Click on the DVD icon to watch the video
Aim
The aim of this chapter is to consider how occlusion may contribute to temporomandibular disorders (TMDs) while emphasising the importance of TMD diagnosis.
Outcome
At the end of this chapter, the clinician should:
-
know the signs and symptoms of TMDs while also understanding the multifactorial origin of these conditions
-
appreciate that these signs and conditions are relatively common in the general population
-
comprehend the nature of the uncertain relationship between occlusion and TMDs
-
be able to screen for TMDs in patients requiring restorative treatment
-
be aware of how to diagnose TMDs in patients with jaw problems and facial pain
-
understand how and why occlusal splints and occlusal adjustment can be used to manage TMDs.
Introduction
The term TMDs describes a group of conditions with similar signs and symptoms that affect the temporomandibular joints (TMJs), the muscles of mastication, or both. In approximate order of importance, the signs and symptoms of TMDs are:
-
pain and tenderness in and around the TMJs and muscles of mastication
-
limitation and incoordination of jaw movement
-
joint sounds – clicking and crepitus (grating of the joint)
-
headaches (increased frequency and severity)
-
tinnitus (occasional association).
Function usually makes symptoms worse, so patients may have difficulty eating or simply talking. A common misconception is that problems with the occlusion are a principal cause of TMDs. Although this may be true for a small proportion of patients, it is not for the vast majority. Nevertheless, there is the potential for an occlusal component to TMDs. This will be discussed later in this chapter. Of real practical importance, TMDs must not be aggravated, let alone overlooked, when providing dental treatment. Before considering these aspects of TMDs, it is worth considering some background.
TMD Background
Signs and symptoms of TMDs occur commonly in the general population, but these are generally of little significance. For instance, around 20% of subjects experience TMJ clicking, but this causes problems for only a few.
Despite extensive research, the aetiology of any given patient’s TMD often remains unclear. We know from epidemiological studies that it often starts in the mid to late teens, but it can present at almost any age. In the general population, there are slightly more females than males with signs and symptoms of TMD. By contrast, in the population attending hospital TMD clinics, the female to male ratio often exceeds 4:1 and there is some evidence that there may be hormonal influences. There are also other influences, including psychosocial factors associated with stress and chronic pain behaviour, but the relationship between pain and psychosocial factors is not straightforward. There is certainly a link between stress-induced parafunctional activity (bruxism) and muscle-related hypertonicity and TMDs. Conversely, there are also many people without TMD symptoms who habitually grind their teeth.
In some patients, symptoms of TMD follow trauma. In others it starts following a change to the occlusion. Interestingly, recent research suggests there are genetic predispositions to TMDs related to the biochemistry of pain experience. This may eventually help to explain why some people are susceptible to TMDs while others are not. There is no single cause of TMDs; they are multifactorial, with factors that clinically appear to:
-
predispose the patient to TMDs – genetic, hormonal, anatomical
-
precipitate TMDs – trauma, occlusal changes, parafunction
-
prolong TMDs – parafunction and psychological stress.
Individual factors, such as parafunction, may even fall into more than one of these categories. Although signs and symptoms of TMD occur commonly in otherwise healthy subjects, there appears to be a greater prevalence in certain systemic conditions, such as fibromyalgia, systemic joint laxity and rheumatoid arthritis. Fibromyalgia is a condition characterised by generalised muscle pain, including masticatory muscle pain. Patients with systemic joint laxity have a collagen defect, predisposing them to strained ligaments. This may, in turn, result in a disc displacement within the TMJ. With rheumatoid arthritis patients, around half experience arthritic TMJ pain. However, most sufferers from TMDs are fairly young and otherwise healthy adults.
Diagnosis of TMDs
Over the years, various systems have been introduced to diagnose TMDs. Nowadays, the gold standard adopted by the international TMD research community is the Research Diagnostic Criteria (RDC/TMD) method. This standardised method of recording a patient’s TMD history and examination considers two axes of diagnosis. Axis I is the physical diagnosis, which provides a description of the anatomical source of the patient’s symptoms. Axis II provides a psychosocial diagnosis, but recording all the necessary information is time consuming and unlikely to be helpful in dental practice. Clinicians must, however, always bear in mind the psychosocial aspects of TMDs, recognising that if a patient appears depressed this may be a reaction to their jaw pain, not necessarily a cause of it.
The criteria to formulate the Axis I diagnosis are quite complex and aimed at research, but the simplicity of the final diagnosis into one of three categories is clinically extremely useful. The three diagnoses are:
-
Group I: muscle (myofascial pain) characterised by muscle tenderness on palpation (see DVD video J).
-
Group II: disc displacements with and without reduction (Figs 7-1 and 7-2) characterised by clicking (with reduction) and locking (without reduction).
-
Group III: TMJ pain and degeneration:
-
arthralgia, characterised by local TMJ tenderness
-
arthrosis, characterised by crepitus
-
arthritis, characterised by crepitus and local TMJ tenderness.
-
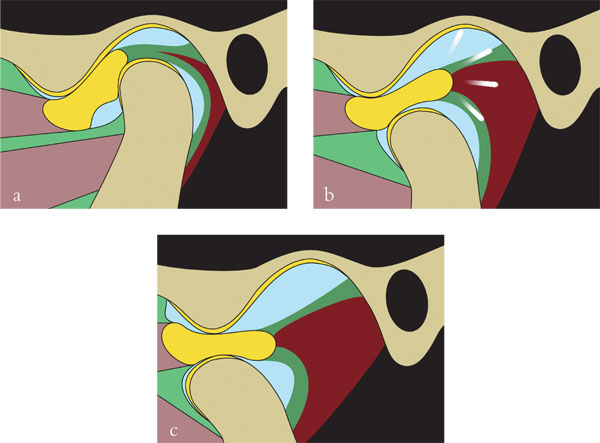
Fig 7-1 Disc displacement with reduction. (a) Disc displaced anteriorly or medially or both when in ICP. (b) On opening, the disc clicks back into place. (c) The disc remains in place until maximum opening but slips off the condyle again during closing.
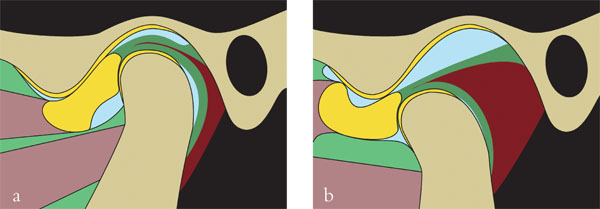
Fig 7-2 Disc displacement without reduction. (a) Disc displaced anteriorly or medially or both when in ICP. On opening, the disc does not go back into place but blocks condylar movement. (b) Maximum opening is often restricted, especially during the acute phase. The trapped disc may also cause mandibular deviation to the affected side.
Diagnoses from two or even all three of these main groups can occur together. The patient featured in the DVD video had TMJ tenderness on palpation, muscle tenderness in five locations, no limitation of jaw opening and an intermittent click on protrusion. The patient was suffering from myofascial pain. Although there was a click, it was non-reproducible and in all probability did not represent disc displacement with reduction. In relation to Group III, the patient had arthralgia (pain from the joint) but there were no clinical signs of arthrosis or arthritis. Therefore, in summary, the patient was diagnosed as having myofascial pain and arthralgia of the right TMJ.
Forms adapted to simplify the RDC for routine clinical care are available at www.ncl.ac.uk/dental/AppliedOcclusion/. These are recommended as a guideline for examination and diagnosis prior to undertaking complex and expensive treatment in cases in which there is any history of TMD.
Screening for TMD in Patients with Extensive Restorative Treatment Needs
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


