During patient treatment, the clinician needs to consider the operator needs, the restoration needs, and the tooth needs. This article discusses molar access and failures of endodontically treated teeth that occur not because of chronic or acute apical lesions but because of structural compromises to the teeth that ultimately render them useless. The authors believe that the current models of endodontic treatment do not lead to long-term success, and that the traditional approach to endodontic access is fundamentally flawed. This article introduces a set of criteria that will guide the clinician in treatment decisions to maintain optimal functionality of the tooth and help in deciding whether the treatment prognosis is poor and alternatives should be considered.
During patient treatment, the clinician needs to consider many factors that will affect the ultimate outcome. In simple terms, these factors can be grouped into 3 categories: the operator needs, the restoration needs, and the tooth needs. The operator needs are the conditions the clinician needs to treat the tooth. The restoration needs are the prep dimensions and tooth conditions for optimal strength and longevity. The tooth needs are the biologic and structural limitations for a treated tooth to remain predictably functional. This article discusses molar access and failures of endodontically treated teeth that occur not because of chronic or acute apical lesions but because of structural compromises to the teeth that ultimately renders them useless. What both authors have discovered in their respective practices through careful observations of failing cases and modes of failure, and observation of the truly long-term (decades) successful cases, is that the current models of endodontic treatment do not lead to long-term success. The authors want to coronally shift the focus to the cervical area of the tooth and create awareness for an endorestorative interface. This article introduces a set of criteria that will guide the clinician in treatment decisions to maintain optimal functionality of the tooth and help in deciding whether the treatment prognosis is poor and alternatives should be considered. This article is not an update on traditional endodontic access, as the authors believe the traditional approach to endodontic access is fundamentally flawed. Traditional endodontic access has been endodontic centric, primarily focused on operator needs, and has been decoupled from the restorative needs and tooth needs. Central to our philosophy is that balance needs to be restored to these 3 needs, which are almost always in conflict when performing complete cusp-tip to root-tip treatment.
Setting the stage for contemporary molar endodontic access
Modern clinicians must factor the unique and dramatically higher biting force of the molar tooth when designing the endodontic portion of the endo-endorestorative-prosthodontic (EERP) continuum. The occlusal forces created by the attachment position of the elevator muscles to the mandible generate occlusal forces that vary dramatically throughout the dentition, with light biting force in the front of the mouth to increasingly heavier forces at the back of the mouth. In physics, the mandible with its hinged access (the temporomandibular joint) is classified as a moment arm. The closer to the hinge, the higher the moment, or force, applied. The ability of the incisor to splay forward when loaded occlusally also comes into play when evaluating tooth stresses during occlusal loading. However, the molar absorbs a more vertical force and, therefore, a significantly higher net compressive force. When these 2 factors are combined (moment arm and splay), the overall compressive forces on the molar create a situation that requires a different set of rules for the calculation of ferrule, post and core design, resistance to fracturing, and (of utmost importance) endodontic access and removal of radicular dentin during endodontic shaping.
There are also different forces. The incisor must withstand milder, but more oblique, shearing forces. Most of the in vitro and in vivo research of post and core design has been conducted on maxillary incisor teeth, and attempting to extrapolate these findings to the molar tooth is not feasible. Placing a post in a round, husky maxillary anterior root and subjecting it to mild shearing force has little relevance to placing a post in a delicate, ovoid root in a mandibular molar and subjecting it to heavy compressive force.
