Chapter 46 Midline laser glossectomy with linguoplasty: treatment of obstructive sleep apnea
1 INTRODUCTION
Obstructive sleep apnea (OSA) is a disorder characterized by repeated collapse of the pharyngeal airway during sleep.1 In adult OSA patients the site of obstruction is roughly evenly split between the palatal level and the hypopharyngeal level.2 Therefore, simultaneous oropharyngeal and hypopharyngeal surgery was conducted to treat multilevel obstruction in adult OSA patients. Uvulopalatopharyngoplasty (UPPP) is the most commonly utilized surgical modality for treating OSA with palatopharyngeal obstruction. Glossectomy has been used to reduce the volume of the tongue base, with resultant increase of the hypopharyngeal airway. Because of the lateral location of important neurovascular bundles in the tongue base, glossectomy is sometimes performed at the midline position to prevent major morbidity.3 The literature described two different surgical approaches.4,5 The transcollar technique to date has been less popular because it involves an open surgery with neck wound. Traditional transoral procedures are performed using CO2 laser.6 However, the inconvenience of using a large CO2 laser handpiece in a narrow oral cavity and the poor capability of hemostasis have limited the clinical application of this procedure.7 This chapter describes the outcomes of performing UPPP plus midline laser glossectomy (MLG) in severe OSA patients, with a specially designed handpiece comprising Nd:Yag laser fiber and suction tube being used to facilitate midline glossectomy.
2 PATIENT SELECTION
Indications for MLG were determined via anatomical structure (Friedman staging),8 but this study only enrolled patients with Friedman stage III or IV. Disease severity is not the main concern of this study. However, to date the procedures of MLG have been reserved for patients with severe OSA who cannot be adequately treated with continuous positive airway pressure (CPAP) therapy, owing to invasiveness and potential morbidities such as bleeding, airway compromise, dysphagia and taste disturbance.
3 SURGICAL PROCEDURE
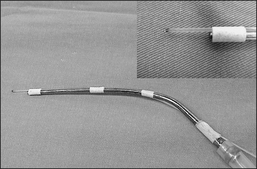
MLG was regularly performed in combination with UPPP for simultaneously enlarging the oropharyngeal and hypopharyngeal airway. MLG was implemented immediately following UPPP. An endotracheal tube was moved from the middle (UPPP position) to the right side and was re-fixed to the right mouth angle. None of the study cohort required tracheostomy. Nd:Yag laser was delivered via laser fiber which was fixed to a metallic suction tube with tape to create a novel excision-suctioned handpiece (Fig. 46.1). Moreover, Nd:Yag laser (Contact Laser™, Surgical Laser Technologies, Montgomeryville, PA, USA) (Fig. 46.2) was set in a continuous mode with a power of 10 watts. The tongue was pulled out as far as possible using MacGill forceps to expose its base (Fig. 46.3). A tongue blade was not used to facilitate prolapsing of the tongue base into the surgical field owing to previous experience showing that the tongue base wound made via this technique was always anterior to the position required. A rectangular midline section line of the dorsum of the tongue was marked, roughly 1 cm anterior to the papilla and extending posterior into the vallecula (Fig. 46.4). Laser cutting of the tongue base began from the left side of the tongue, ran across the dorsum of the tongue, and turned to the right side of tongue. After creating the excision border, teeth forceps were used to grip the dissected tissue to facilitate excision (Fig. 46.5). Bleeding from the lateral border of the wound was not unusual and was stopped by electrocautery. A rectangular wound in the tongue base (2 cm in width, 2–2.5 cm in length and approximately 1–1.5 cm in depth) was created after tissue removal (Fig. 46.6). Additional lingual tonsils were not removed since our previous investigation revealed that hypertrophic lingual tonsil, despite having an obscure laryngeal structure, did not contribute significantly to adult OSA.7 The laser char in the tongue base wound was carefully cleaned using a cotton soaked with H2O2. Finally, the wound was approximated in the tongue base using 2–0 Dexon via mattress suture (2–3 stitches) (Figs 46.7 and 46.8). This study demonstrates a case showing the area of the tongue base resected before and after MLG (Figs 46.9 and 46.10).
< div class='tao-gold-member'>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses