Simultaneous surgical repositioning of the maxilla and mandible has become routine for complex dentofacial deformities. An essential component of its predictability is the technique of preoperative model surgery. Improvements in model surgery technique (e.g., use of Erickson Model Block) and use of a vertical skeletal reference point intraoperatively have helped transform double-jaw surgery into a predictable treatment modality in orthognathic surgery.
The use of model surgery allows the surgeon’s planned osteotomies to be carried out ex vivo, thereby allowing for the fabrication of rigid interdental splints to be used intraoperatively to relate the teeth, and therefore the skeletal segments, into their planned positions during application of rigid internal fixation.
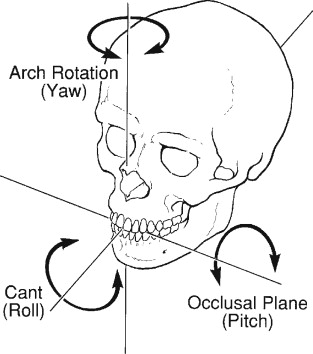
To carry out the desired surgical procedures for correction of a dentofacial deformity, the surgeon must decide the exact three-dimensional (3D) movements in all areas of the maxillary and mandibular osteotomies. This is decided at the patient’s final preoperative clinical examination. Assuming that both jaws are being repositioned and that the maxilla will be repositioned first, the surgeon must decide on specific 3D changes in the maxilla that will optimize the patient’s results, including facial balance, symmetry, facial soft-tissue drape (e.g., nasolabial esthetics, lip support), amount of exposed maxillary incisor at rest, and occlusal plane pitch, roll, and yaw ( Figure 16-1 ). The resulting changes in the position of the mandible and attached soft tissue must also be taken into consideration, because they will be determined completely by the occlusion with the repositioned maxilla and the resulting occlusal plane.
The decisions for maxillary repositioning are made with the final preoperative posteroanterior (PA) and lateral cephalograms available in order to determine the final 3D surgical plan. To enable the accurate transfer of this surgical plan to the patient at surgery, the planned movements are performed on dental casts, which must be accurately mounted on a semiadjustable articulator. The occlusal relationship that results between the repositioned maxilla and the unmoved mandible is recorded in acrylic as an interocclusal wafer known as the intermediate splint . This becomes the exact prescription for repositioning the mobilized maxilla to the stable mandible in all dimensions except the vertical, which is finalized during surgery with use of a skeletal vertical reference guide.
The importance of precision and accuracy in this model surgery procedure on the articulator-mounted dental casts cannot be overemphasized. With this in mind, we will outline the important steps and technical and theoretic considerations necessary for the accuracy of this model surgery, because the desired results are determined by its precision.
There are many ways to perform model surgery, and this chapter discusses the method that we use. It is a method most similar to the Eastman anatomically oriented model surgery technique. It takes into consideration that one of the jaws is always a stable reference for repositioning the opposite jaw, which is surgically mobilized. In isolated maxillary surgery the anteroposterior (AP) and transverse position of the maxilla is determined by its occlusal relationship with the mandible. Preoperative evaluation has shown this relationship to be acceptable. The vertical position is the only variable not controlled by the interocclusal splint and maxillomandibular relationship. Intraoperative autorotation of the maxillomandibular complex is performed to achieve the desired vertical change of the maxillary incisor. In isolated mandibular surgery, the mandibular position is dictated completely by the interocclusal splint and the maxillary position. In double-jaw surgery, some surgeons prefer to reposition the mandible first. In such cases the principles of model surgery are the same except that the mandible is moved the exact desired amount in all three dimensions, and the intermediate splint is fabricated with the repositioned mandible and the unmoved maxilla.
The goal of this chapter is to allow the reader to accurately transfer presurgical planning to real-life skeletal movements on the day of surgery. It is important to realize that orthognathic surgery is a series of orderly steps that begin in the early phases of orthodontic treatment planning, as illustrated elsewhere in this text, and culminate in postoperative patient management.
MOUNTING THE CASE
Once all preoperative records have been obtained and evaluated to create an operative plan, the next step is creating a model for simulation of surgical movements and fabrication of operative splints. Indications for semiadjustable versus hinge articulators has been a topic of some debate. There have been several absolute indications suggested for the use of an anatomic, semiadjustable articulator, which include asymmetry cases and cases in which fabrication of an intermediate splint is indicated (double-jaw surgery) and to ensure coincident facial and dental midlines. For straightforward single-jaw cases, a simple hinge articulator is sufficient for fabrication of the final surgical splint, assuming accurate preoperative clinical analysis (i.e., midline verification) has been performed.
Mounting a single-jaw case can be achieved on a simple hinge articulator once the final occlusion has been determined. The casts may be luted together with them related in the final occlusal relationship using yellow sticky wax. Plaster or stone is used to secure the casts to the hinge articulator. Once the plaster has dried, the wax is removed and the teeth may be separated. The hinge axis will accurately provide the new centric relation for single-jaw surgery. This method is possible when careful preoperative planning has determined that single-jaw-only surgery is indicated and the final occlusion will provide favorable outcomes with respect to facial and dental midlines ( Figure 16-2 ). From this point the surgical splint may be fabricated (to be discussed elsewhere in this chapter).

