HISTORY
The history of Le Fort I osteotomy dates to Germany in 1859, when von Langenbeck performed the first maxillary osteotomy at the level of the fracture line described by Le Fort in 1901. The osteotomy was performed to access nasopharyngeal polyps. Mobilization of the maxilla with the use of bone chisels along the Le Fort I fracture line was described by Cheever in the United States in 1867, for the purpose of eradicating nasal obstruction caused by recurrent epistaxis. Le Fort I osteotomy was used for orthognathic surgical correction for the first time in 1927, when Wassmund corrected a post-traumatic malocclusion and midfacial deformities. Axhausen was the first surgeon to perform a total mobilization of the maxilla with repositioning, and later, Schuchardt performed a separation of the pterygomaxillary junction for mobilization of the maxilla. He noticed that incomplete osteotomy of the maxilla was insufficient for anterior repositioning of the maxilla and thus recommended a fracture at the pterygomaxillary junction.
In the 1960s, the precision of the operative technique was brought to light by Obwegeser. Two main technical issues that he addressed were the complete mobilization of segments to reposition the maxilla without tissue resistance, and the use of bone graft between the pterygoid plate and the maxillary tuberosity. Subsequently, several surgeons followed suit and further developed and refined the techniques of Le Fort I osteotomy that the oral and maxillofacial surgeons of today know. This technique has become an essential part of the surgical armamentarium of oral and maxillofacial surgeons for correction of dentofacial deformities. Despite its versatility, Le Fort I osteotomy was not popularized until the advent of safe and improved anesthetic techniques and hypotensive anesthesia. The risk of bleeding and vascular implications with down-fracturing of the maxilla in an uncontrolled environment was too great.
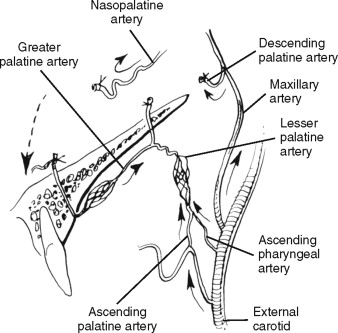
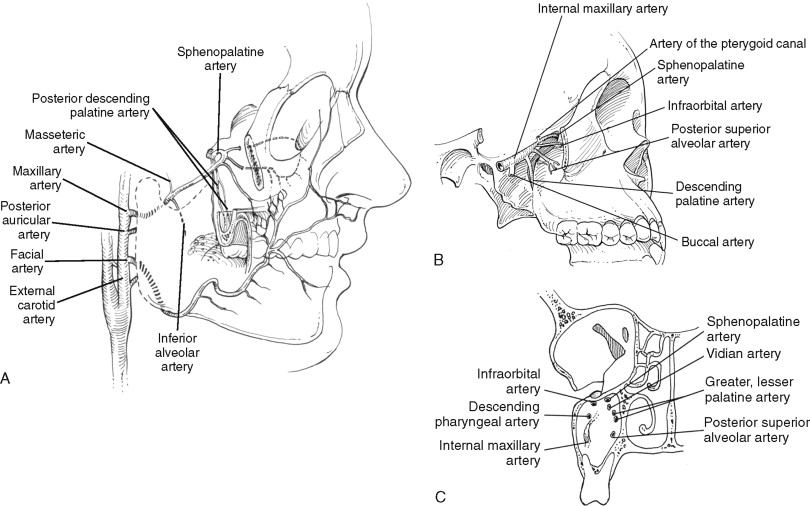
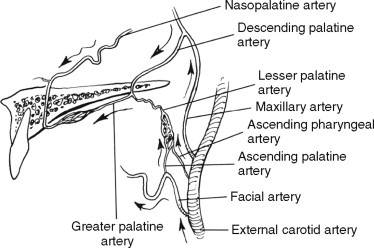
Another breakthrough was Bell’s landmark study, which provided the first scientific basis for the Le Fort I down-fracture. His study showed that adequate blood supply to the maxilla was maintained despite severance of the palatine artery ( Figure 7-1 ). Microangiographic evidence suggested that bilateral severance of the descending palatine vessels does not compromise the blood supply to the mobilized maxilla. Subsequently, Bell et al demonstrated the revascularization phenomenon and osseous healing following total maxillary osteotomy.
To this day, the techniques of Le Fort I osteotomy are under constant modification and revision and are tailored to different surgeons’ experiences and treatment objectives. The fundamental principles of maxillary osteotomy remain unchanged, with the focus on vascularity of the maxilla.
