EPIDEMIOLOGY
Skin cancer is the most common malignant neoplastic entity affecting humans. These neoplasms can be divided into non-melanoma skin cancers (NMSCs) and malignant melanoma. NMSCs account for 95% of all skin neoplasms and melanomas for the remaining 5%. Melanomas are responsible for 75% of all skin cancer–related deaths. Malignant melanoma, a malignancy of melanocytes, was responsible for approximately 5020 deaths in 2006. It is estimated that 7910 deaths will result from melanoma in 2007. This accounts for approximately 4% of all cancer-related deaths in the United States ( Box 37-1 ).
-
4% of all cancer deaths
-
5% of all skin cancers
-
75% of all skin cancer–related deaths
-
20% occur in head and neck region
-
1 : 75 incidence rate in 2004
Approximately 62,190 cases of malignant melanoma were diagnosed in 2006. In 2004, approximately 55,000 cases were diagnosed. The mortality rate has risen by 2% each year since 1960 as a result of this rapidly increasing incidence. However, with this increasing incidence the 5-year survival rate has also increased. Since the primary mode of therapy (i.e., surgery) has not changed appreciably over time, one can attribute this to an increased public awareness and early detection of these lesions. This chapter discusses the etiology, risk factors, clinical and histological characteristics, diagnosis, staging, and management of this potentially fatal skin neoplasm.
INCIDENCE AND ETIOLOGY
Melanoma is one of a few malignancies in the United States with an increasing incidence. In 1935, the incidence of melanoma was 1 : 1500 and is estimated to reach 1 : 50 people by 2010. At the present time, 25% of individuals affected by this disease are under the age of 40. It is the most common malignancy in women ages 25-29 and is second only to breast cancer in women ages 30-34.
Approximately 20% of all melanomas are found in the head and neck region. Less than 1% of lesions are found in the oral cavity. These oral lesions, although rare, are associated with a high mortality rate. In general, men have a predilection toward being affected with head, neck, and trunk melanomas more frequently than women, who favor extremity (especially lower) sites.
Excessive ultraviolet (UV) light exposure was thought to be the primary etiologic factor in the development of malignant melanomas. The link between Caucasian race and living nearer the equator, such as in Australia or the Southeastern United States, is undeniable. However, this link does not provide a biologic explanation for many cases, such as subungual or mucosal melanomas. There is now compelling evidence that genetic aberrations, as in all malignant neoplasms, play a crucial role in the development. There is also evidence that links periods of high-intensity UV light exposure, rather than chronic exposure, with the development of melanomas. An exception is the lentigo maligna melanoma. This form of melanoma, as with the NMSCs (i.e., basal cell and squamous cell carcinomas) tend to be associated with more prolonged UV light exposures.
Caucasians are the typical patients who develop malignant melanomas. African-American, Hispanics, and Asians rarely develop the disease. Darker-skinned races tend to have higher mortality rates with melanoma because of the predilection toward developing the acral lentiginous subtype and typically presenting with advanced stage disease at diagnosis. Women tend to be slightly more affected than men worldwide and have slightly better overall survival than males. The countries with the highest rates of melanoma are Australia and New Zealand, with 37.7 cases per 100,000 men and 29.4 cases per 100,000 women. In comparison, the United States has approximately 6.4 cases per 100,000 men and 11.7 cases per 100,000 women. California, Florida, Texas, New York, and Pennsylvania have the highest rates of estimated new melanoma cases.
Many risk factors for the development of melanoma have been identified ( Box 37-2 ). Generally accepted risk factors are: Fitzpatrick skin type 1 or 2 ( Table 37-1 ), red or blonde hair, family history, actinic keratosis, pronounced freckling of the upper back, three or more blistered sunburns before adulthood, and an outdoor job (e.g., lifeguard) for more than 3 years before the age of 20. Individuals with two of these risk factors have an estimated threefold to fourfold increase in incidence of developing a melanoma; those with three or more have an increase incidence of approximately 20-fold. These risk factors do not adequately address melanomas in nonUV-light–exposed areas. These lesions are thought to arise de novo and not as a result of environmental exposure. A family history of melanoma increases the risk by two to eight times. Immunosuppression has also been associated with an increased risk of melanoma development.
-
Family history
-
Fitzpatrick skin type 1 or 2
-
Three or more blistering sunburns before age 20
-
Three or more years before age 20 with an outdoor job (e.g., lifeguard)
-
Actinic keratosis lesions
-
Pronounced freckling of upper back
-
Red or blonde hair
-
Immunosuppression
-
Dysplastic nevus syndrome
-
Congenital nevi >20 mm
| Type | Characteristics |
|---|---|
| 1 | Always burns easily, no immediate pigment darkening, never tans |
| 2 | Always burns easily, trace immediate pigment darkening, tans with difficulty and minimally |
| 3 | Burns minimally, immediate pigment darkening, tans gradually and uniformly (light brown) |
| 4 | Burns minimally, immediate pigment darkening, tans well (moderate brown) |
| 5 | Rarely burns, immediate pigment darkening, tans very well (dark brown) |
An association between benign melanocytic proliferations (e.g., nevus) and malignant melanoma has clearly been established by Skender-Kalnenas and co-workers. They evaluated 289 cases of thin, malignant melanomas and the association with benign melanocytic proliferations. A nevus was found to be associated with over 50% of the lesions, and of these nevi, 56% were dysplastic nevi, 41% were common acquired nevi, and 3% were congenital nevi. The association with melanocytic proliferation was greater with advanced age of the patient.
