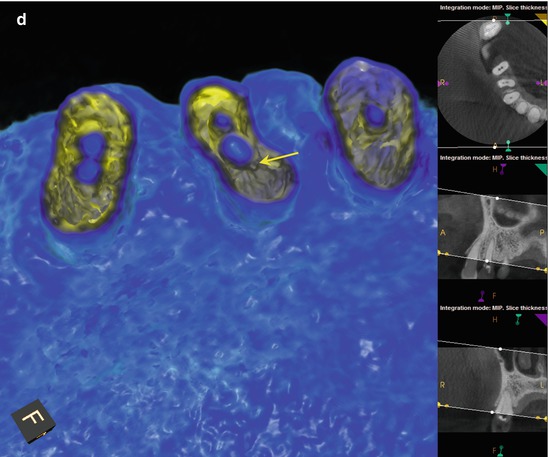
Fig. 5.1
(a, b) Preoperative radiographs reveal dystrophic obliteration of the canal spaces in tooth #5. Access and instrumentation was performed on #4, but only the buccal canal in #5 could be located. (c) An intra-treatment CBCT disclosed the location of the palatal canal 1 mm palatal and mesial to the area of ultrasonic excavation (white arrow). Note the kidney bean shape and mesial invagination of the root form not appreciated on the 2-D image. (d) A colorized axial section of the 3-D model demonstrates the instrumented canal diameters of #4 and the location of the palatal canal (yellow arrow) in #5. (e, f) Using a NiTi D11T spreader as an explorer, the palatal canal space is engaged and the orifice uncovered (red arrow). A small file will be inserted into the canal for verification and working length measurement. (g, h) Mid-obturation and final radiographs. Precise triangulation and accurate measurements guided the conservative excavation and location of this “calcified” canal in a critical abutment
5.2 Case #2
Description
The patient had RCT in teeth #2/3 approximately 14 months ago; both teeth have remained symptomatic. She is presenting for consultation.
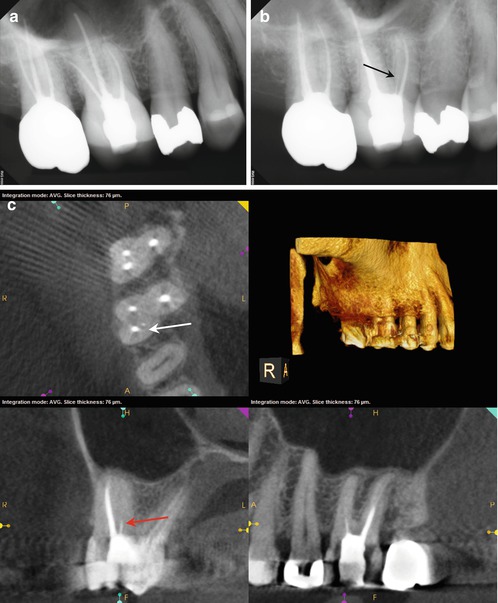
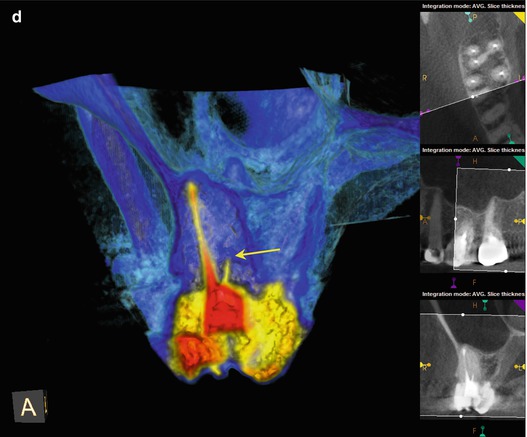
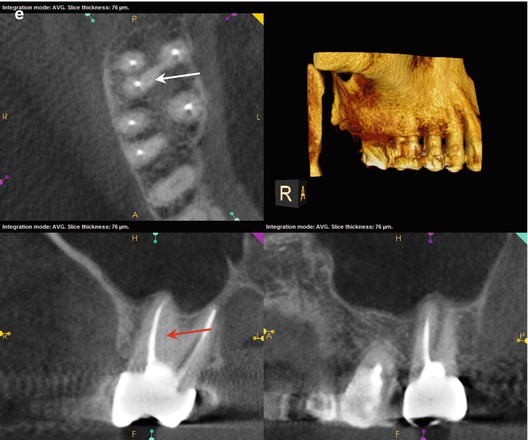
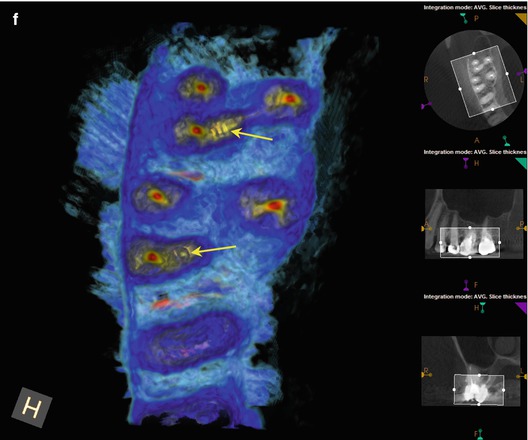
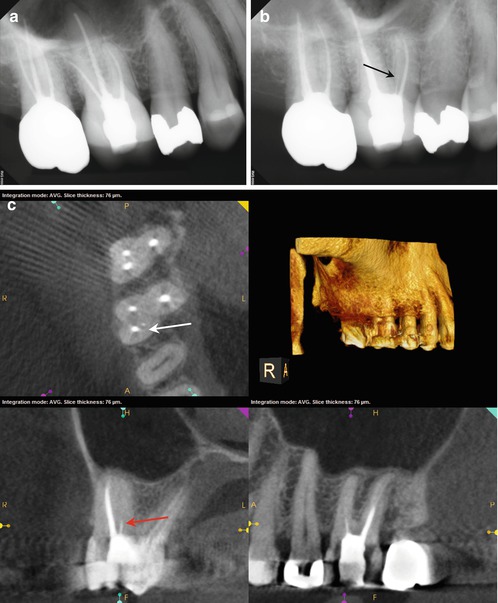
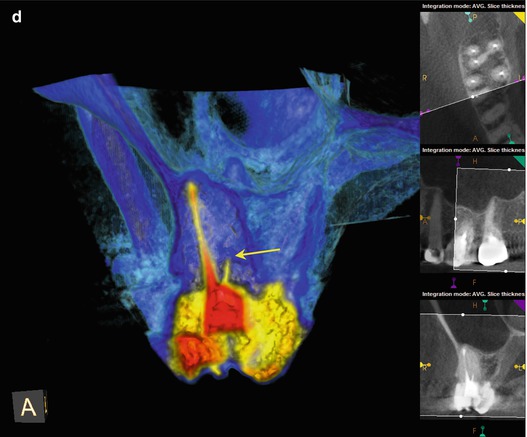
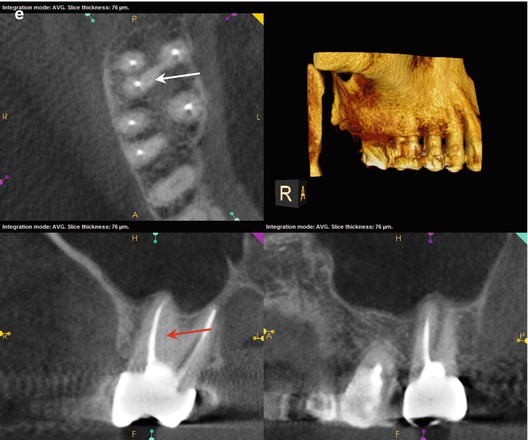
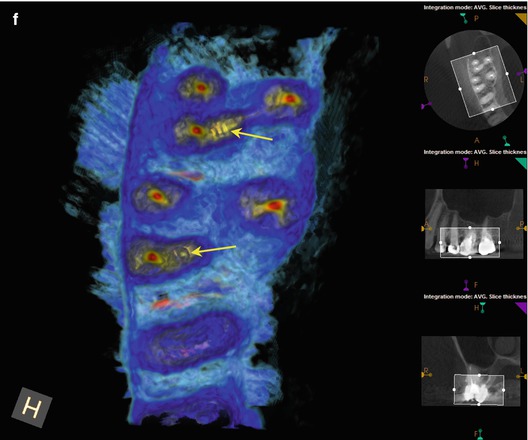
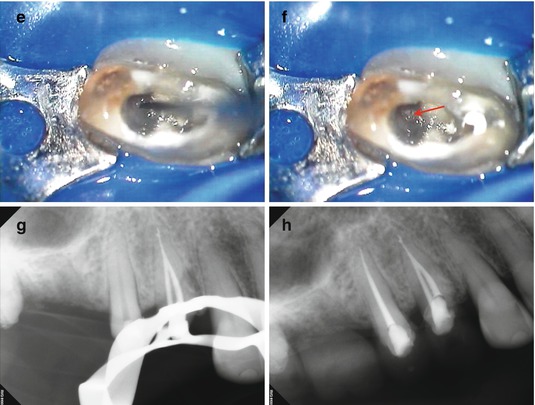
Fig. 5.2
