclei have a characteristic horseshoe distribution. Do not confuse them with Langerhans cells, which are antigen-processing cells.
Reactive, Hypersensitivity, and Autoimmune Conditions
Intrabony and Dental Tissues
49. True or false: The periapical granuloma is composed of a collection of histiocytes—that is, a true granuloma.
False. The periapical granuloma is a tumor-like (-oma) proliferation of granulation tissue found around the apex of a nonvital tooth. It is associated with chronic inflammation from pulp devitalization. The inflammation can stimulate proliferation of the epithelial rests of Malassez to form an apical radicular or periapical cyst (Fig. 4-7).
50. What is condensing osteitis?
Condensing osteitis, a relatively common condition, manifests as an area of radiopacity in the bone, usually adjacent to a tooth that has a large restoration or endodontic therapy, although occasionally it may lie adjacent to what appears to be a sound tooth. It is asymptomatic. Histologically, condensing osteitis consists of dense bone, with little or no inflammation. It probably arises as a bony reaction to a low-grade inflammatory stimulus from the adjacent tooth. Idiopathic osteosclerosi, bone scar and dense bone island are terms used for similar bone lesions unassociated with teeth.
51. What are the different causative factors between the wearing down of teeth caused by attrition, abrasion, erosion, and abfraction?
Attrition: tooth to tooth contact
Abrasion: a foreign object to tooth contact (e.g., toothbrush bristles, bobby pins, nails)
Erosion: a chemical agent to tooth contact (e.g., lemon juice, gastric juices)
Abfraction: occlusal stress leading to excessive tensile forces, which cause damage to enamel at cervical areas of the teeth
Soft Tissue Conditions
52. Name some systemic conditions associated with aphthous-like ulcers.
53. True or false: An aphthous ulcer is the same as a traumatic ulcer.
False, but with reservations. A traumatic ulcer is the most common form of oral ulcer and, as its name suggests, occurs at the site of trauma, such as the buccal mucosa, lateral tongue, lower labial mucosa, or sulci. It follows a history of trauma, such as mastication or toothbrush injury. An aphthous ulcer may occur at the same sites, but often with no history of trauma. However, patients prone to developing aphthae tend to do so after episodes of minor trauma (Fig. 4-8).
54. A child returns after a visit to the dentist at which several amalgam restorations were placed. The child now has ulcers of the lateral tongue and buccal mucosa on the same side as the amalgams. What is your diagnosis?
This is a factitial injury. Children may inadvertently chew their tongues and buccal mucosae while tissues are numb from local anesthesia because the tissues feel strange to the child. Children and parents should be advised to be alert for such behavior.
55. Is the mucocele a true cyst?
It depends. The term mucocele refers loosely to a cystlike lesion that contains mucus and usually occurs on the lower lip, ventral tongue, or floor of the mouth. However, it may occur wherever mucous glands are present. In most cases, it is not a true cyst because it is not lined by epithelium. It is caused by escape of mucus into the connective tissue when an excretory salivary duct is traumatized. Therefore, the mucocele is lined by fibrous and granulation tissue. In a few cases, it is caused by distention of the excretory duct because of a distal obstruction or the presence of a sialolith; the preferred term is salivary duct cyst.
56. What is the cause of necrotizing sialometaplasia?
This painless ulcer usually develops on the hard palate but may occur wherever salivary glands are present. It represents vascular compromise and subsequent infarction of the salivary gland tissue, with reactive squamous metaplasia of the salivary duct epithelium that may mimic squamous cell carcinoma. The lesion resolves on its own.
57. Name the major denture-related findings in the oral cavity.
• Chronic atrophic candidiasis, especially of the palate (denture sore mouth)
• Papillary hyperplasia of the palatal mucosa
• Fibrous hyperplasia of the sulcus where the denture flange impinges (epulis fissuratum)
• Traumatic ulcers from overextension of flanges
• Angular cheilitis (candidiasis) from overclosure
• Denture base hypersensitivity reactions (very uncommon; resembles chronic atrophic candidiasis)
58. A patient is suspected of having an allergy to denture materials. What do you recommend?
The first thing is to rule out chronic atrophic candidiasis (denture stomatitis or denture sore mouth) because this much more common. The patient should be treated with fluconazole (much more effective than nystatin or clotrimazole) or Mycostatin–triamcinolone cream applied directly to the denture to be worn by the patient; the denture must also be soaked in an antifungal agent overnight because it is a fomite. If these measures are taken and there is no response, the patient should be patch-tested by an allergist or dermatologist to a panel of denture base materials, which include metals and acrylic polymerization products. Usually, the lesions resolve with topical steroids.
59. What is a gum boil (parulis)?
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses