Introduction
The concept of “ideal” occlusion in harmony with craniofacial structures is often proposed as an ultimate goal of orthodontic treatment. The aim of this study was to assess the impact of slight variations in posterior occlusion and the history of straight-wire orthodontic treatment on the predictability of incisor inclination and third-order angles.
Methods
Axial incisor inclinations, third-order angles, and craniofacial relationships were assessed on lateral headfilms and corresponding dental casts of 75 healthy white subjects, 16 to 26 years old, selected by the general inclusion criterion of a good interincisal relationship. Four groups were formed: group A (n = 17), Angle Class I occlusion subjects with no orthodontic treatment; group B (n = 20), Angle Class I occlusion subjects treated with standardized straight-wire orthodontics; group C (n = 20), up to a half-cusp distal occlusion after straight-wire treatment; and group D (n = 18), up to a half-cusp distal occlusion and no orthodontic treatment. Regression analysis was used to insert predictor angles into selected regression equations of the subjects with “ideal” occlusion, and the absolute differences between predicted and observed response angles were determined.
Results
Small differences in incisor inclination were found between subjects with “ideal” occlusion and those who slightly deviated from “ideal” with a mild occlusion of the Angle Class II category. Posterior occlusion was not relevant to the validity of the vast majority of predictor-response pairs. Straight-wire treatment produced incisor inclination that was slightly protruded compared with subjects who had good natural occlusion.
Conclusions
The “ideal” posterior occlusion concepts as a general orthodontic treatment goal should be reconsidered.
Correction of incisor inclination is a major interest in orthodontics; the diversity of adequate incisor inclination influences a variety of aspects, including esthetics, the patient’s self-perception, function, stability, and phonetics. Guidelines for incisor inclination correction therefore refer mostly to esthetically and functionally acceptable findings in untreated subjects with normal occlusion. Orthodontic dentoalveolar treatment goals are often formulated on the basis of “ideal” occlusion concepts, including an Angle Class I occlusion, adequate canine guidance, and an interincisal relationship judged as good: ie, proper support, no midline deviation, good esthetics, and adequate function. Such an occlusal configuration is normally considered to be “ideal” and can be found naturally in most subjects with differing craniofacial properties who have not been treated orthodontically. In these untreated “ideal” occlusion subjects, variation in incisor inclination is a basic element in achieving dentoalveolar compensation of mild skeletal bias. Accordingly, guidelines for correcting incisor inclination are often formulated on the basis of floating norms, including regression equations for calculating specific incisor positions on the basis of sagittal craniofacial properties, such as the ANB angle.
Several attempts have been made to integrate “ideal” occlusion concepts into orthodontic treatment planning by proposing regression models as guidelines for imitating the natural dentoalveolar compensation mechanism to enable the calculation of either necessary axial incisor inclination or third-order angles as a direct straight-wire treatment goal. On the other hand, an acceptable posterior occlusion—stable and functional with an interincisal relationship not requiring orthodontic treatment because of good esthetics and adequate function—goes beyond the “ideal” Angle Class I occlusion concept. Moreover, judging from previous research, there does not seem to be a significant correlation between functional disorders and slight sagittal variations in occlusion.
It was the aim of this study to test the suitability of a set of regression equations derived from subjects with “ideal” occlusion, either treated with straight wires or untreated, with and without ideal occlusion characteristics, but with the inclusion criterion of good interincisal relationships. Furthermore, we hoped to answer the question of whether equations used previously apply to subjects with proper interincisal relationships, despite variations in posterior occlusion that most orthodontists would consider as deviating from the ideal. The rationales for this group configuration were to check for a dependency between good incisor inclination and moderate Angle class variation, and to elaborate on possible differences between straight-wire treated and natural subjects in terms of the predictability of third-order inclination by using craniofacial findings from lateral radiographs.
The null hypothesis was that there would be no significant differences between the 4 study groups in terms of the prediction error (prediction of third-order angles and axial incisor inclination by using sagittal craniofacial data as a predictor).