(a, b) Preoperative radiographs disclose no obvious periapical pathology, but the obturation of the MB root in #3 appears to be off-center, and a thin radiopaque line is evident slightly distal to the filled MB canal (black arrow). (c) The axial section of #3 reveals a small high-density dot palatal to the MB1 canal (The white arrow points to a sealer tract from the previous root canal filling in the MB root). The location, as well as the configuration relative to the MB1 (red arrow), is suggestive of a sealer tract in the uninstrumented MB2 canal. (d) The colorized 3-D coronal section highlights the presence of the sealer in MB2, with a similar density to the root canal filling material (yellow arrow). (e) The axial section of #2 demonstrates a broad fusion of the MB and Palatal roots (white arrow), while the coronal section reveals a low-density line that is suggestive of MB2 (red arrow). (f) The colorized 3-D axial section discloses the sealer tract in #3 and an area of dentin density in the MB root of #2 that may contain the MB2 canal (yellow arrows)
5.3 Case #3
Description
The patient received RCT in tooth #18 approximately 3 years ago; the tooth was retreated 12 months prior to presentation. The patient has been symptomatic for the previous 2 years and recently reported a diagnosis of fractured tooth. The patient desires a second opinion.
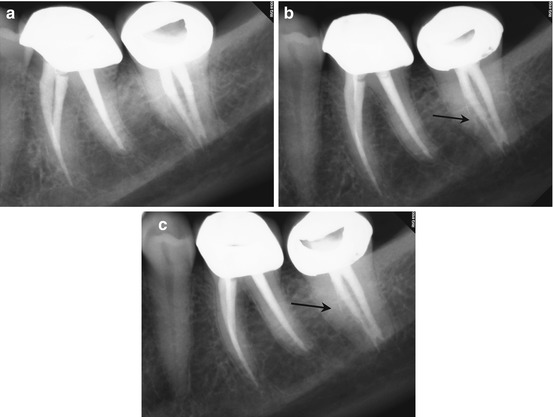
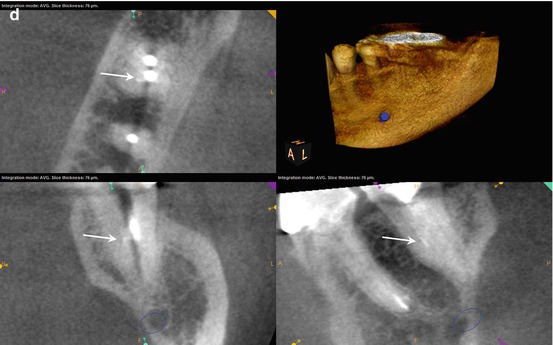
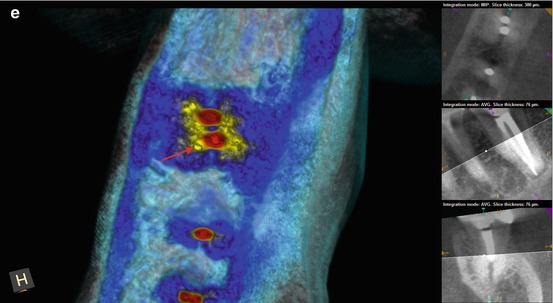
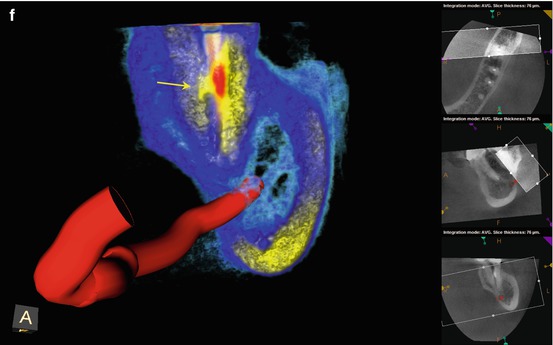
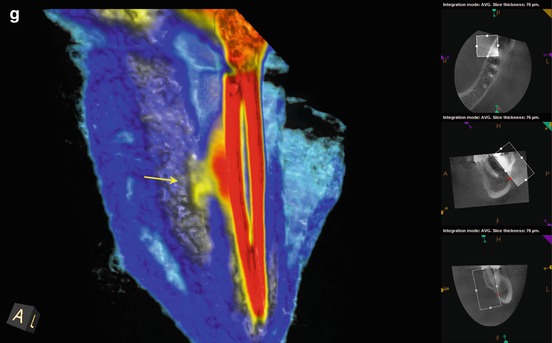

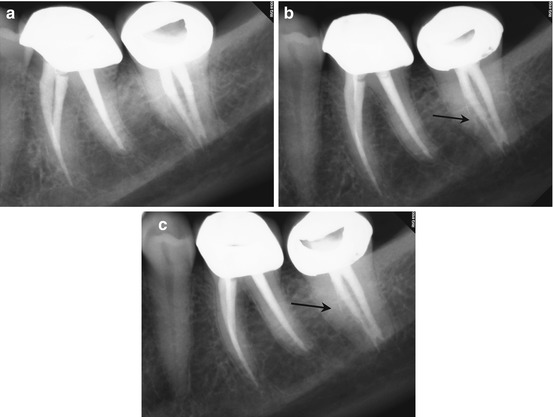
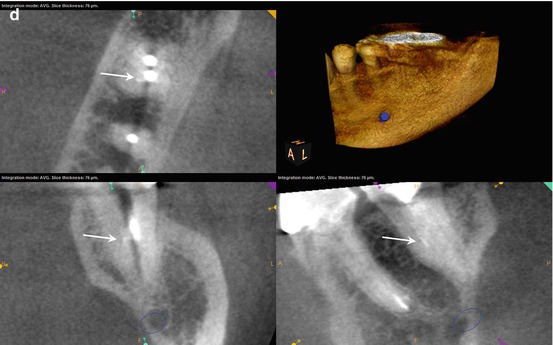
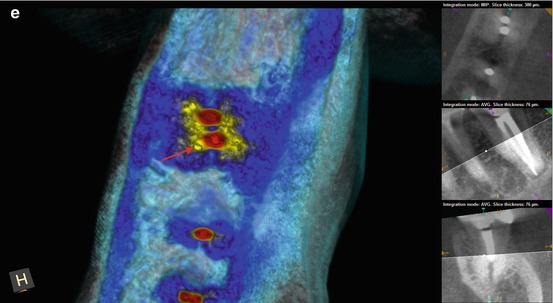
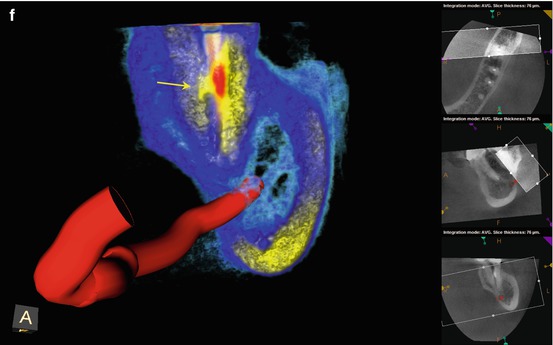
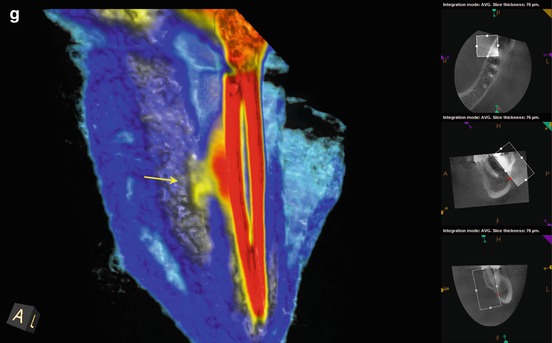

Fig. 5.3