Box 1 presents a compelling argument for change, or, perhaps, a return to the pre-Schilder era of directed dentin conservation. Many people were hopeful that the promise of point number 1, the endodontic monoblock of bonded endodontic obturants, posts, and cores, could revitalize a hollowed-out tooth. This has not reached fruition. Most restorative dentists are unaware of point number 2. Most have always assumed that coronal composite restorations, especially those that are bonded to enamel, strengthen the crown of the tooth and prevent coronal fracturing. This common notion has created a false hope, as no such intracoronal splinting benefit exists. Point number 4 eliminates posts as a reconstructive asset in molars. Point 5 presents the troubling fact that altering the thickness of radicular dentin, especially in the ovoid and fluted root, predisposes the root to fracture. Yet the dentin in the endodontically treated tooth has virtually the same strength and moisture content as a tooth with intact pulp. Root fractures in endodontically treated teeth should be considered as iatrogenically generated, not because of any fault of the tooth. The authors have exhausted the means to reinforce the endodontically treated molar stump, and now realize that dentin is the key.
- (1)
The failure of the endodontic monoblock
- (2)
The failure of intracoronal splinting using adhesive dentistry
- (3)
The resurgence of partial coverage posterior restorations
- (4)
The recognition that molars do not benefit from placement of posts
- (5)
Crack initiation in stress tests of endodontically treated roots
Endodontic accesses are traditionally conservative to the occlusal/incisal tooth structure. However, with the changes that occur in restorative dentistry, this technique is unnecessarily restrictive for the operator and potentially damaging to the more critical cervical area of the tooth.
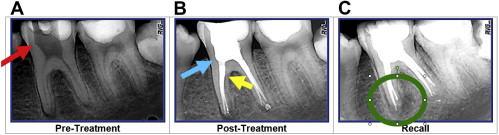
The following case is representative of a large percentage of endodontic accesses performed by general dentists and endodontists. This story is replayed each day in the United States and Canada. Fig. 1 shows a lower first molar of a 20-year-old woman. These young teeth are dangerously hollow to begin with. By the time that both of these well-meaning dentists had finished with the tooth, the molar was nearly worthless. The most important structures were so badly compromised that the tooth was permanently crippled.

The general dentist created the first access using fissure burs and with the type of dentin removal that is the standard today ( Fig. 2 A). The tooth was then reaccessed by an internationally recognized endodontist ( Fig. 2 B, C). This model for generous removal of pericervical dentin is common in many specialty practices. Eighteen months later, the lesion on the mesial root continues to enlarge ( Fig. 3 ). In the authors’ practices, such a tooth does not warrant endodontic retreatment. The wholesale loss of PCD has reduced the value of this tooth to the point that, when the tooth becomes symptomatic, extraction and replacement with an implant is a better option. In fairness to their patients, dentists must change the process, or make implants a first option instead of the eventual option. The new model of endodontic access is superimposed over the tooth in Fig. 4 .


In summary, directed dentin and enamel conservation is the best and only proven method to buttress the endodontically treated molar. No man-made material or technique can compensate for tooth structure lost in key areas of the PCD. Molar access, key to endodontic success, should also be considered as the key to restorative success and to long-term retention of the molar tooth. The primary purpose of the redesigned access is to avoid the fracturing potential of the endodontically treated molar. For expediency, molar fracturing can be described as retrograde vertical root fracture; midroot vertical root fracturing; oblique root/crown fracturing; and horizontal, oblique, and vertical coronal fracturing.
A new model for endodontic access
As endodontic access is deconstructed, it is crucial to understand the 5 catalyst forces that will change the future of endodontic access and coronal shaping. They are:
- 1.
Implant success rates
- 2.
Operating microscopes and micro-endodontics
- 3.
Biomimetic dentistry
- 4.
Minimally invasive dentistry
- 5.
Esthetic demands of patients.
In both of the authors’ practices, the endodontic goals and armamentarium have been in a constant state of flux for nearly a decade as we have collaborated to bring the EERP continuum to maturity. The goal is to satisfy the demands of the big 5 forces for change mentioned earlier. In so doing, we have come to realize that, when cutting endodontic access, our previous needs as dentists were often in conflict with the needs of the tooth.
