INTRODUCTION AND MIDFACE ANATOMY
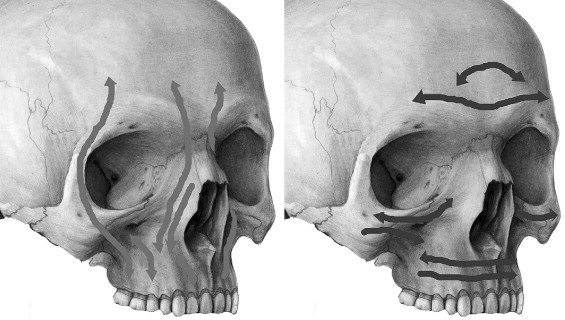
Facial fractures are predominantly afflictions of the young (20 to 40 years old) male (male to female ratio of 4 to 1). The number one cause of these injuries is motor vehicle accidents, followed by assault. Disruption of the facial skeleton distorts the patient’s appearance, and may compromise the function of several structures, including the masticatory system, ocular system, olfactory apparatus, and nasal airway. The facial skeleton is often described in terms of horizontal and vertical buttresses that are made up of thin segments of bone encased and supported by a more rigid framework of “buttresses.” The midface is anchored to the cranium through this framework.
Understanding the horizontal and vertical supports of the face is one of the most important concepts in craniofacial surgery. Comprehension of this concept enables the following:
- 1.
Aids in diagnosis and treatment planning of complex facial fractures.
- 2.
Simplifies the complex interrelationship of the facial bones.
- 3.
Provides links either directly or indirectly through another bone to the cranium or cranial base as a point of stable reference.
- 4.
Allows placement of screws and plates in regions of denser bone, and will restore facial profile, width, and height and establish support for the teeth and globes.
The buttress system absorbs and transmits forces applied to the facial skeleton. Masticatory forces are transmitted to the skull base primarily through the vertical buttresses, which are joined and additionally supported by the horizontal buttresses. The skull base itself is a major component of the horizontal support framework, although not classically thought of as part of the buttress system. When external forces are applied, these components prevent disruption of the facial skeleton until a critical level is reached, and then fractures occur ( Figure 14-1 ). In any rigid structure, fractures occur at areas of weakness and/or where stress concentrations occur. The areas where facial fractures tend to occur are weaker both collectively and individually, so that they tend to act like a “crumple zone” for the cranium and skull base when excessive force is absorbed. The classic fracture patterns described by LeFort in 1901 coincide with these areas of the facial skeleton, with fractures occurring through the junctions of horizontal and vertical buttresses, at suture lines, and in thinner segments of bone.
CLASSIFICATION OF MIDFACE FRACTURES
LEFORT CLASSIFICATION SYSTEM
René LeFort described the classic patterns of fracture in his 1901 work. LeFort’s experiments consisted of dropping cadaver skulls from several stories or striking them with a wooden club. He found three distinct fracture patterns, which he termed the linea minoros resistentiae. Simply stated, the LeFort I fracture separates the palate from the maxilla, the LeFort II separates the maxilla from the face, and the LeFort III results in craniofacial dysjunction.
The LeFort I fracture is a low transverse fracture that crosses the floor of the nose, pyriform aperture, canine fossa, and lateral wall from the maxilla, resulting in separation of the palate from the maxilla ( Figure 14-2 ).

The LeFort II fracture crosses the nasal bones on the ascending process of the maxilla and lacrimal bone and crosses the orbital rim. Only the LeFort II fracture violates the orbital rim. This proximity to the infraorbital foramen causes type II fractures to have the highest incidence of infraorbital nerve hypoesthesia. The LeFort II fracture extends posteriorly to the pterygoid plates at the base of the skull. Whereas a LeFort I fracture causes a low septal fracture, a LeFort II fracture results in a high septal fracture ( Figure 14-3 ).
