Introduction
Not all adult Class III malocclusion patients are candidates for surgical correction. In patient assessment and selection, major issues remain regarding diagnosis and treatment planning. The purpose of this investigation was to ascertain whether adding a transverse parameter to a discriminant analysis could improve the classification of adults with Class III malocclusion into 2 groups of patients: those who can effectively be treated by orthodontic therapy and those who require orthognathic surgery.
Methods
Cephalograms, plaster casts, and extraoral photos of 69 adults with Class III malocclusion were analyzed. A discriminant analysis was performed to identify the variables that best separate the 2 groups.
Results
Stepwise variable selection resulted in a new, highly significant ( P <0.0001) model of 4 variables that provided the best discriminant function to distinguish between patients with and without indications for surgical correction. The resulting equation was the following: score = –10.988 + 0.243 * Wits + 0.055 * M/M ratio + 0.068 * NSAr – 0.589 * mand MLD. The percentage of patients correctly classified by this equation was 91.3%. The sensitivity was 0.92, and the specificity was 0.89.
Conclusions
In the discriminant analysis, the mandibular midline deviation as a transverse component was included. The addition of the transverse variable led to an improved model concerning the predictive value in Class III malocclusion patients with surgical requirements.
Class III malocclusion is a severe dentofacial anomaly. In most patients, there is no single feature responsible for the anomaly. Those with Class III malocclusion frequently show combinations of skeletal and dentoalveolar components. Moreover, there are complex interactions of genetic and environmental factors that can act synergistically, in isolation, or in opposition.
Compared with Class I subjects, several aberrant cephalometric measurements have been reported in Class III malocclusion patients, such as shorter anterior cranial base length, more acute cranial base angle, shorter and more retrusive maxilla, more obtuse gonial angle, excessive lower anterior face height, mandibular prognathism or excessive growth, more proclined maxillary incisors, and more retroclined mandibular incisors. Studies have also shown that no single morphologic feature indicates potential Class III development.
Kerr et al presented cephalometric criteria for classification of adult Class III patients to treat them objectively. The pretreatment lateral cephalograms of patients who had either surgical or orthodontic treatment of their Class III malocclusion were compared by using univariate statistical methods. Although significant differences were found between both groups in terms of ANB angle, maxillary-mandibular (M/M) ratio, mandibular incisor inclination, and Holdaway’s angle, in view of the complex interaction of skeletal and dentoalveolar parameters, it seems highly improbable that single variables could contain enough information to explain the anomaly. Furthermore, univariate statistical techniques were insufficient for diagnosis, treatment planning, and outcome prognosis. Therefore, recent studies have recommended a multivariate approach for analyzing the relationship between craniofacial structure and Class III malocclusion.
Based on a discriminant analysis (DA), Stellzig-Eisenhauer et al developed a formula to classify Class III adults into a group that is treatable solely orthodontically and a group that requires orthognathic surgery. DA is a multivariate procedure that has been especially designed to differentiate between 2 groups of subjects from the same population. In the orthodontic literature, most studies with multivariate statistics explored the potential of DA. The determining variables in the aforementioned study were the following: Wits appraisal (Wits), length of the anterior base (S-N), M/M ratio, and lower gonial angle (Go lower ). With the multivariate model, 92% of the study patients could be classified correctly. Consequently, the DA was highly significant ( P <0.0001).
In addition to these results, DA had previously been successfully applied to separate Class III patients from Class I subjects. Moreover, a DA was used to determine the prognosis for treatment outcome and relapse of orthodontically treated Class III patients.
In the study of Schuster et al, multivariate procedures were used to identify the dentoskeletal variables that provide the best differentiation between prepubertal children with Class III malocclusion who could be adequately treated by orthopedic or orthodontic therapy alone and those who required orthognathic surgery. The models were highly significant, classifying 93.2% to 94.3% of the patients correctly.
In the studies of Stellzig-Eisenhauer et al and Schuster et al, the Wits appraisal was the most predictive variable for differentiating between nonsurgery and surgery patients.
However, the results of the former studies should be regarded critically. Although multivariate techniques are better than univariate ones, their limitations include the following: for a sufficiently stable model that also applies to patients outside the study, a large sample size is a prerequisite, and the selection of parameters might not include all variables required to accurately differentiate the groups.
Stellzig-Eisenhauer et al could correctly allocate 97.7% of the solely orthodontically treated adults with Class III malocclusion. Those who required orthognathic surgery could be classified in 86.4% of the cases; only 2.3% of the nonsurgery patients were misclassified, but 13.6% of those who needed orthognathic surgery were misclassified. These findings led to the hypothesis that, especially in borderline surgical patients, additional factors are responsible for the necessity of surgical intervention. Because Class III patients frequently show skeletal deviations in the transverse dimension, the predictive value of the multivariate model might improve if transverse components are included.