(a–c) Preoperative radiographs from several different angulations fail to disclose a definitive diagnosis. However, closer examination of the magnified image suggests a thin radiopaque line from the mesial canal in two of the images (black arrows). The obturation is also off-center, again suggestive of additional canal spaces within the root. (d) The axial, coronal, and sagittal sections of the CBCT scan reveal a high-density dot or line, highly suggestive of sealer extruded into the uninstrumented ML canal space (white arrows). (e) The colorized 3-D axial section highlights the high-density object adjacent to the MB canal; the direction is on a line from the ML canal to the ML line angle of the root surface (red arrow). (f) The colorized 3-D coronal section reveals the bifurcation of the main canal, with sealer streaming into the lingual aspect of the bifurcation (yellow arrow). (g) A magnified view of the colorized coronal section with part of the sagittal aspect of the root removed. The detail of the bifurcation is displayed, and accurate measurements regarding depth can be obtained. It was ascertained from the scan that the depth from the floor of the chamber to the bifurcation entrance was 4 mm, on an angle toward the ML line angle of the mesial root. (h, i) The root canal filling (RCF) was harvested from the canal spaces, and the ML canal was located and negotiated (black arrow). A periapical radiograph was exposed to verify the complete removal of the RCF material. The canals were treated with Ca(OH)2 for 3 weeks; the patients’ symptoms subsided in 1 week and were absent at the completion appointment. (j, k) Right-angle and off-angle radiographs of the completed case, demonstrating the presence of three canals with multiple anastomoses between them
5.4 Case #4
Description
The patient was asymptomatic, but presented for evaluation of a “pimple on his gum.”