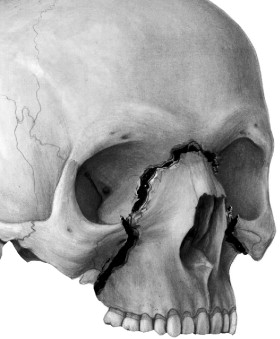
Finally, the LeFort III fracture traverses the frontal process of the maxilla, lacrimal bone, lamina papyracea, and orbital floor. This fracture often involves the posterior plate of the ethmoid. Because of their location, LeFort III fractures are associated with the highest rate of cerebrospinal fluid (CSF) leaks ( Figure 14-4 ).

LIMITATIONS OF THE LEFORT CLASSIFICATION SYSTEM
The LeFort fracture classification system, despite its shortcomings, is still the most accepted method to classify fractures and the location of osteotomies of the midface. However, recent studies have demonstrated that this classification system can be imprecise. The LeFort fracture system is deficient in addressing most midface fractures because they do not follow the simple LeFort pattern of fracture but, rather, assume a combination of LeFort fractures. In addition, most midface fractures have some degree of comminution and are complicated by fractures and displacement not addressed in the LeFort system. These midface fractures include palate, medial maxillary arch, dentoalveolar, and anterior maxillary fractures (orbit and zygoma).
OTHER CLASSIFICATIONS
Sagittal fractures of the palate occur in as many as 25% of all patients with fractures of the midface. They are not classified in typical LeFort fracture terminology. However, LeFort did describe traumatic injuries to the palate in his series of papers on maxillary fractures. Palatal fractures, as classified by Hendrickson et al, are divided into six types: I, anterior and posterolateral alveolar; II, sagittal; III, parasagittal; IV, para-alveolar; V, complex; and VI, transverse. Palatal fractures are associated with LeFort I fractures 100% of the time and with either LeFort II/III or mandible fractures 50% of the time.
There are many other classification systems for describing midface fractures. Donat et al described a system that divides the face into a matrix of vertical and horizontal beams, creating a lattice of 11 unilateral and 22 bilateral sites, to describe midface fractures. According to their preliminary data in 87 patients with midface fractures, this scheme allowed for accurate transcription and communication among physicians 98% of the time.
Another classification system is the Wassmund system. This system describes fractures as grades I to V. For example, a Wassmund I fracture is equivalent to a LeFort II fracture. A Wassmund IV fracture is equivalent to a LeFort III fracture. A Wassmund III fracture is characterized as a LeFort III fracture without inclusion of the nasal bones.
Manson described the facial fracture classification system based on CT findings. He divided fractures into low- and high-impact fractures. Most facial trauma results in complex forces applied to the skeleton, with fracture patterns rarely being simply a classic unilateral or bilateral LeFort pattern. Fractures can be isolated or occur in combinations that blur the division between classifications. Comminution fractures, crush injuries to the anterior maxillary wall, and zygomaticomaxillary complex fractures are very common and do not classically fit the LeFort classification.
For descriptive purposes, we will classify midface fractures into fractures that affect occlusion (such as LeFort fractures) and fractures with no effect on occlusion when displaced. The fractures that do not involve occlusion include orbit fractures, nasal fractures, zygoma fractures, frontal bone fractures, and combination fractures such as naso-orbito-ethmoidal fractures. This chapter will discuss LeFort fractures and naso-orbito-ethmoidal fractures, and the other topics will be discussed in different chapters.
CLASSIFICATION OF MIDFACE FRACTURES
LEFORT CLASSIFICATION SYSTEM
René LeFort described the classic patterns of fracture in his 1901 work. LeFort’s experiments consisted of dropping cadaver skulls from several stories or striking them with a wooden club. He found three distinct fracture patterns, which he termed the linea minoros resistentiae. Simply stated, the LeFort I fracture separates the palate from the maxilla, the LeFort II separates the maxilla from the face, and the LeFort III results in craniofacial dysjunction.
The LeFort I fracture is a low transverse fracture that crosses the floor of the nose, pyriform aperture, canine fossa, and lateral wall from the maxilla, resulting in separation of the palate from the maxilla ( Figure 14-2 ).