Material and methods
Lateral headfilms and corresponding dental casts of 75 white subjects (26 male and 49 female; 16-26 years of age) were arbitrarily and sequentially taken from the files of a private orthodontic practice in Göttingen, Germany, according to the following exclusion criteria: deciduous teeth, missing teeth, filled incisors, crowned teeth, and morphologic tooth anomalies. Four study groups were formed according to the general inclusion criterion of incisor inclination that was considered acceptable or adequate by visual and cephalographic screening (ie, proper interincisal support, no midline deviation, good esthetics, and adequate function), with the exception of minor rotations or minor mandibular crowding of 2 mm or less that would not significantly affect axial incisor inclination, by 2 orthodontists at the University Medical Center of Göttingen, Germany, but otherwise different inclusion characteristics: group A comprised subjects who had not previously undergone orthodontic treatment and who had “ideal” occlusion characteristics, as indicated by an Angle Class I posterior and canine occlusion; group B subjects had the same morphologic dental characteristics after 0.022-in straight-wire treatment (torque-tip incisor prescription, +7°/+5° maxillary incisors, and −1°/+2° mandibular central incisors; Ormco, Orange, Calif) with a standardized archwire sequence, starting with 0.014-in nickel-titanium, followed by a 0.014-in Australian wire, 0.016-in and 0.018-in Australian wires, and a 0.016 × 0.022-in stainless steel wire, and finished with a 0.017 × 0.025-in stainless steel wire; group C comprised subjects who had undergone the same straight-wire treatment routine as did group B, but were finished with a posterior occlusion that deviated slightly from what is considered the “ideal” Angle Class I occlusion, apparent as a distal cusp-to-cusp occlusion of quarter to half cusps, and group D had the same occlusal characteristics, but no orthodontic treatment. This study had a retrospective design, and the orthodontic treatments in groups B and C had already been completed at the time of the assessments. Some subjects in group A later received orthodontic treatment because of minor rotations or minor crowding of less than 2 mm, whereas the subjects in group D later received comprehensive orthodontic care. There was no double assignment of subjects—eg, to group A before treatment and then to group B after treatment.
In the case of disagreement between the assessors concerning a subject’s eligibility, that subject was excluded from the trial sample.
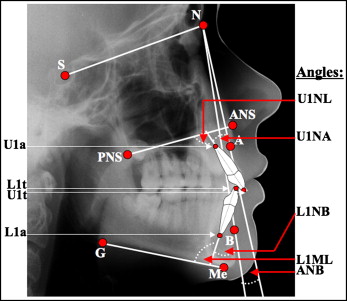
Cephalometric and third-order cast measurements were made. Incisor axis inclination and sagittal craniofacial structures were analyzed by using lateral cephalograms and the landmarks and angles indicated in Figure 1 . Upper (U1) and lower (L1) central incisor inclinations were assessed with reference to the cephalographic lines NA and NL (U1NA, U1NL), and NB and ML (L1NB, L1ML), respectively. Sagittal craniofacial relationships were classified by using the ANB angle.
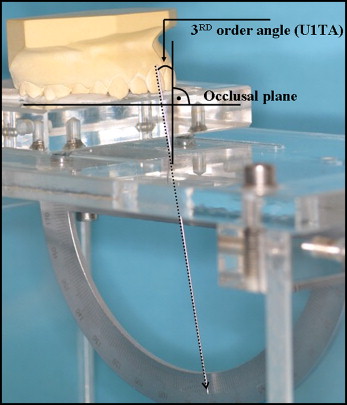
Third-order angles were measured directly from the dental plaster casts of each subject matching corresponding lateral radiograph by using a gauge for measuring third-order angles ( Fig 2 ). Upper and lower right central incisors (U1, L1) were chosen and prepared for assessment by marking the middle of the labial long axis of the incisor’s clinical crown. Third-order values (U1TA, L1TA) were defined as positive if the gingival portion of the facial tangent was lingual to the incisal portion and vice versa.