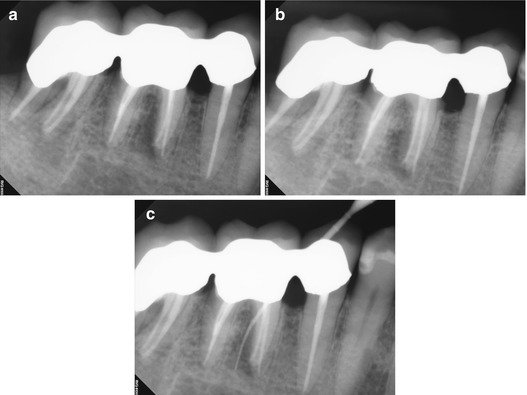
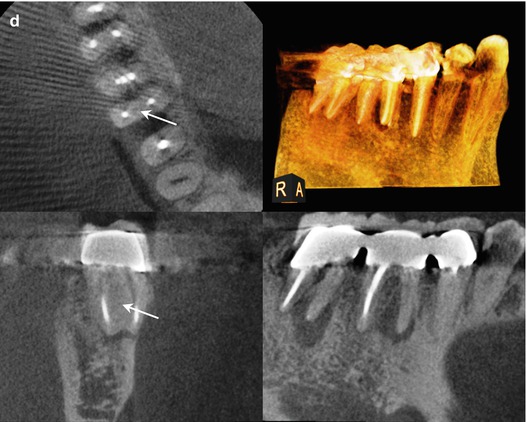
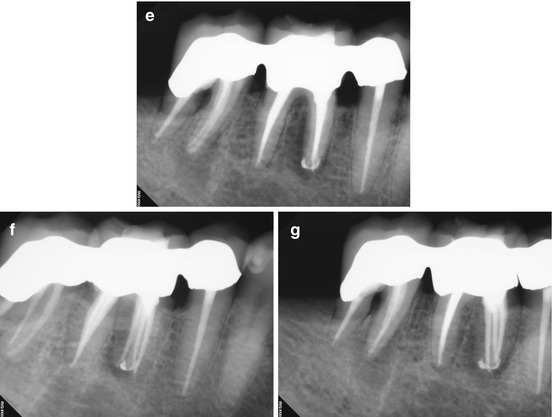
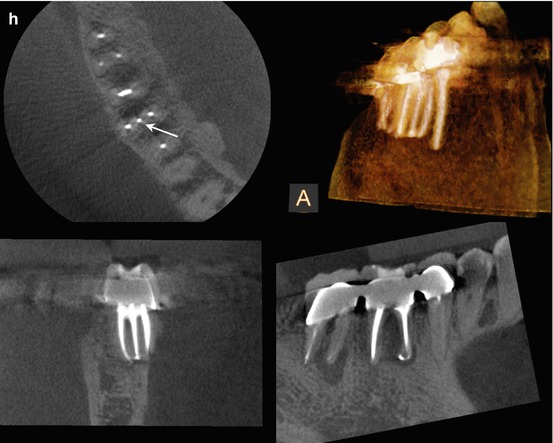
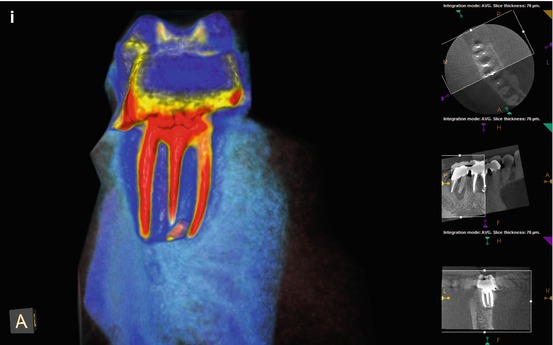
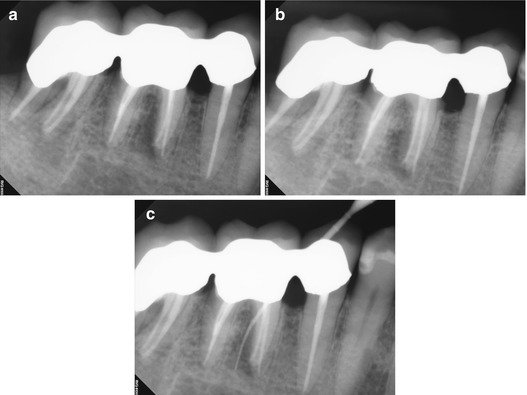
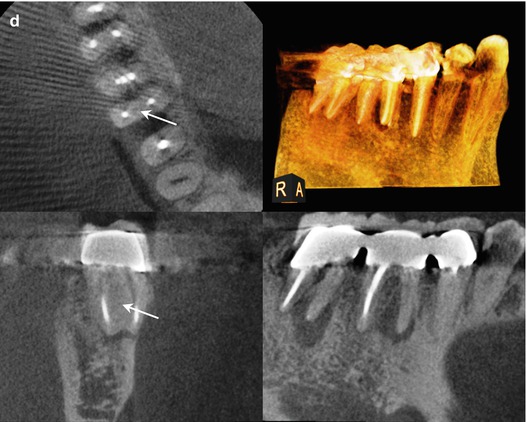
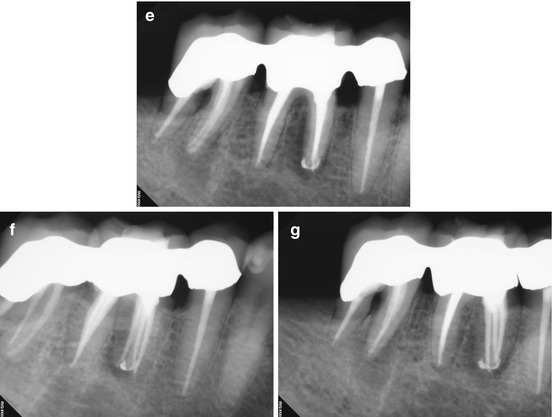
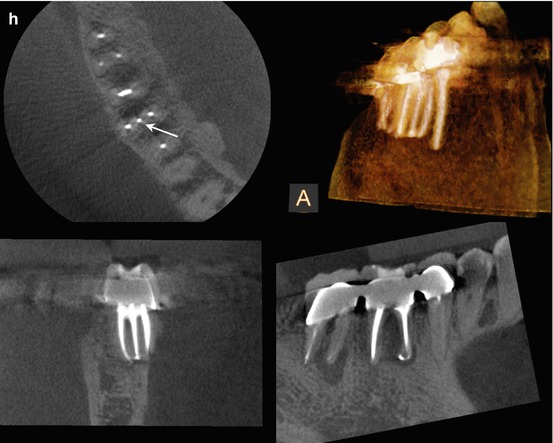
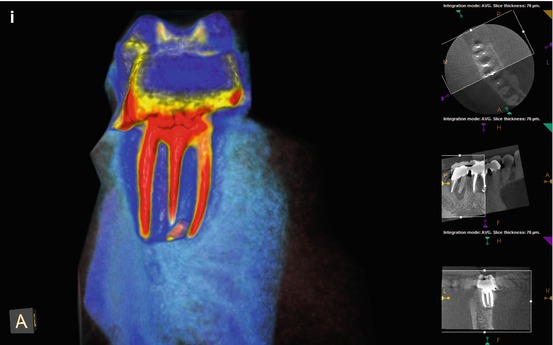
Fig. 5.4
(a, b) Right-angle and off-angle radiographs reveal PAP on the mesial root of tooth #30. There is also a suggestion of pathology on the mesial root of #31 as well. (c) Tracing the sinus tract revealed the source to be the apex of the mesial root of #30. Periodontal probing of the tooth was within normal limits, discounting a vertical root fracture as an etiology. (d) The axial and coronal sections of the CBCT scan were suggestive of a middle mesial canal: the distance between the MB and ML canals in the axial section measured 4.3 mm, exceeding the reported minimum span for a third negotiable space. Note also the PAP on the mesial root of #31, with the high probability of the same etiology. (e–g) Right-angle and off-angle radiographs reveal 3 separate canals and apical foramen in the completed mesial root. The retreated distal root also had 3 canals, but the final instrumentation created one large, scalloped ribbon canal configuration. (h) The axial and coronal sections demonstrate the span of the obturation in the mesial root and the confluence of the canals in the distal (The white arrow is pointing to the obturation of the Middle Mesial canal space in the axial section of the post-operative CBCT scan). (i) The colorized 3-D model highlights the comparative sizes between the retreated MB and ML canals and the primary instrumentation of the MM canal, terminating in 3 separate apical foramina
5.5 Case #5
Description
The patient presented with a diagnosis of symptomatic apical periodontitis, localized to a tooth that was endodontically treated 3 years previously.