Therefore, the purpose of this investigation was to apply DA to a new patient population to determine whether the addition of a transverse parameter could improve the correct classification of adults with Class III malocclusion into patients who can effectively be treated by orthodontic therapy and those who require orthognathic surgery.
Material and methods
To obtain as large a sample size as possible for a sufficiently stable model, our analysis was based on data from the Department of Orthodontics of the University of Wuerzburg in Germany and from 7 cooperative private practices. All patients were white adults ( Table I ) and met the inclusion criteria matching those of the original study : (1) Class III molar relationship, (2) negative overjet, (3) Wits appraisal ≤–2 mm, and (4) a negative difference between the ANB angle and the individualized ANB angle. Patients with craniofacial disorders such as cleft palate or craniosynostosis were excluded.
| Nonsurgery group | Surgery group | |
|---|---|---|
| Age (y) | ||
| Median | 23.6 | 24.2 |
| Mean | 27.6 | 26.2 |
| Maximum | 52.4 | 56.5 |
| Minimum | 18.0 | 17.9 |
The classification of the patients into nonsurgery and surgery groups was based on pretreatment records (plaster casts, cephalograms, and extraoral pictures). The patients were grouped by 3 independent and experienced orthodontists. The following treatment outcome criteria for both the surgery and nonsurgery groups had to be fulfilled: (1) stable occlusion in the sagittal, transverse, and vertical dimensions; (2) correct overjet and overbite; (3) proper incisal inclination; (4) satisfactory facial esthetics; and (5) long-term stability. The nonsurgery group consisted of 28 patients, and the surgery group consisted of 41 patients.
Because the lateral cephalograms were taken with different x-ray devices, all linear measurements were corrected by their respective magnification factors. One investigator traced all films with the original 21 landmarks ( Fig ) and digitized the data using appropriate software (fr-win, computerkonkret, Falkenstein, Germany).
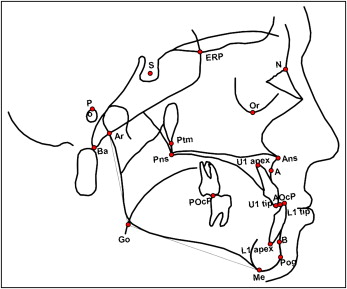
As in the previous study, the following linear, proportional, and angular measurements were calculated: S-N (anteroposterior length of the cranial base), PoOr-NBa (cranial deflection), ML-NSL (divergence of the mandibular plane relative to the anterior cranial base), NSAr (saddle angle), ArGoMe (gonial angle), SNB (anteroposterior mandibular position in the anterior cranial plane), Wits (length of the distance AO-BO; AO (intersection between a perpendicular line from Point A and the occlusal plane); BO (intersection between a perpendicular line from Point B and the occlusal plane); ANB (anteroposterior relationship of the maxilla and the mandible); ANB-ANB ind (difference between the ANB angle and an individualized ANB angle according to the formula ANB ind = –35.16 + 0.4 ∙ SNA + 0.2 ∙ ML – NSL ); M/M ratio (ratio of the anteroposterior length of the maxilla to the anteroposterior length of the mandible); ANPog (angle of convexity); 1/1 (angle between the axis of the maxillary and mandibular incisors); SNA (anteroposterior maxillary position to the anterior cranial plane); and NL-NSL (inclination of the palatal plane in relation to the anterior cranial base).
Thirty-five films were selected randomly, retraced, and redigitized by the same examiner independently on 2 separate occasions, 2 weeks apart. The method error in locating and measuring was calculated as recommended by using the formula of Dahlberg :
∑d2
∑ d 2
is the sum of the squared differences between the first and second registrations of a pair, and n is the number of double registrations. Random errors ranged from 0.14 to 1.88 mm for the linear measurements and from 0.31° to 1.98° for all angular variables. Systematic error was tested at the 10% level of significance, as recommended by Houston, and no systematic errors were found.
In the study of Stellzig-Eisenhauer et al, a DA was used to identify the variables that best separated the patients who needed orthognathic surgery for correction from those who did not. In this regard, the discriminant function was based only on lateral cephalometric landmarks. Consequently, the skeletal transverse component of Class III malocclusion was not considered.
The investigation of Stellzig-Eisenhauer et al resulted in the following equation that gives a score for assigning a new patient to 1 group: score = –1.805 + 0.209 ∙ Wits + 0.044 ∙ S-N + 5.689 ∙ M/M – 0.056 · Go lower . The critical score was –0.023, which was the mean value of the group centroids of the 2 groups.