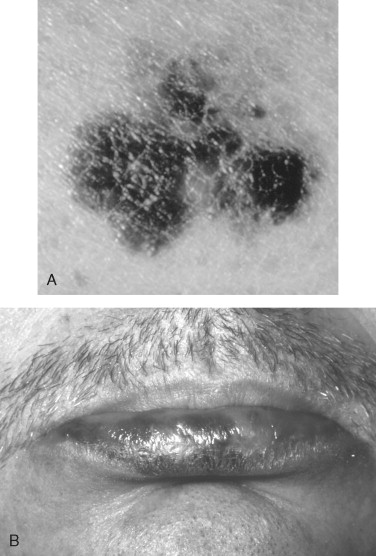
The majority of melanomas arising in the head and neck region, approximately 70%, have been found to arise in pigmented lesions. This includes pigmented lesions of the oral cavity ( Figures 37-1 and 37-2 ). A change in the character of pigmented lesions, particularly in patients with any other risk factors, should raise the level of suspicion for a malignant transformation. All pigmented lesions without an obvious etiology (e.g., amalgam tattoo) in the oral cavity should be biopsied and followed periodically since the mortality of intraoral melanomas approaches 100%. Congenital nevi greater than 20 mm have a malignant transformation rate of approximately 20%, and lesions associated with dysplastic nevus syndromes have a 100% rate of malignant transformation over an individual’s lifetime; removal of these lesions is recommended.


As a result of the high mortality associated with late melanomas, the index of suspicion with pigmented lesions of the head, neck, and oral cavity should be high. The authors recommend using, and instructing patients to use, the ABCDE and P method of evaluation:
-
A symmetry: Irregular “lopsided” lesions
-
B order: Notched, angled, nonlinear borders
-
C olor: Multiple colors within a lesion or loss of color (amelanotic)
-
D iameter: Greater than 6 mm lesion or changes in size of existing lesion
-
E levation: Changes in height or new onset nodularity to lesion
-
P ersistence: Lesion that demonstrates persistent erythema, scaling, itching, or ABCDE changes.
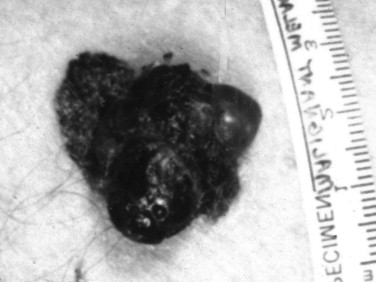
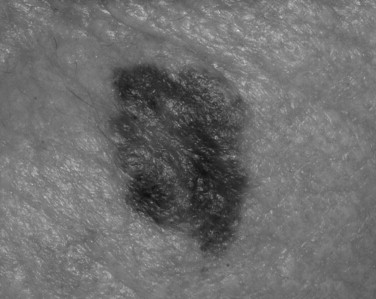
Melanomas have been clinically and histologically subdivided into five types ( Table 37-2 ): superficial spreading ( Figure 37-3 ), nodular ( Figure 37-4 ), lentigo maligna ( Figure 37-5 ), acral lentiginous ( Figure 37-6 ), and desmoplastic.
| Prevalence | Age | Clinical Features | Common Sites | |
|---|---|---|---|---|
| Superficial spreading | 70% of all; common in light skinned people | 4th-5th decade | Classic ABCDE features; pigmented macule | Head, neck, trunk, back, extremities |
| Nodular | 15% of all | 4th-5th decade | Rapid growth; usually from normal skin; poorer prognosis; 5% amelanotic | Head, neck, trunk |
| Acral lentiginous | 10% of all; most common in non-whites | 6th-7th decade | Tan, flat irregular macule; not associated with sun-exposed areas | Plantar, hands, subungual surfaces common |
| Desmoplastic | Rare; commonly associated with lentigo maligna lesions | 6th-7th decade | Sun-exposed areas; pigmented or flesh colored | Head and neck |
| Lentigo maligna | 5-10% of all; associated with chronic sun exposure | 7th-8th decade | Irregular, tan-brown macule | Head and neck; neck and cheeks commonly |

INCIDENCE AND ETIOLOGY
Melanoma is one of a few malignancies in the United States with an increasing incidence. In 1935, the incidence of melanoma was 1 : 1500 and is estimated to reach 1 : 50 people by 2010. At the present time, 25% of individuals affected by this disease are under the age of 40. It is the most common malignancy in women ages 25-29 and is second only to breast cancer in women ages 30-34.