Table 1 presents the hierarchy of needs to maintain optimal strength, fracture resistance, and several other characteristics needed for long-term full function of the endodontically treated tooth. Banking of tooth structure is key and is age- and case-sensitive. For example, in the case of the importance of pericervical enamel, the cementoenamel junction (CEJ) is an invaluable asset in the physiologically young molar. Margins of direct and indirect restorations placed on enamel have been shown to be more caries resistant than margins on dentin. The CEJ is also the most ideal vehicle to transition the stress from crown to apex.
| Value to the Tooth | Tissue Type |
|---|---|
| High | PCD |
| Undermined dentin | |
| The D 2 J | |
| Axial wall DEJ | |
| Cervical enamel in the physiologic young tooth | |
| Medium | Coronal enamel |
| Low | 2° dentin |
| No value or liability | 3° Dentin |
| Undermined enamel | |
| Inflamed pulp in mature teeth | |
| Cementoenamel junction in physiologically aged tooth or in root caries–prone patient |
Three-dimensional Ferrule
Three-dimensional ferrule is the backbone of prosthetic dentistry and has historically been described as axial wall dentin covered by the axial wall of the crown or bridge abutment. Ferrules are frequently used outside of dentistry. For example, in musical instruments, a ferule is a metal band used to prevent the ends of wooden instruments from splitting. Compression fittings for attaching tubing (piping) commonly have ferrules in them. A swaged termination type for wire rope or the cap at the end of a cane or umbrella are ferrules. In pool and billiards, the portion of a cue that tops the shaft and to which the leather tip is bonded is a ferrule. In fishing, the male and female joints that join one section of a rod to the next are known as ferrules.
Research varies on the minimal vertical amount required, but the range of absolute minimums is from 1.5 mm to 2.5 mm. The clinician must remember that buildup material, although necessary, does not count toward ferrules. A more comprehensive view of ferrules is needed, and is embodied in the term three-dimensional ferrule (3DF). There are 3 components of the new ferrule; first is the vertical component, which was described earlier, and is the traditional ferrule. The second component is dentin girth (thickness). The absolute minimum thickness is 1 mm; however, 2 mm is obviously a safer number. Girth becomes more important closer to the finish lines of the preparation. The thickness of the remaining dentin (the wall thickness) between the external surface of the tooth at the finish line and the endodontic access is more important apically. Further, progressing apically down onto the root surface in the endodontically treated tooth, the wall thickness can vary considerably and can become thin in places, especially if large coronal shaping or flaring was done during the endodontic treatment. Thus, axially deep finish lines on root structure can be extremely damaging to 3DF. Gutta percha is an exceptionally poor core material. The third component is total occlusal convergence (TOC) or net taper. TOC is the total draw of the 2 opposing axial walls of the prepared tooth to receive a fixed crown. A net taper or TOC of 10° requires 3 mm of vertical ferrule; a TOC of 20° requires 4 mm of vertical ferrule. Deep chamfer marginal zones, common with modern porcelain crowns, typically have a net taper of 50° or more, and therefore many modern esthetic margins lose a millimeter or more of their original potential 3DF at the crown margin interface. In short, typical modern porcelain crown prep has less 3DF than the corresponding gold crown prep. Hence, the need for directed dentin conservation during endodontic access becomes even more crucial, and, at the same time, the volume of dentin removed in the axial direction should be questioned in the modern era of high-strength zirconia core crowns that actually allow minimal axiomarginal reduction. In certain case types and finish line designs, the degree of apical placement of the finish line can affect the ferrule quality, as mentioned earlier. Light axiomarginal reduction coupled with apically placed finish lines and a nonzero-degree emergence profile of the restoration can provide high 3DF. The concept of 3DF incorporates an interplay between these factors that, in sum, indicate the true ferrule quality.