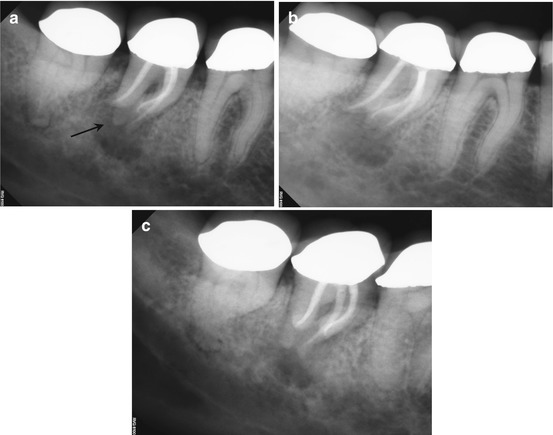
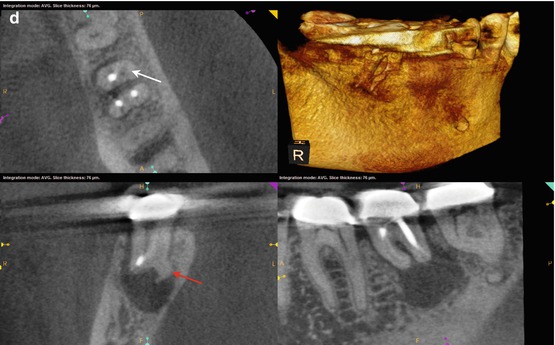
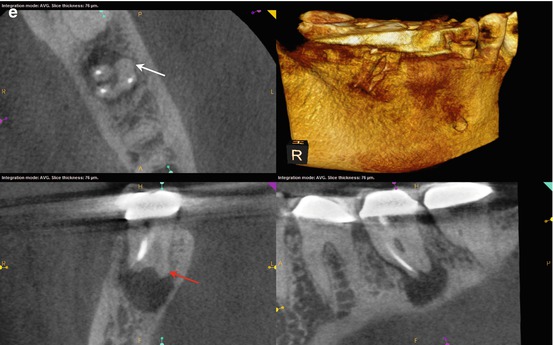
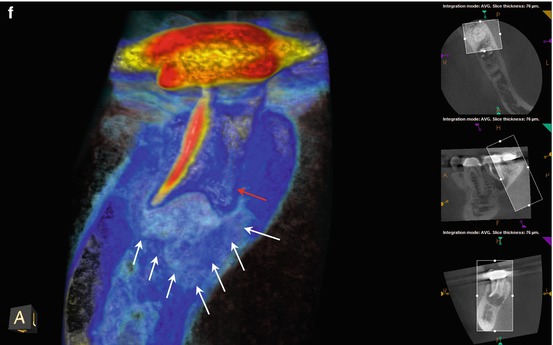
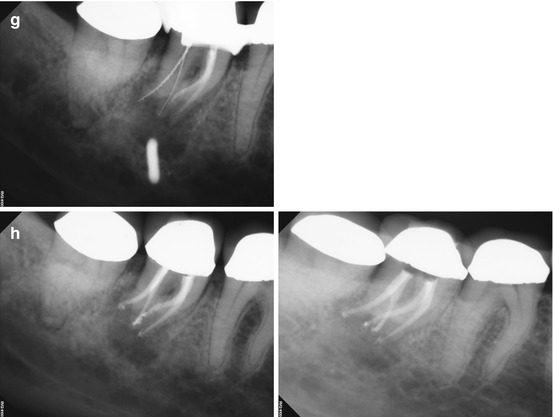
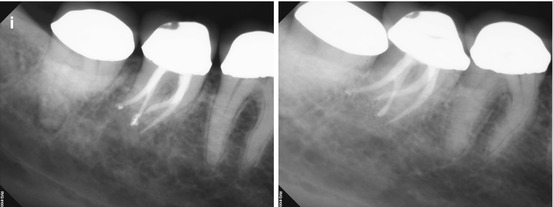
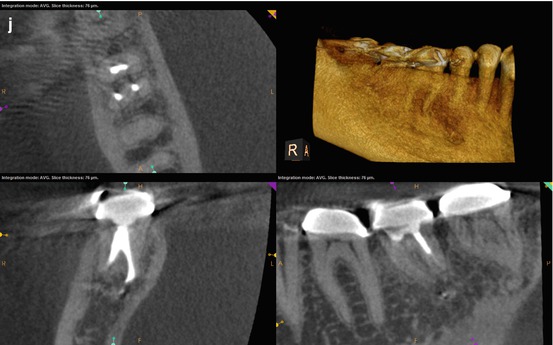
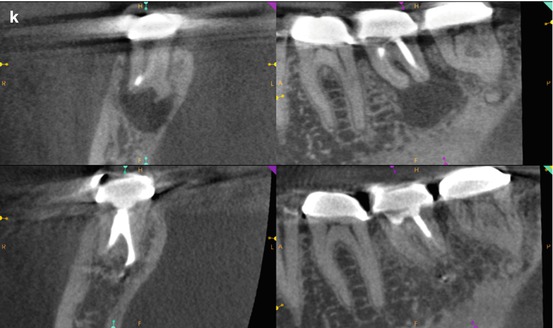
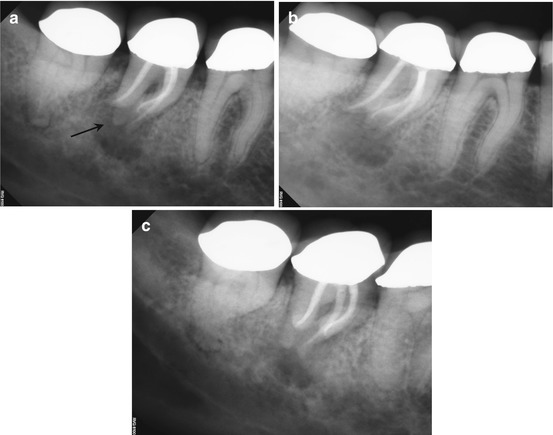
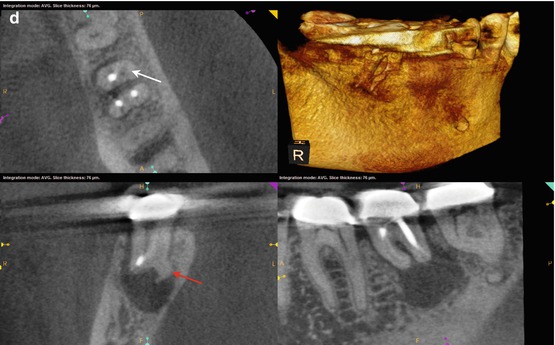
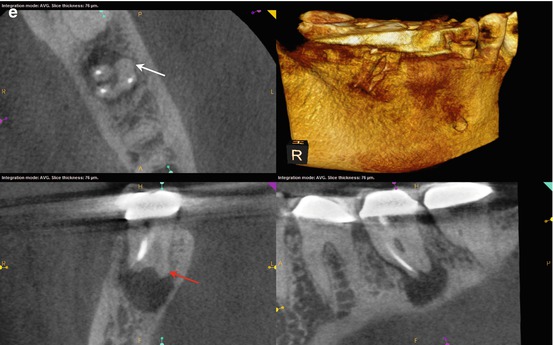
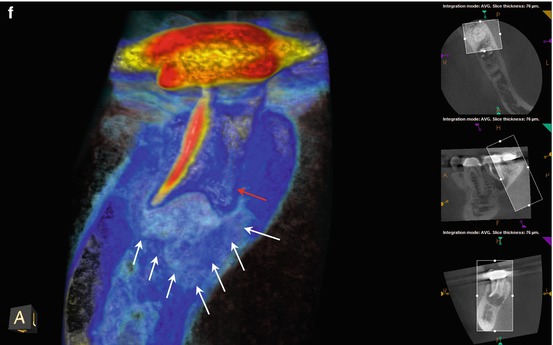
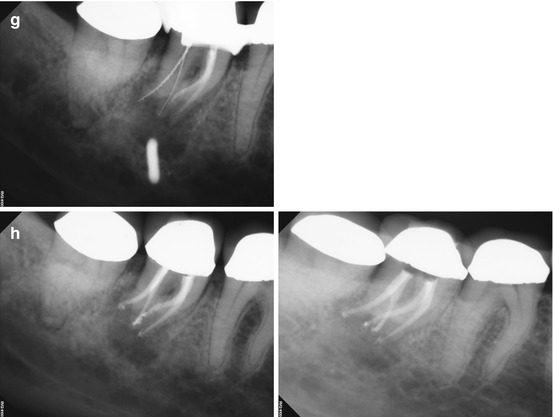
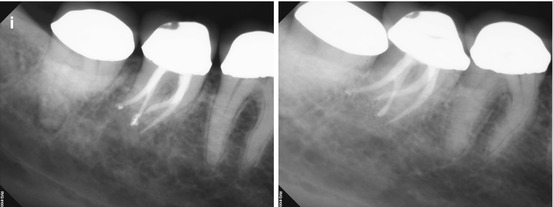
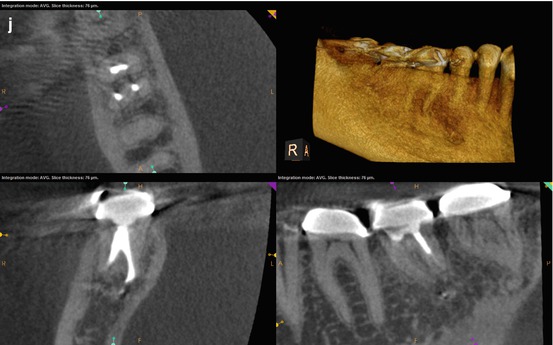
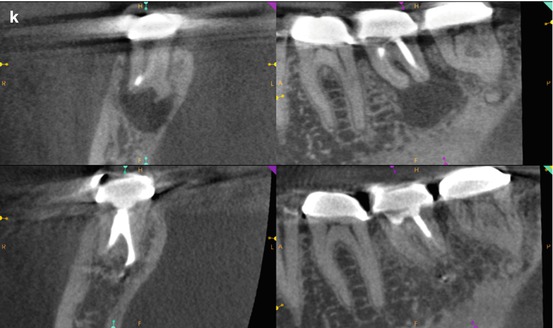
Fig. 5.5
(a–c) Right-angle and off-angle radiographs reveal a large PAA at the apices of tooth #30. There is a suggestion of an auxiliary root in (a) (black arrow), but its origin within the chamber and buccal-lingual position is not disclosed in any of the conventional images. (d) The axial view in the scan 2 mm apical to the CEJ confirms the presence of a second canal in the distal root, 2 mm lingual to the DB (white arrow). The coronal section reveals a sharp dilacerations of this root toward the buccal as it nears its terminus (red arrow); this change in direction will be explained in the next. (e) The axial view 2 mm from the terminus shows the DL root fusing with the ML root (white arrow), but their respective canal spaces do not join. At this level, the canal assumes a more linear path (red arrow). (f) The colorized 3-D coronal section highlights the juxtaposition of the DB and DL roots (red arrow) as well as the extent of the PA lesion and the thinning of the lingual cortical plate (white arrows). (g) Working length radiograph with files in the DB and DL canals. The gutta-percha is yet to be removed from the mesial canals (the radiopaque pin in the image is a 5 mm reference in the film holder). (h) Final radiographs of the completed retreatment. Note the overlapping of the mesial roots and the DL root. (i) 12-month recall radiographs; the lesion appears to be resolved, but overlying structures can mask underlying spaces. (j) 12-month CBCT scan demonstrates complete resolution after a thorough review of all the slices in all planes. This slice level corresponds to the location of the largest dimension of the lesion preoperatively. (k) A comparison of the preoperative (top) and 12-month postoperative (bottom) coronal and sagittal slices at almost identical levels, exhibiting complete resolution of the lesion
5.6 Case #6
Description
The patient presents for evaluation of tooth #2. It has been treated within the previous 9 months and has developed deep periodontal probing at the mesial aspect of the root. The tooth is mobile but not depressible in the socket. Initial micro-reflection of the area and inspection with the SOM did not disclose any vertical fracture.