The LeFort II fracture crosses the nasal bones on the ascending process of the maxilla and lacrimal bone and crosses the orbital rim. Only the LeFort II fracture violates the orbital rim. This proximity to the infraorbital foramen causes type II fractures to have the highest incidence of infraorbital nerve hypoesthesia. The LeFort II fracture extends posteriorly to the pterygoid plates at the base of the skull. Whereas a LeFort I fracture causes a low septal fracture, a LeFort II fracture results in a high septal fracture ( Figure 14-3 ).
Finally, the LeFort III fracture traverses the frontal process of the maxilla, lacrimal bone, lamina papyracea, and orbital floor. This fracture often involves the posterior plate of the ethmoid. Because of their location, LeFort III fractures are associated with the highest rate of cerebrospinal fluid (CSF) leaks ( Figure 14-4 ).

LIMITATIONS OF THE LEFORT CLASSIFICATION SYSTEM
The LeFort fracture classification system, despite its shortcomings, is still the most accepted method to classify fractures and the location of osteotomies of the midface. However, recent studies have demonstrated that this classification system can be imprecise. The LeFort fracture system is deficient in addressing most midface fractures because they do not follow the simple LeFort pattern of fracture but, rather, assume a combination of LeFort fractures. In addition, most midface fractures have some degree of comminution and are complicated by fractures and displacement not addressed in the LeFort system. These midface fractures include palate, medial maxillary arch, dentoalveolar, and anterior maxillary fractures (orbit and zygoma).
OTHER CLASSIFICATIONS
Sagittal fractures of the palate occur in as many as 25% of all patients with fractures of the midface. They are not classified in typical LeFort fracture terminology. However, LeFort did describe traumatic injuries to the palate in his series of papers on maxillary fractures. Palatal fractures, as classified by Hendrickson et al, are divided into six types: I, anterior and posterolateral alveolar; II, sagittal; III, parasagittal; IV, para-alveolar; V, complex; and VI, transverse. Palatal fractures are associated with LeFort I fractures 100% of the time and with either LeFort II/III or mandible fractures 50% of the time.
There are many other classification systems for describing midface fractures. Donat et al described a system that divides the face into a matrix of vertical and horizontal beams, creating a lattice of 11 unilateral and 22 bilateral sites, to describe midface fractures. According to their preliminary data in 87 patients with midface fractures, this scheme allowed for accurate transcription and communication among physicians 98% of the time.
Another classification system is the Wassmund system. This system describes fractures as grades I to V. For example, a Wassmund I fracture is equivalent to a LeFort II fracture. A Wassmund IV fracture is equivalent to a LeFort III fracture. A Wassmund III fracture is characterized as a LeFort III fracture without inclusion of the nasal bones.
Manson described the facial fracture classification system based on CT findings. He divided fractures into low- and high-impact fractures. Most facial trauma results in complex forces applied to the skeleton, with fracture patterns rarely being simply a classic unilateral or bilateral LeFort pattern. Fractures can be isolated or occur in combinations that blur the division between classifications. Comminution fractures, crush injuries to the anterior maxillary wall, and zygomaticomaxillary complex fractures are very common and do not classically fit the LeFort classification.
For descriptive purposes, we will classify midface fractures into fractures that affect occlusion (such as LeFort fractures) and fractures with no effect on occlusion when displaced. The fractures that do not involve occlusion include orbit fractures, nasal fractures, zygoma fractures, frontal bone fractures, and combination fractures such as naso-orbito-ethmoidal fractures. This chapter will discuss LeFort fractures and naso-orbito-ethmoidal fractures, and the other topics will be discussed in different chapters.
IMAGING MODALITIES
Current options for midface imaging include plain film radiographs, computed tomography (CT), two-dimensional (2D) and three-dimensional (3D) reformatted computed tomography, magnetic resonance imaging (MRI), and ultrasound. Imaging modalities of the midface continue to evolve with the advent of better computer algorithms and higher resolution CT scanners. The ability of a particular imaging method to improve diagnosis and aid treatment-planning decisions will dictate which modalities are used in the future. Currently, surgeons show a subjective preference for the use of CT and 3D reformatted CT in maxillofacial trauma.