Undermined Enamel Versus Undermined Dentin
Because undermined enamel has not been shown to be strengthened by resin restorations, it becomes a liability because of fracture potential, poor C factor, and as a physical and visual obstruction to the endodontic operator. Conversely, because dentin acts as a trimodal composite, it can be of great value to the tooth whether the undermined dentin occurs naturally, such as the soffit, or from previous restorative/endodontic treatment. It is important to clarify that the act of purposely undermining dentin for mechanical retention of restorative materials or when using round burs in endodontic access is no longer indicated in contemporary restorative and endodontic dentistry. Enamel is essentially a crystalline structure and is therefore naturally supported 100% by dentin. Dentin, by contrast, is a multilevel composite that can stand alone and acts ideally as a semirigid pipe.
PCD
PCD is the dentin near the alveolar crest. Although the apex of the root can be amputated, and the coronal third of the clinical crown removed and replaced prosthetically, the dentin near the alveolar crest is irreplaceable. This critical zone, roughly 4 mm above the crestal bone and extending 4 mm apical to the crestal bone, is important for 3 reasons: ferrule, fracturing, and dentin tubule orifice proximity from inside to out. The research is unequivocal; long-term retention of the tooth and resistance to fracturing are directly related to the amount of residual tooth structure. The more dentin is kept, the longer the tooth is kept.
A new model for endodontic access
As endodontic access is deconstructed, it is crucial to understand the 5 catalyst forces that will change the future of endodontic access and coronal shaping. They are:
- 1.
Implant success rates
- 2.
Operating microscopes and micro-endodontics
- 3.
Biomimetic dentistry
- 4.
Minimally invasive dentistry
- 5.
Esthetic demands of patients.
In both of the authors’ practices, the endodontic goals and armamentarium have been in a constant state of flux for nearly a decade as we have collaborated to bring the EERP continuum to maturity. The goal is to satisfy the demands of the big 5 forces for change mentioned earlier. In so doing, we have come to realize that, when cutting endodontic access, our previous needs as dentists were often in conflict with the needs of the tooth.
Table 1 presents the hierarchy of needs to maintain optimal strength, fracture resistance, and several other characteristics needed for long-term full function of the endodontically treated tooth. Banking of tooth structure is key and is age- and case-sensitive. For example, in the case of the importance of pericervical enamel, the cementoenamel junction (CEJ) is an invaluable asset in the physiologically young molar. Margins of direct and indirect restorations placed on enamel have been shown to be more caries resistant than margins on dentin. The CEJ is also the most ideal vehicle to transition the stress from crown to apex.
| Value to the Tooth | Tissue Type |
|---|---|
| High | PCD |
| Undermined dentin | |
| The D 2 J | |
| Axial wall DEJ | |
| Cervical enamel in the physiologic young tooth | |
| Medium | Coronal enamel |
| Low | 2° dentin |
| No value or liability | 3° Dentin |
| Undermined enamel | |
| Inflamed pulp in mature teeth | |
| Cementoenamel junction in physiologically aged tooth or in root caries–prone patient |
Three-dimensional Ferrule
Three-dimensional ferrule is the backbone of prosthetic dentistry and has historically been described as axial wall dentin covered by the axial wall of the crown or bridge abutment. Ferrules are frequently used outside of dentistry. For example, in musical instruments, a ferule is a metal band used to prevent the ends of wooden instruments from splitting. Compression fittings for attaching tubing (piping) commonly have ferrules in them. A swaged termination type for wire rope or the cap at the end of a cane or umbrella are ferrules. In pool and billiards, the portion of a cue that tops the shaft and to which the leather tip is bonded is a ferrule. In fishing, the male and female joints that join one section of a rod to the next are known as ferrules.