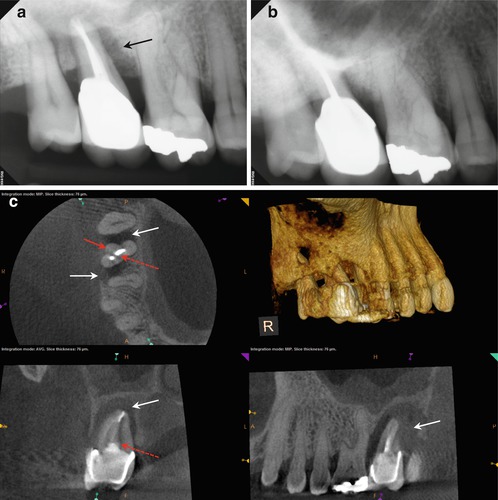
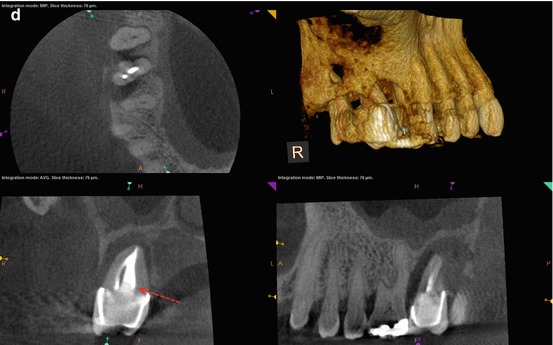


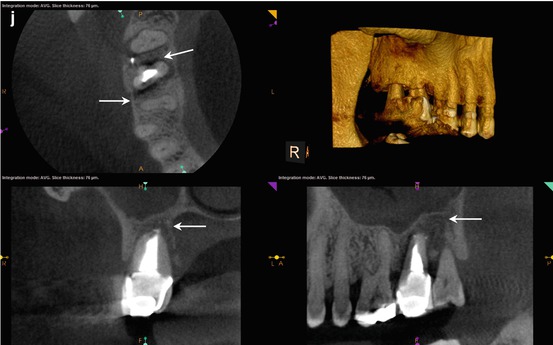
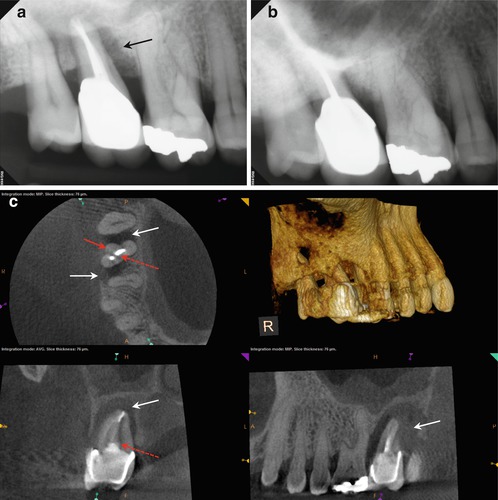
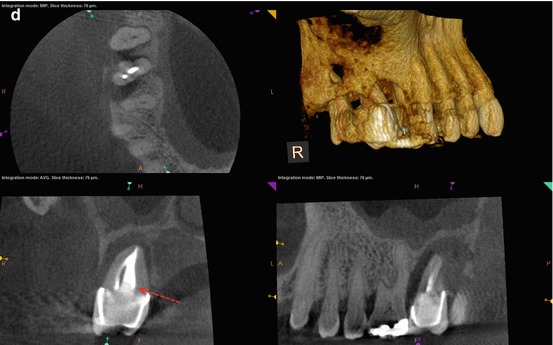


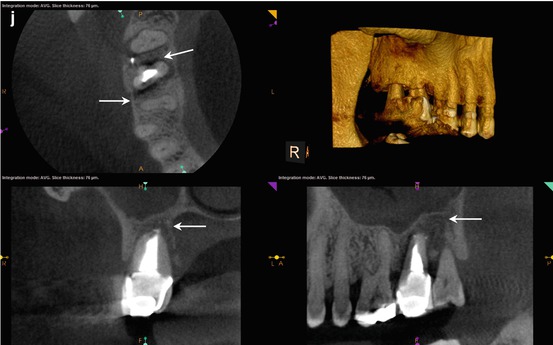
Fig. 5.6
(a, b) Preoperative radiographs demonstrating the extent of the bone loss at the mesial aspect of the root and the appearance of a 3-walled defect (black arrow). (c, d) The axial view reveals the extent of the bone loss at the mesial and distal aspects, with only the palatal wall intact (white arrows). The bulbous portion of the root at the distal suggests the location of the DB canal (red arrow). The coronal view shows the approximate location of the suspected perforation (red-dashed arrows); the invagination of the root form and the proximity of the obturative material were suggestive of this iatrogenic event. Reaccess of the canal spaces confirmed the presence of the DB canal and the perforation in the palatal canal. (e) Final posttreatment radiograph; note the multiple apical foramina in the mesial and distal aspects of the apical third of the root and the dramatic change in the width of the obturation. (f, g) Recall radiographs 6 months after initial treatment. The probing depth was reduced dramatically, and the tooth became more stable in the alveolus. Multiple apical foramina can be seen in the mesial and distal aspects of the apical third of the root. (h, i) 12-month recall radiographs reveal resolution of the mesial defect, although the PDL is widened and indicates possible occlusal trauma. The periodontal probing depths are within normal limits. (j) 12-month recall CBCT scan demonstrates approximately 80 % resolution of the presenting lesion, with a reestablishment of the buccal cortical plates and periapical bone matrix (white arrows)
5.7 Case #7
Description
The patient presents in pain in a tooth that has been previously treated 1 year ago. Her preliminary diagnosis is symptomatic apical periodontitis.