PLAIN FILM RADIOGRAPHS
The accuracy in using plain film radiography and clinical evaluation in situations of mandibular fracture has been well documented. However, with the advent of CT, plain film radiography no longer has much of a role in midface trauma. Superimposition of structures and lack of detail in comminution and soft tissue injuries make plain film radiology difficult to utilize. A submentovertex film in situations of isolated arch fractures may be the only instance in which a plain film may be adequate, and even then only as a postreduction film.
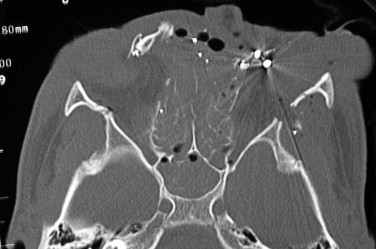
COMPUTED TOMOGRAPHY
The use of computed tomography for identification of fracture patterns of the midface is the standard of care. Since its advent in the 1970s, computed tomography has changed dramatically, offering multiplanar, high-resolution images that can be reformatted using computer algorithms to generate three-dimensional images.
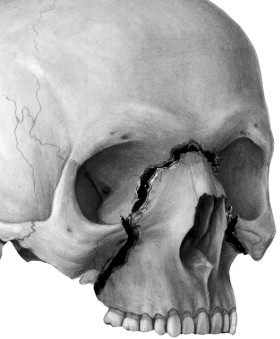
Both three-dimensional CT and two-dimensional CT have their own merits. Three-dimensional CT has been shown to be most advantageous in cases of severe facial trauma. Surgeons have identified its usefulness in predicting the need for immediate bone grafting and the need for external fixation secondary to extensive comminution ( Figure 14-5 ). It has been shown to have increased accuracy in the region of the vertical maxillary buttress. Additionally, 3D CT has improved visualization of horizontal fracture patterns, lateral translation of segments, rotation, spatial relationships, and fracture comminution. Nevertheless, 3D CT has not been shown to have an increased accuracy for identification of mandible fractures and has a decreased visualization of soft tissues and deep internal architecture of orbits and sinuses. Two-dimensional CT clearly has an advantage in diagnosis when injury involves the paranasal sinuses, orbital walls, or soft tissues ( Figure 14-6 ).

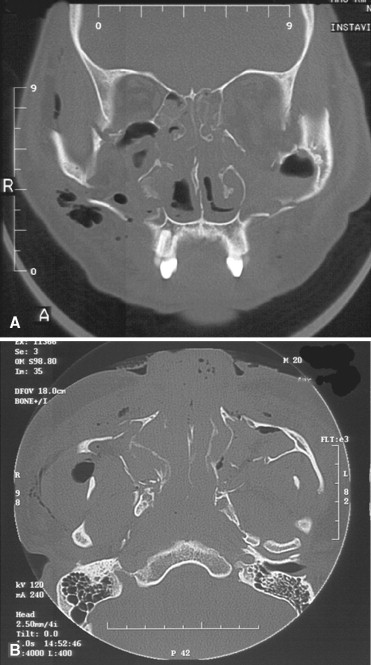
If available, using both types of imaging puts the surgeon at an advantage before entering the operating room. In using a single modality, two-dimensional multiplanar imaging (axial, sagittal, and coronal) would be the method of choice.
MAGNETIC RESONANCE IMAGING
MRIs are typically not helpful in acute bony trauma to the face. If there is a question of soft tissue injury to nervous structures, MRI may be helpful. MRI is typically performed 48 hours after trauma. Blood has variable signal intensity on T1-weighted images, depending on its age and location. Generally, a radiologist has a low degree of confidence in assessing a facial fracture with an MRI. MRI is used as an adjunctive examination when intracranial injury or unusual soft tissue injury may be present. MRI is superior in the evaluation of brain and dural-space injury. MRI has a high incidence of false-negative results, as compared with CT, for imaging the midface.
