This article illustrates a new treatment system combining segmented wire and osseointegrated mini-implants for molar distalization without complex appliances. The procedures, advantages, efficacy, and indications for this method are discussed. Two patients whose treatment plans included distal molar movement and orthodontic mini-implant treatment were recruited. One patient required 1 molar to be uprighted, and the other needed molar distalization to regain space lost for the missing maxillary right second premolar. C-implants (diameter, 1.8 mm; length, 8.5 mm) were placed and, after 4 weeks of healing, were used as direct anchorage and indirect anchorage simultaneously for correcting the asymmetric Class II molar relationship. Few orthodontic attachments were necessary, and the teeth moved rapidly to the planned positions without detrimental effects on the occlusion. The combination of segmented archwires, minimum bonded attachments, and a partially osteointegrated mini-implant (C-implant) was a simple and effective treatment choice in distalization treatment.
Unilateral full-step Class II correction, with asymmetry in the maxillary arch, can pose a challenge for the orthodontist. Although various treatment modalities have been developed and used successfully over the years, many need intensive cooperation from the patient. Noncompliant mechanics can be complicated and cumbersome. Unilateral premolar extraction is usually an available treatment option but can result in arch skewing or displacement of the midline.
Headgears can be adjusted to provide a distalization force on the Class II side. Removable appliances designed to distalize molars have been advocated, but both approaches require much patient cooperation.
Fixed functional devices can provide a distalization force to the maxillary posterior teeth but also influence the mandibular dentition. Pendulum appliances and distal jets have been advocated and proven successful for molar distalization. However, there are disadvantages, including laboratory time and expense. Whereas these appliances incorporate design components to attempt to prevent anchorage loss, flaring of the anterior teeth and increased overjet usually take place to a significant extent. One negative sequela usually seen with these appliances as posterior teeth distalize is increased lower facial height because of clockwise mandibular autorotation.
In more recent years, treatment mechanics with skeletal anchorage combined with pendulum springs have been devised primarily for molar distalization. However, these biomechanical systems are somewhat complex and require significant laboratory time and expense. The distalization process is also delayed because of the waiting period for these palatal implants to achieve osseointegration. Sugawara et al demonstrated the distalization capability of a skeletal anchorage system involving titanium anchor plates. Although effective, the surgical placement of a miniplate is more difficult and invasive than that of a mini-implant. Park showed the possibility of full-arch distalization using mini-implants. However, these mini-implants acted as auxiliaries for continuous archwire systems during the whole orthodontic treatment.
We present 2 patients who had limited treatment incorporating unilateral molar distalization with skeletal anchorage. The skeletal anchorage was provided by a C-implant, introduced as a partially integrated mini-implant system (Cimplant, Seoul, Korea). These relatively simple treatment mechanics use direct or indirect anchorage to achieve efficient, bodily molar distalization, while minimizing undesirable vertical dimension changes.
The biomechanics of molar distalization with pushing mechanics use partially osseointegrated C-implants. A C-implant is composed of titanium grade V alloy; it is self-tapping and threaded. Each C-implant has 2 components: the screw part has a diamter of 1.8 mm, and the head part measures 2.5 mm in diameter. The head is inserted into the screw and tapped into place. Precise fit and friction retain the head during treatment. The screw surface is sandblasted large grit and acid-etched treated for optimal osseointegration except for the upper 2 mm that is in contact with soft tissues. Upper and lower structures are mechanically interoriented; this means that they can have many variations. Especially, the head part can have different lengths and different numbers of holes. According to the treatment objectives, the head part can be changed in midtreatment, without the need to remove the implanted screw. The 0.8-mm diameter hole of the head part can receive archwires ( Fig 1 , A ).
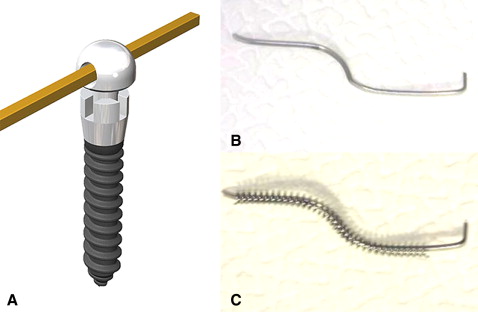
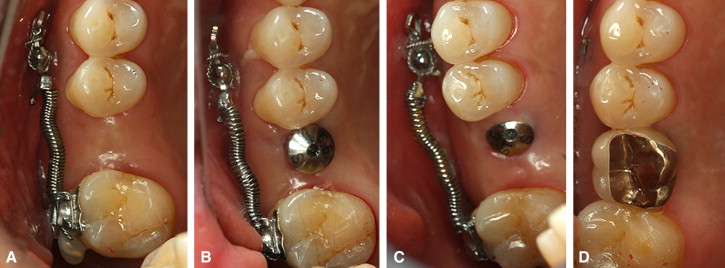
C-implants can provide absolute anchorage with the advantage of resistance to rotation force and high stability during force application. Direct anchorage can be obtained by using a segmental archwire with an open-coil spring to push the teeth independently ( Fig 1 , B and C ). Intrusive step bends are usually made to the segmented archwire to minimize the extrusion tendency during distalization. Indirect anchorage can also be established by attaching a wire ligature wire from the C-implant to a bracket anterior to the mini-implant. Mesial movement of anterior teeth can thus be prevented.
Case reports
Patient 1
A man, aged 42 years 7 months, had a chief complaint of loss of the maxillary right first molar and mesial inclination of the second molar. This condition followed the extraction 2 years previously of the first molar after a vertical fracture ( Figs 2 and 3 , A-C ). Pretreatment intraoral photographs showed bilateral Class I canine relationships, and a Class I molar relationship on the left side. There was a full-step Class II second molar relationship on the right side because of mesial drifting after the first molar extraction. There was a slight anterior open-bite tendency. The maxillary and mandibular midlines were coincident.