Research varies on the minimal vertical amount required, but the range of absolute minimums is from 1.5 mm to 2.5 mm. The clinician must remember that buildup material, although necessary, does not count toward ferrules. A more comprehensive view of ferrules is needed, and is embodied in the term three-dimensional ferrule (3DF). There are 3 components of the new ferrule; first is the vertical component, which was described earlier, and is the traditional ferrule. The second component is dentin girth (thickness). The absolute minimum thickness is 1 mm; however, 2 mm is obviously a safer number. Girth becomes more important closer to the finish lines of the preparation. The thickness of the remaining dentin (the wall thickness) between the external surface of the tooth at the finish line and the endodontic access is more important apically. Further, progressing apically down onto the root surface in the endodontically treated tooth, the wall thickness can vary considerably and can become thin in places, especially if large coronal shaping or flaring was done during the endodontic treatment. Thus, axially deep finish lines on root structure can be extremely damaging to 3DF. Gutta percha is an exceptionally poor core material. The third component is total occlusal convergence (TOC) or net taper. TOC is the total draw of the 2 opposing axial walls of the prepared tooth to receive a fixed crown. A net taper or TOC of 10° requires 3 mm of vertical ferrule; a TOC of 20° requires 4 mm of vertical ferrule. Deep chamfer marginal zones, common with modern porcelain crowns, typically have a net taper of 50° or more, and therefore many modern esthetic margins lose a millimeter or more of their original potential 3DF at the crown margin interface. In short, typical modern porcelain crown prep has less 3DF than the corresponding gold crown prep. Hence, the need for directed dentin conservation during endodontic access becomes even more crucial, and, at the same time, the volume of dentin removed in the axial direction should be questioned in the modern era of high-strength zirconia core crowns that actually allow minimal axiomarginal reduction. In certain case types and finish line designs, the degree of apical placement of the finish line can affect the ferrule quality, as mentioned earlier. Light axiomarginal reduction coupled with apically placed finish lines and a nonzero-degree emergence profile of the restoration can provide high 3DF. The concept of 3DF incorporates an interplay between these factors that, in sum, indicate the true ferrule quality.
Undermined Enamel Versus Undermined Dentin
Because undermined enamel has not been shown to be strengthened by resin restorations, it becomes a liability because of fracture potential, poor C factor, and as a physical and visual obstruction to the endodontic operator. Conversely, because dentin acts as a trimodal composite, it can be of great value to the tooth whether the undermined dentin occurs naturally, such as the soffit, or from previous restorative/endodontic treatment. It is important to clarify that the act of purposely undermining dentin for mechanical retention of restorative materials or when using round burs in endodontic access is no longer indicated in contemporary restorative and endodontic dentistry. Enamel is essentially a crystalline structure and is therefore naturally supported 100% by dentin. Dentin, by contrast, is a multilevel composite that can stand alone and acts ideally as a semirigid pipe.
PCD
PCD is the dentin near the alveolar crest. Although the apex of the root can be amputated, and the coronal third of the clinical crown removed and replaced prosthetically, the dentin near the alveolar crest is irreplaceable. This critical zone, roughly 4 mm above the crestal bone and extending 4 mm apical to the crestal bone, is important for 3 reasons: ferrule, fracturing, and dentin tubule orifice proximity from inside to out. The research is unequivocal; long-term retention of the tooth and resistance to fracturing are directly related to the amount of residual tooth structure. The more dentin is kept, the longer the tooth is kept.
Sacrifice versus compromise
In the featured case, significant dentin was sacrificed to facilitate expedient and safe (avoidance of rotary file separation) instrumentation. No compromise was made in creating a direct pathway to the apices allowing copious irrigation and full vertical compaction of heated gutta percha, and yet the endodontic treatment was failing. Contrast that case with the tooth in Fig. 5 . There was a significant compromise when the dentist, 20 years ago, stopped removing dentin when he or she could not find the canal systems and filled less than half of the distal root. Yet the poor endodontic result is successful, the well-preserved PCD has buttressed the tooth, and the overall case is a still a success after 20 years. The authors have seen many cases of seemingly poor endodontic results that have defied current and conventional endodontic wisdom. Without detracting from the Schilder Objectives, the case types that seem to be lacking in the long-term are those with the appearance of high-quality endodontics, namely generous endodontic access, continuous taper, and large shape, facilitating the compaction of warm gutta percha.