ULTRASOUND
Ultrasound has an evolving role in the diagnosis of facial trauma. Benefits of ultrasound include the avoidance of radiation exposure for the patient as well as the advantages that this diagnostic method is inexpensive, portable, noninvasive, readily available, and fast. In certain situations, it could be considered a first-line alternative to plain film radiography. Limitations include inability to diagnose nondisplaced fractures and nondiagnostic images in cases of tissue emphysema.
Ultrasound may be used as a postreduction verification of zygomatic arch fractures as opposed to re-exposing a patient to radiation. Additionally, it has some utility in visualizing the anterior wall of the frontal sinus. Currently, the limitations of ultrasound outweigh its usefulness in most facial trauma situations.
MIDFACE FRACTURES AND NEUROLOGIC INJURY
There have been many attempts to assess the relationship between facial trauma, in particular midface trauma, and neurologic injury. The key issue that research has attempted to address is the role of facial bones in protection from neurologic injury. From an evolutionary and mechanical standpoint, a description of the facial bones as an impact- or stress-bearing region to absorb forces that would otherwise be transmitted to the brain seems logical. Data from Lee et al showed that the presence of facial fractures is associated with decreased traumatic brain injury. However, the majority of recent data suggests the opposite is true. Specifically, Davidoff reported a 55% incidence of concomitant facial fracture and brain injury, defined as a loss of consciousness or post-traumatic amnesia. Keenan and Martin have independently shown facial fractures to be a marker for severe head injury.
These studies do not suggest that facial fractures cause brain injury in any way. They support the notion that in order to sustain facial fractures, a high-velocity and typically blunt force is required. The most common mechanisms of injury for facial fractures have been motor vehicle accidents, motorcycle accidents, and interpersonal violence. These mechanisms typically share the features of being high-velocity, blunt trauma. It is plausible that in order for midface or upper face injuries to occur a sufficient magnitude of force must be generated, ensuring transmission of force to the brain in the majority of cases.
Haug has shown that when there is neurologic injury and facial fractures, the maxilla or zygoma is more likely to be involved. Additionally, when facial fractures and deaths related to neurologic injury were reviewed, as many as 84% of patients had a fracture pattern that included the maxilla, nose, zygoma, or orbits. This seems to suggest that neurologic risk severity could be formulated based on the fracture patterns of the face. This would coincide with the notion that a greater velocity injury would be required to cause a certain fracture or multiple fractures. It has been shown that LeFort II and III fractures are more likely to occur with a combination of cranial bone fractures whereas a LeFort I fracture is associated with frontal bone fracture only. In addition, LeFort type fractures have a higher probability of intensive care unit (ICU) admission, higher Index Severity Scores, and a greater need for immediate operative intervention and for creation of a surgical airway.
NASO-ORBITAL-ETHMOID FRACTURES
INTRODUCTION
Naso-orbital-ethmoid (NOE) fractures have been classically described as the most challenging facial fractures to treat. Before 1960 little information can be found in the literature regarding treatment approaches to this region. The anatomy of the region tends to be delicate. Fractures tend to be comminuted. Late or inadequate correction of deformities can result in midface retrusion, shortened palpebral fissures, telecanthus, enophthalmos, ocular dystopia, blindness, cerebrospinal fistula, anosmia, epiphora, and nasal deformities.
ANATOMY
The bony structure of this region is composed of the internal angular process of the frontal bone, nasal bones, frontal process of the maxilla, lacrimal bone, lamina papyracea, ethmoid bone, sphenoid bone, and nasal septum. The nasal bones, vomerine bone, perpendicular plate of the ethmoid, ethmoid labyrinths, lacrimal bone, and lamina papyracea are thin and predisposed to comminuted fractures ( Figure 14-7 ).
The concept of horizontal and vertical buttressing can also be applied to this region. The superior horizontal buttress is composed of the frontal bone and superior orbital rims. The inferior horizontal buttress is comprised of the inferior orbital rims and zygoma. The vertical buttresses are created by the internal angular process of the frontal bone, the frontal process of the maxilla, the cartilaginous septum, the vomerine bone, and the perpendicular plate of the ethmoids.