Both cephalographic tracings and third-order cast measurements were made manually by 1 examiner (M.K.), twice for each headfilm or dental cast, at an interval of 1 week. Repeated measures were subjected to error analysis. The median (minimum, maximum) difference between these 2 measurements for distinct features were U1NA, 0.1° (−6.3°, 5.5°); L1NB, 0.1° (−6.1°, 2.3°); U1NL, 0.1° (−5.0°, 7.4°); L1ML, −0.1° (−7.6°, 4.7°); U1TA, 0.0° (−2.5°, 2.0°); L1TA, −0.5° (−1.5°, 2.0°); and ANB 0.7° (−1.4°, 2.6°).
Statistical analysis
Predictions of cephalographic incisor inclinations (U1NA, U1NL, L1NB, and L1ML) and third-order angles (U1TA and L1TA) were calculated on the basis of sagittal craniofacial relationships (ANB angle) or cephalometric incisor inclination angles by using previously published linear regression equations separately for the 4 study groups ( Tables I and II ). Minimum, maximum, and median absolute deviations of predicted response angles and actual measured response angles were assessed. According to quantile-quantile plots, the data were not normally distributed. Therefore, nonparametric tests were performed. In detail, the absolute deviations were compared between the 4 groups with the Kruskal-Wallis test and, if necessary, with pair-wise Mann-Whitney U tests. The equations used in a previous study, based on 69 subjects with “ideal” occlusion, were updated by simple regression by using the data of the 17 untreated subjects with “ideal” occlusion from this study (group A). Correlations between predictor and response angles were assessed with the Pearson correlation coefficient R. All analyses were carried using the software R (version 2.8; www.r-project.org ) with a level of significance of α = 5%.
| Group | Angle class | Straight-wire treatment | Response | Predictor | Test pairs | Median absolute deviation from actual response (°) (range) |
|---|---|---|---|---|---|---|
| A | I | No | U1NA | ANB | 17 | 4.0 (0.7-12.9) |
| L1NB | ANB | 17 | 7.2 (0.0-20.1) | |||
| U1NL | ANB | 17 | 5.7 (0.3-17.4) | |||
| L1ML | ANB | 17 | 3.6 (0.0-17.4) | |||
| U1TA | U1NA | 17 | 2.0 (0.0-10.0) | |||
| L1TA | L1NB | 17 | 1.9 (0.0-9.8) | |||
| U1TA | U1NL | 17 | 2.9 (0.1-7.6) | |||
| L1TA | L1ML | 17 | 2.1 (0.0-11.3) | |||
| B | I | Yes | U1NA | ANB | 20 | 4.1 (0.1-14.7) |
| L1NB | ANB | 20 | 13.0 (2.2-26.8) | |||
| U1NL | ANB | 20 | 3.8 (0.0-14.3) | |||
| L1ML | ANB | 20 | 5.9 (0.6-16.5) | |||
| U1TA | U1NA | 20 | 3.4 (0.1-9.9) | |||
| L1TA | L1NB | 20 | 2.5 (0.2-11.3) | |||