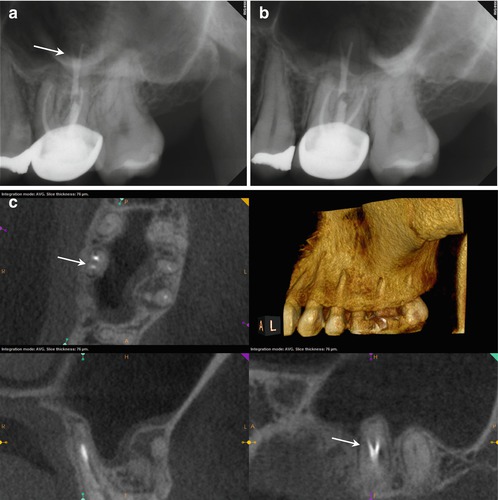
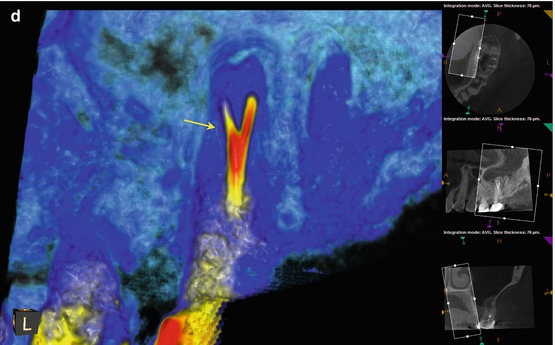

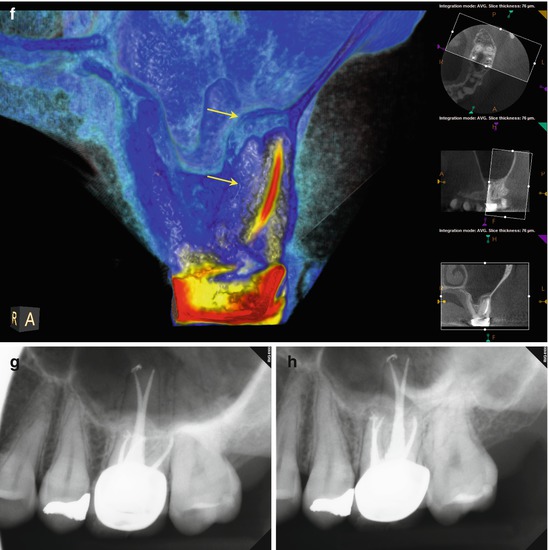

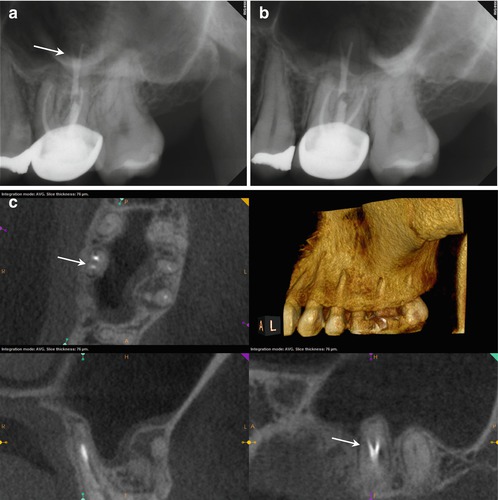
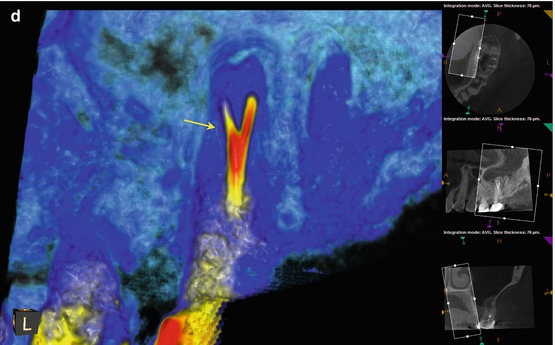

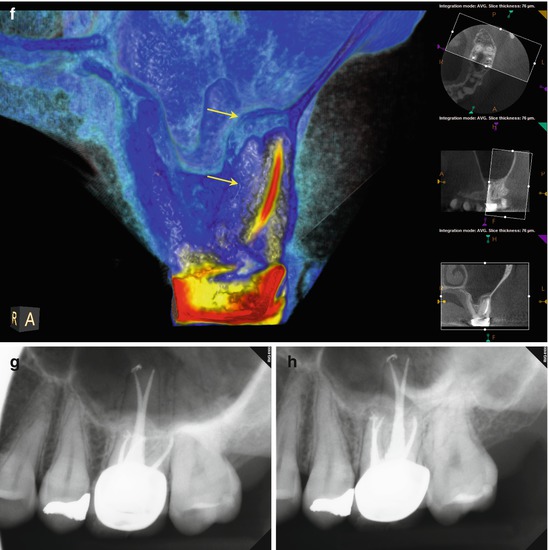

Fig. 5.7




(a, b) Preoperative radiographs from different angles reveal PAP on the MB root apex, as well as the suggestion of a bifurcation of the palatal canal (white arrow). The distal part of the split appears more dense than the mesial, implying that the mesial radiopacity is a sealer tract. (c) The CBCT scan shows definitively two separate canals in the palatal root. Accurate measurements place the level of the bifurcation 4.3 mm from the terminus of the distopalatal canal. The higher density spot in the axial and sagittal sections of the palatal root is the gutta-percha; the lower density object is the sealer tract (white arrows). (d) This colorized sagittal section has been magnified to ascertain the angle of the bifurcation; the deviation is less than 40°, so an appropriately angled instrument should be able to engage the orifice without difficulty (white arrow). When the angle of bifurcation is 60° or more, the dilaceration may be too abrupt to allow easy insertion of the file without additional coronal modification of the common canal space. (e) The axial section of the MB root demonstrates the eccentric placement of the MB root canal filling, indicative of the presence of an MB2 canal (white arrow). The coronal view of the same root suggests that the MB2 may, in fact, be a separate root fused to the MB1 (red arrow). (f) The colorized coronal section highlights the MB2 root and the distension/expansion of the floor of the maxillary sinus from the developing apical lesion (yellow arrows). (g, h) Final treatment radiographs presenting the obturation of the separate MB1/MB2 canals as well as the mesiopalatal and distopalatal canals. (i) 12-month recall radiograph: the lesion at the MB root appears healed, and the patient is asymptomatic
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