Medial Canthal Tendon
The medial canthal tendon deserves separate attention in the anatomy section because of its importance in both the classification and treatment of NOE fractures. Untreated canthal disruptions will lead to one of the more obvious cosmetic deformities in this region.
Generally, the medial canthal tendon surrounds the lacrimal sac medially and develops laterally to merge with the orbicularis oculi muscle, tarsal plate, and suspensory ligaments of the eyelids. In this manner, the medial canthal tendon aids eyelid and globe support and improves the aesthetics of the palpebral fissures. Detachment of medial eyelid support will result in a horizontal narrowing of the palpebral fissure known as traumatic telecanthus. This is thought to be caused by the unopposed muscle pull of the orbicularis oculi on the mobile tendon. Normal intercanthal distance is 28 to 35 mm and closely approximates half the interpupillary distance. Intercanthal distances greater than 35 mm suggest injury and those greater than 40 mm are diagnostic for injury to the canthal attachment ( Figure 14-8 ).

Specifically, the medial canthal tendon divides into three limbs: anterior, posterior, and superior. The anterior limb is fan shaped, inserts on the anterior lacrimal crest, and extends to the frontal process of the maxilla. This limb measures approximately 10 mm in length and 4 mm in width. It functions to pull the medial commissure of the eyelids forward and slightly downward. The posterior, or deep, limb is thinner and inserts on the posterior lacrimal crest of the lacrimal bone. It functions to maintain the eyelids in a position tangent to the globe. The superior limb encompasses the lacrimal sac and attaches to the junction of the frontal process of the maxilla and the internal angular process of the frontal bone. This superior limb adds a posterior and superior vector to the medial canthal tendon ( Figure 14-9 ). The re-creation of this superior and posterior vector for canthopexy has proven to provide the best cosmetic outcomes in cases of canthus disruption.
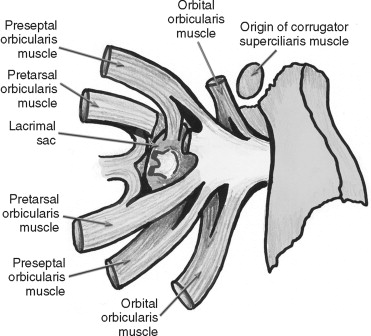
Lacrimal Drainage Apparatus
The lacrimal system consists of a gland, located in the superolateral aspect of the orbit, and a delicate drainage system that funnels from the upper and lower eyelids and exits into the nasal cavity below the inferior turbinate. The lacrimal drainage apparatus begins at the medial aspect of the upper and lower eyelids in the form of an upper punctum and a lower punctum. Each punctum has respective canaliculi that travel medially and join as the common canaliculus. The common canaliculus drains to the lacrimal sac, which joins the lacrimal duct. The lacrimal sac is situated in the medial aspect of the orbit in the lacrimal fossa. The duct is oriented vertically and runs inferolaterally from the lacrimal fossa to the inferior meatus of the nose through an opening known as the valve of Hasner. The duct is approximately 30 mm in length and is lined by columnar epithelium. The sac works in conjunction with the eyelid musculature to function as an excretory duct.
INJURY CLASSIFICATION
In other texts or journal articles, the names for fractures in the naso-orbital-ethmoid region range from “naso-orbital,” “naso-ethmoid,” “naso-ethmoid orbital,” “naso-orbital-ethmoid,” to “orbitoethmoid.” Classification of injury to the naso-orbital-ethmoid complex historically was described in terms of unilateral or bilateral and isolated or extended . Isolated referred to injuries of the central midface, while extended referred to injury to adjacent anatomic areas.
A recent classification scheme developed by Markowitz is more clinically useful to the surgeon. He refined the classic description by identifying the fracture pattern based on the “central” bone fragment. The borders of the central bone fragment are defined by the lateral nose, the inferior orbital rim, the medial orbital (ethmoidal) wall, the nasomaxillary buttress at the piriform aperture, and the frontal process of the maxilla. More succinctly, this can be seen as the lower two thirds of the medial orbital rim. The medial canthal tendon attaches to the superior aspect of the central fragment.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