Thus, each Class III malocclusion patient with a score higher than the critical score can be treated successfully by orthodontic therapy alone. In contrast, each Class III patient with a more negative score than the critical score must be treated by combined orthodontic-orthognathic therapy.
In this study, a transverse parameter was additionally implemented (mandibular midline deviation, mand MLD). For this purpose, the degree of mand MLD was diagnosed by analysis of the pretreatment plaster casts as described by Schwarz (1936) and Grünberg (1912). This is a routinely used procedure in our pretherapeutic diagnostic evaluation. Here, the sagittal jaw relationship is determined involving all tooth movements. The differences between the Angle classes on both sides after reconstruction (Schwarz) unmask the mand MLD. To verify the finding of chin deviation, visible facial asymmetry was used. A mandibular deviation from the facial midline of at least 2 mm was evaluated as laterognathism.
Statistical analysis
The data analysis was performed by using SPSS PC+ (version 14.0, SPSS, Chicago, Ill). The arithmetic means, standard deviations, medians, minimums, and maximums were calculated for each variable and group ( Table II ).
| Nonsurgery group (n = 28) | Surgery group (n = 41) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Cephalometric variable | Mean | SD | Median | Minimum | Maximum | Mean | SD | Median | Minimum | Maximum |
| SNA (°) | 79.29 | 0.74 | 79.35 | 69.40 | 85.50 | 79.32 | 0.66 | 79.30 | 69.70 | 86.40 |
| SNB (°) | 78.80 | 0.65 | 78.15 | 71.50 | 85.10 | 83.00 | 0.79 | 82.30 | 73.90 | 93.80 |
| ANB (°) | 0.49 | 0.44 | 0.65 | –7.10 | 4.20 | –3.68 | 0.53 | –3.70 | –10.40 | 4.30 |
| ANB-ANB ind (°) | –3.75 | 0.28 | –3.45 | –7.00 | –1.20 | –7.52 | 0.36 | –7.50 | –14.30 | –2.90 |
| ANPog (°) | –0.51 | 0.54 | –0.15 | –9.10 | 3.80 | –5.27 | 0.62 | –4.90 | –12.50 | 4.40 |
| Wits (mm) | –4.56 | 0.30 | –4.50 | –7.70 | –1.10 | –9.22 | 0.49 | –9.50 | –18.90 | –3.00 |
| PoOr-NBa (°) | 32.28 | 0.64 | 32.60 | 23.50 | 37.60 | 31.81 | 0.53 | 31.60 | 22.40 | 41.40 |
| NSAr (°) | 127.06 | 1,20 | 127.20 | 112.70 | 137.60 | 121.83 | 0.78 | 123.10 | 111.00 | 130.70 |
| ArGoMe (°) | 126.69 | 1,10 | 128.20 | 111.30 | 136.40 | 128.25 | 1.35 | 127.30 | 111.70 | 148.90 |
| Go upper (°) | 51.29 | 0.75 | 51.35 | 44.00 | 61.20 | 52.00 | 0.68 | 52.00 | 42.10 | 62.60 |
| Go lower (°) | 75.40 | 1.02 | 74.60 | 65.60 | 85.40 | 76.25 | 1.17 | 76.00 | 59.90 | 92.00 |
| NL-NSL (°) | 9.26 | 0.99 | 8.90 | –4.30 | 22.40 | 7.60 | 0.50 | 8.20 | –0.10 | 14.30 |
| ML-NSL (°) | 34.51 | 1.03 | 34.65 | 23.40 | 45.10 | 32.42 | 1.50 | 31.70 | 8.90 | 54.60 |
| 1-NSL (°) | 102.95 | 1.12 | 102.50 | 92.40 | 114.30 | 107.83 | 1.18 | 107.90 | 91.30 | 123.30 |
| 1-ML (°) | 89.90 | 1.05 | 90.15 | 78.80 | 102.20 | 84.34 | 1.19 | 84.60 | 69.40 | 102.70 |
| 1/1 (°) | 132.64 | 1.55 | 132.50 | 109.20 | 149.50 | 135.42 | 1.48 | 134.40 | 116.10 | 159.30 |
| S-N (mm) | 66.18 | 1.21 | 66.50 | 46.00 | 76.00 | 68.70 | 0.76 | 68.00 | 61.00 | 80.00 |
| M/M ratio (%) | 92.71 | 1.35 | 93.25 | 78.90 | 109.00 | 81.26 | 1.20 | 80.20 | 68.50 | 102.70 |
| Mand MLD (mm) | 0.45 | 0.11 | 0.00 | 0.00 | 2.00 | 1.35 | 0.16 | 1.00 | 0.00 | 3.00 |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