For double-jaw surgery or for cases in which movements may not be straightforward, mounting on a semiadjustable articulator is indicated. Accurate model surgery can be performed only if the point of origin precisely replicates the patient’s maxillomandibular relationship and the relation of maxillary arch to the condylar hinge axis. To achieve this, it is necessary to have a correct bite registration and facebow records. The finished product can be only as accurate as the starting point.
Although absolute precision with model surgery is an important aspect of orthognathic surgery, many potential sources of error may be introduced before the models are manipulated in the laboratory. Nattestad detailed the potential for inaccurate surgical outcomes as a result of errors in recording the center of mandibular rotation as performed with a facebow. He noted that this is accentuated in situations involving excessive autorotation of the mandible where mandibular rotation of 5 mm at the incisors produced 2 mm of horizontal malpositioning of the maxilla. Furthermore, several authors have focused on accurate recording of centric relation as a major instigator of inaccurate results. Minimizing these errors is an essential portion of the preoperative workup and should be performed by the surgeon conducting the operation.
Wolford and Galiano recently reported an alternative method of mounting the maxillary cast, pointing out the possible inaccuracies in the traditional facebow mounting. They proposed using the SAM occlusal plane indicator (OPI) device. Clinical and cephalometric measurements are used to mount the models on the articulator, without using a facebow. Follow-up clinical data are still needed to verify this technique’s superiority, although its rationale is very plausible.
Although the facebow transfer for accurate mounting of the maxillary cast is important, it is the accurate recording of centric relation that will have the most profound impact on the surgical outcome. This is essentially the starting point from which all movements will be based. If a patient has a large centric relation/centric occlusion (CR/CO) shift, this will become evident when the patient is supine and paralyzed on the operating room table; therefore it will need to be replicated in the clinical setting preoperatively and duplicated in the laboratory setup. The definition of centric relation is fairly controversial and has undergone changes over the past several years. It was initially noted to be the position in which the condyles are seated in the most “posterior superior” position; however, it is now described as the most “superior anterior” position in the glenoid fossa. Regardless of the definition, ultimately, the most important aspect is to replicate the most repeatable position without the assistance of the patient.
Several techniques have been described for manipulating the patient into centric relation and recording this position. Campos evaluated both the “chin point guidance” and the “swallowing techniques,” finding both to be accurate. Other authors have found reproducible results with “bimanual manipulation.” Once the patient has been guided into CR, it should be recorded in a material that is “dead-soft” and allows for passive manipulation with no occlusal deflection. Closure should stop with the first occlusal contact, and the material should be allowed to set for several minutes before removal in order to minimize distortion. Adrien and Schouver found that errors in mounting were directly proportional to the thickness of the material used to record CR and noted that the material should be as thin as possible between the molars.
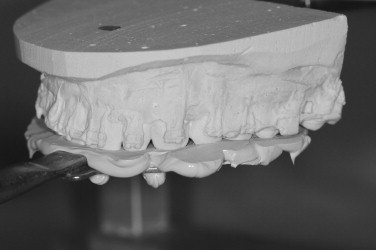
Using the previously obtained facebow record, the maxilla is mounted to the top portion of a semiadjustable articulator with mounting stone or plaster ( Figures 16-3 and 16-4 ). Mounting stone requires incorporation of less water than plaster and therefore appears to dry to completion sooner, allowing one to perform surgical movements and secure dry casts in place sooner. It is, however, more difficult to cut through, given its increased density. Regardless of the material used, adequate drying time is essential to allow for maximum accuracy. Also, the cone of the mounting material used should be sanded completely smooth over the entire extent of the vertical dimension so that marking the casts is clear and evaluating movements is accurate.
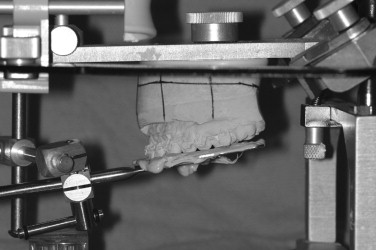
Once the maxillary cast is carefully mounted using the facebow as previously described, the centric relation record is used to relate the mandibular cast in the appropriate centric occlusion. It is important to ensure that there are no interferences between the record and the teeth that would prevent the cast from being fully seated. Also, the stop pin on the articulator should be set to the neutral position that will allow the upper arm of the articulator to parallel the Frankfort horizontal plane. Once the mandibular cast is mounted and the occlusal record removed, there should be tooth contact without moving the stop pin. This would indicate that the occlusal record obtained was accurately replicated. If there is a large gap requiring the stop pin to be adjusted before first occlusal contact, this is an indication that the casts were not fully seated into the occlusal record before mounting or that the material used to obtain the record was too thick. In this situation the centric relation record should be rechecked in the patient and the casts remounted. With model surgery and the intraoperative intermediate splints based primarily on occlusal relationships, verification of this record is crucial.
MARKING THE CASTS
Various methods for marking casts that allow for recording differences between preoperative and postoperative maxillary movements have been recommended. Any method that is useful to aid the understanding of the changes that can be expected and provide an idea of osteotomy appearance, bony overlap, or midline shift should be employed when marking the casts. We prefer to create horizontal markings that are parallel to the baseplate and therefore the Frankfort horizontal plane. The marks are placed on either side of where the proposed osteotomy will be located clinically. This marking is achieved by placing a marking pen flat on the table and rotating the cast to create a perfect horizontal line. Next, the pen can be placed on a 1-cm spacer (or stacked tongue sticks), and the second horizontal line is drawn.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