Approximately 20% of all melanomas are found in the head and neck region. Less than 1% of lesions are found in the oral cavity. These oral lesions, although rare, are associated with a high mortality rate. In general, men have a predilection toward being affected with head, neck, and trunk melanomas more frequently than women, who favor extremity (especially lower) sites.
Excessive ultraviolet (UV) light exposure was thought to be the primary etiologic factor in the development of malignant melanomas. The link between Caucasian race and living nearer the equator, such as in Australia or the Southeastern United States, is undeniable. However, this link does not provide a biologic explanation for many cases, such as subungual or mucosal melanomas. There is now compelling evidence that genetic aberrations, as in all malignant neoplasms, play a crucial role in the development. There is also evidence that links periods of high-intensity UV light exposure, rather than chronic exposure, with the development of melanomas. An exception is the lentigo maligna melanoma. This form of melanoma, as with the NMSCs (i.e., basal cell and squamous cell carcinomas) tend to be associated with more prolonged UV light exposures.
Caucasians are the typical patients who develop malignant melanomas. African-American, Hispanics, and Asians rarely develop the disease. Darker-skinned races tend to have higher mortality rates with melanoma because of the predilection toward developing the acral lentiginous subtype and typically presenting with advanced stage disease at diagnosis. Women tend to be slightly more affected than men worldwide and have slightly better overall survival than males. The countries with the highest rates of melanoma are Australia and New Zealand, with 37.7 cases per 100,000 men and 29.4 cases per 100,000 women. In comparison, the United States has approximately 6.4 cases per 100,000 men and 11.7 cases per 100,000 women. California, Florida, Texas, New York, and Pennsylvania have the highest rates of estimated new melanoma cases.
Many risk factors for the development of melanoma have been identified ( Box 37-2 ). Generally accepted risk factors are: Fitzpatrick skin type 1 or 2 ( Table 37-1 ), red or blonde hair, family history, actinic keratosis, pronounced freckling of the upper back, three or more blistered sunburns before adulthood, and an outdoor job (e.g., lifeguard) for more than 3 years before the age of 20. Individuals with two of these risk factors have an estimated threefold to fourfold increase in incidence of developing a melanoma; those with three or more have an increase incidence of approximately 20-fold. These risk factors do not adequately address melanomas in nonUV-light–exposed areas. These lesions are thought to arise de novo and not as a result of environmental exposure. A family history of melanoma increases the risk by two to eight times. Immunosuppression has also been associated with an increased risk of melanoma development.
-
Family history
-
Fitzpatrick skin type 1 or 2
-
Three or more blistering sunburns before age 20
-
Three or more years before age 20 with an outdoor job (e.g., lifeguard)
-
Actinic keratosis lesions
-
Pronounced freckling of upper back
-
Red or blonde hair
-
Immunosuppression
-
Dysplastic nevus syndrome
-
Congenital nevi >20 mm
| Type | Characteristics |
|---|---|
| 1 | Always burns easily, no immediate pigment darkening, never tans |
| 2 | Always burns easily, trace immediate pigment darkening, tans with difficulty and minimally |
| 3 | Burns minimally, immediate pigment darkening, tans gradually and uniformly (light brown) |
| 4 | Burns minimally, immediate pigment darkening, tans well (moderate brown) |
| 5 | Rarely burns, immediate pigment darkening, tans very well (dark brown) |
An association between benign melanocytic proliferations (e.g., nevus) and malignant melanoma has clearly been established by Skender-Kalnenas and co-workers. They evaluated 289 cases of thin, malignant melanomas and the association with benign melanocytic proliferations. A nevus was found to be associated with over 50% of the lesions, and of these nevi, 56% were dysplastic nevi, 41% were common acquired nevi, and 3% were congenital nevi. The association with melanocytic proliferation was greater with advanced age of the patient.
The majority of melanomas arising in the head and neck region, approximately 70%, have been found to arise in pigmented lesions. This includes pigmented lesions of the oral cavity ( Figures 37-1 and 37-2 ). A change in the character of pigmented lesions, particularly in patients with any other risk factors, should raise the level of suspicion for a malignant transformation. All pigmented lesions without an obvious etiology (e.g., amalgam tattoo) in the oral cavity should be biopsied and followed periodically since the mortality of intraoral melanomas approaches 100%. Congenital nevi greater than 20 mm have a malignant transformation rate of approximately 20%, and lesions associated with dysplastic nevus syndromes have a 100% rate of malignant transformation over an individual’s lifetime; removal of these lesions is recommended.


As a result of the high mortality associated with late melanomas, the index of suspicion with pigmented lesions of the head, neck, and oral cavity should be high. The authors recommend using, and instructing patients to use, the ABCDE and P method of evaluation:
-
A symmetry: Irregular “lopsided” lesions
-
B order: Notched, angled, nonlinear borders
-
C olor: Multiple colors within a lesion or loss of color (amelanotic)
-
D iameter: Greater than 6 mm lesion or changes in size of existing lesion
-
E levation: Changes in height or new onset nodularity to lesion
-
P
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