| U1TA | U1NL | 20 | 2.4 (0.7-8.8) | |||
| L1TA | L1ML | 20 | 2.3 (0.1-7.2) | |||
| C | II | Yes | U1NA | ANB | 20 | 5.3 (0.5-12.1) |
| L1NB | ANB | 20 | 10.8 (0.7-24.3) | |||
| U1NL | ANB | 20 | 1.2 (0.1-8.8) | |||
| L1ML | ANB | 20 | 3.8 (1.1-18.9) | |||
| U1TA | U1NA | 20 | 2.1 (0.2-6.7) | |||
| L1TA | L1NB | 20 | 3.3 (0.2-17.3) | |||
| U1TA | U1NL | 20 | 1.3 (0.1-5.9) | |||
| L1TA | L1ML | 20 | 3.1 (0.1-19.6) | |||
| D | II | No | U1NA | ANB | 18 | 3.4 (0.1-14.4) |
| L1NB | ANB | 18 | 6.5 (1.3-23.5) | |||
| U1NL | ANB | 18 | 5.7 (1.4-13.0) | |||
| L1ML | ANB | 18 | 3.8 (0.1-9.9) | |||
| U1TA | U1NA | 18 | 4.6 (0.2-8.5) | |||
| L1TA | L1NB | 18 | 2.1 (0.2-6.1) | |||
| U1TA | U1NL | 18 | 3.0 (0.4-7.4) | |||
| L1TA | L1ML | 18 | 2.7 (0.1-7.3) |
| Sample | Regression | Correlation | |||||
|---|---|---|---|---|---|---|---|
| Response | Predictor | n | Intercept | Slope | R | P | |
| ES | U1NA | ANB | 69 | 25.10 ± 1.08 | −2.05 ± 0.34 | −0.60 (−0.73, −0.42) | <0.01 |
| U | 86 | 25.67 ± 1.02 | −2.21 ± 0.30 | −0.63 (−0.75, −0.49) | <0.01 | ||
| ES | L1NB | ANB | 69 | 21.27 ± 1.04 | 1.43 ± 0.32 | 0.48 (0.27, 0.65) | <0.01 |
| U | 86 | 21.40 ± 0.97 | 1.13 ± 0.28 | 0.40 (0.21, 0.57) | <0.01 | ||
| ES | U1NL | ANB | 69 | 112.49 ± 1.11 | −1.19 ± 0.34 | −0.39 (−0.58, −0.17) | <0.01 |
| U | 86 | 112.95 ± 1.10 | −1.45 ± 0.32 | −0.44 (−0.60, −0.25) | <0.01 | ||
| ES | L1ML | ANB | 69 | 90.75 ± 1.28 | 1.33 ± 0.40 | 0.38 (0.16, 0.57) | <0.01 |
| U | 86 | 91.19 ± 1.20 | 1.00 ± 0.35 | 0.30 (0.09, 0.48) | <0.01 | ||
| ES | U1TA | U1NA | 69 | −4.74 ± 1.71 | 0.48 ± 0.08 | 0.59 (0.41, 0.73) | <0.01 |
| U | 86 | −5.56 ± 1.41 | 0.51 ± 0.07 | 0.64 (0.49, 0.75) | <0.01 | ||
| ES | L1TA | L1NB | 69 | −20.79 ± 2.62 | 0.71 ± 0.10 | 0.65 (0.49, 0.77) | <0.01 |
| U | 86 | −19.89 ± 2.34 | 0.69 ± 0.09 | 0.63 (0.48, 0.74) | <0.01 | ||
| ES | U1TA | U1NL | 69 | −49.60 ± 10.31 | 0.50 ± 0.09 | 0.55 (0.35, 0.69) | <0.01 |
| U | 86 | −50.38 ± 8.22 | 0.50 ± 0.08 | 0.59 (0.43, 0.71) | <0.01 | ||
| ES | L1TA | L1ML | 69 | −62.83 ± 7.99 | 0.64 ± 0.08 | 0.68 (0.53, 0.79) | <0.01 |
| U | 86 | −57.74 ± 7.36 | 0.58 ± 0.08 | 0.63 (0.48, 0.75) | <0.01 | ||
| ES | U1TA | ANB | 69 | 6.75 ± 1.06 | −0.71 ± 0.33 | −0.26 (−0.46, −0.02) | 0.03 |
| U | 86 | 6.99 ± 0.98 | −0.93 ± 0.29 | −0.33 (−0.51, −0.13) | <0.01 | ||
| ES | L1TA | ANB | 69 | −5.25 ± 1.22 | 0.92 ± 0.38 | 0.28 (0.04, 0.49) | 0.02 |
| U | 86 | −5.23 ± 1.09 | 0.81 ± 0.32 | 0.27 (0.06, 0.45) | 0.01 | ||
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