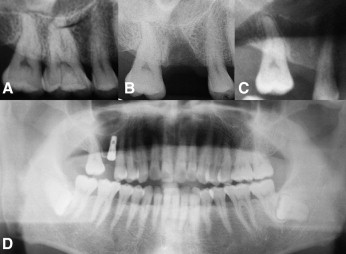
A panoramic radiograph at the initial examination showed mesial drifting and tipping of the maxillary right second molar ( Fig 3 , D ). An implant fixture had been placed into the missing molar position 2 months previously. The implant was close to the second premolar due to inadequate space for placement at the time of surgery ( Fig 3 , D ). The missing maxillary right first molar allowed mesial inclination of the maxillary right second molar into a full-step Class II second molar relationship. The treatment plan was to place a partially osseointegrated mini-implant that could endure heavy and dynamic forces in the interradicular space between the maxillary right first and second premolars. A segmental archwire with an open-coil spring was planned to move the second molar distally into a Class I second molar relationship.
A C-implant (diameter, 1.8 mm; length, 8.5 mm) was implanted in the interradicular space between the maxillary first and second premolars with a 45° apical angulation to the long axis of the teeth ( Fig 4 ). The angular placement of the mini-implant allowed for less chance of root contact because of greater interradicular space in the apical areas of the roots ( Fig 5 ).
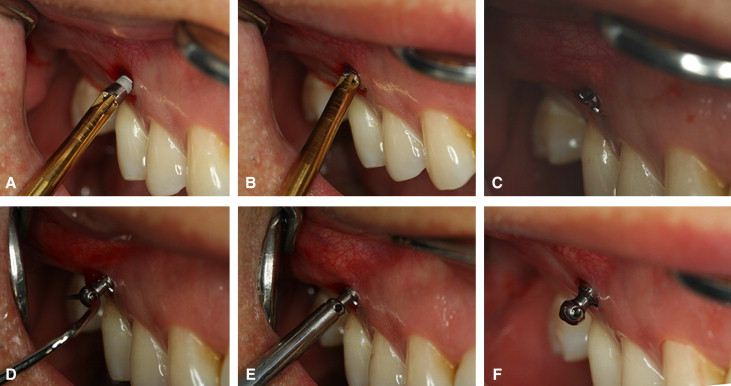

The segmental stainless steel wire (0.017 × 0.025 in) was placed into the hole of the C-implant head to the archwire slot of the second molar, and light orthodontic force (50 g) was applied with an open-coil spring immediately because that maxillary second molar showed fast mesial tipping tendency in a short period ( Fig 6 , A ). One month later, a crimpable hook was placed on the archwire to activate the open-coil spring, and intrusive step bends were made to the segmental archwire to prevent the extrusion tendency of the second molar ( Figs 6, B , and 7, A ). The patient was examined every 4 weeks to monitor progress ( Figs 6, C and D , and 7, B and C ). Selective grinding was done on the second molar to eliminate premature contacts as the tooth distalized. Two months later, the second surgery for the restorative implant was done. Four months later, distal movement was stopped, and the prosthesis was delivered.
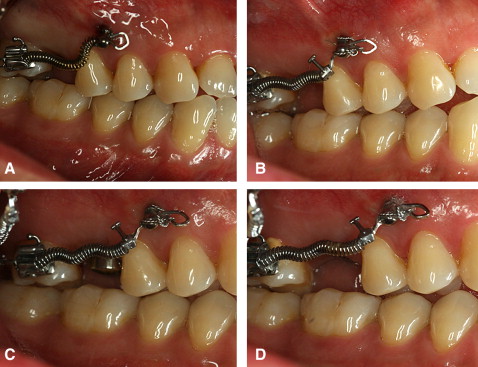
The final photographs and the panoramic radiograph show that adequate uprighting of the second molar provided sufficient space for an implant crown with normal dimensions ( Figs 7, D , 8, and 9 ). The patient’s preexisting occlusion was maintained. An anterior open-bite tendency remained, but a minimal increase in the anterior open bite was noted during treatment. In this minor tooth-movement case, bracketing was limited to the maxillary right first molar only ( Fig 10 ). The total treatment time was 3 months, after which the implant prosthesis was delivered in the regained space ( Fig 10 ). The C-implant was also stable during the total treatment and successfully removed by using topical anesthesia.



Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