SURGICAL ANATOMY
BONES
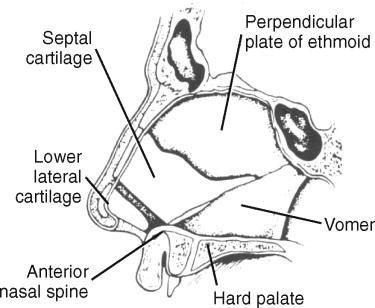
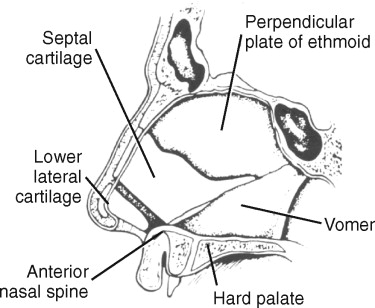
In the anterior view of the skull, the two maxillae form the border of the piriform aperture and the inferior and medial border of the orbit. The fused nasal crests extend upward from the palatine process to form the inferior portion of the nasal septum. The crests end anteriorly in the anterior nasal spine, and posteriorly, they articulate with the vomer. Nasal cartilage forms the anterior-inferior portion of the nasal septum, and the upper part of the bony septum is the perpendicular plate of the ethmoid bone ( Figure 7-2 ). The maxilla contains the maxillary sinus, which defines its anterior surface, and the canine fossa just above the alveolar process. Above the canine fossa and slightly below the infraorbital rim, the infraorbital foramen is located between 8 and 20 mm from the nasal floor ( Figure 7-3, A ). The vascular and neural contents of the infraorbital canal supply the blood flow and sensation to the skin of the cheek, the upper lip, and the lateral aspect of the nose. Superolaterally, the body of the maxilla articulates with the zygoma, and the roof of the maxillary sinus forms the predominant part of the floor of the orbit. Superomedially, the frontal process of the maxilla extends upward between the nose and the orbit, forming the lateral wall of the nasal cavity, and articulates with the frontal and nasal bones. Inferomedially, the perpendicular plate of the palatine bone runs upward as a posterior medial wall of the maxillary sinus, and it contains the descending palatine neurovascular bundle. During osteotomy of the lateral nasal wall, care is taken to extend the osteotomy no farther than 25 to 30 mm posteriorly from the piriform rim. The mean length of the medial sinus wall from the piriform rim to the descending palatine canal is approximately 34 mm.
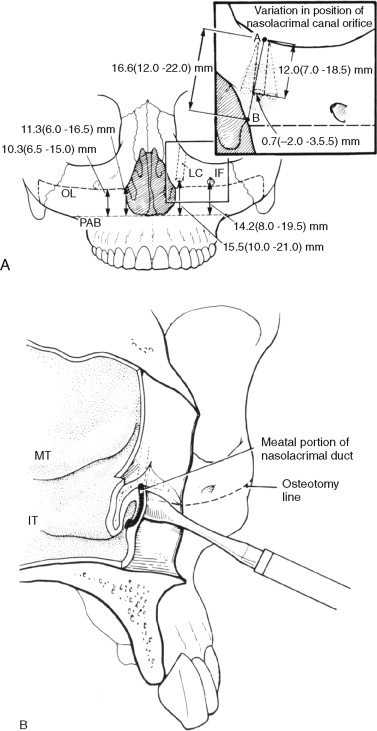
The nasolacrimal duct is located within the bony wall between the maxillary sinus and the nasal cavity. The duct terminates below the inferior turbinate in the inferior meatus. The location of the nasolacrimal duct underneath the inferior turbinate is 10 to 14 mm posterior from the piriform aperture and 10 to 21 mm from the nasal floor. The maxillary height is correlated with the height of the infraorbital foramen. Atrophic rhinitis is a potential complication of inferior turbinectomy performed during Le Fort I superior repositioning. When the osteotomy is made just beneath the infraorbital foramen and extends into the piriform rim at the level of the anterior attachment of the inferior turbinate, it is not very likely to cause injury to the nasolacrimal duct ( Figure 7-3, B ). Although it is an extremely rare event, injury to the lacrimal system can occur with Le Fort I superior repositioning.
Posteriorly, the maxillary tuberosity defines the posterior border of the maxilla, and the pterygomaxillary fissure lies between the maxillary tuberosity and the pterygoid plates of the sphenoid bone. This anatomic landmark is important in the pterygomaxillary disjunction during Le Fort I osteotomy because the descending palatine artery is located medially within 10 mm from the maxillary tuberosity as the osteotome is driven anteriorly and medially through the pterygomaxillary articulation.
MUSCLES
The orbicularis oris muscle, the main functional unit of the nasolabial region, serves as the attachment for several other lip and cheek muscles. The orbicularis oris surrounds the stomion, and its fibers arise from the buccinator, the depressor, and the levator anguli oris. Risorius, the smiling muscle, arises from the fascia over the parotid gland and blends into the angle of the mouth. Superolaterally, the zygomaticus major inserts into skin at the angle of the mouth and is continuous with the orbicularis oris. The four muscles that run downward into the upper lip include the zygomaticus minor (origin: zygomatic bone), the levator labii superioris (origin: maxilla), the levator labii superioris alaeque nasi (origin: frontal process of the maxilla), and the levator anguli oris (origin: maxilla). The levator labii superioris alaeque nasi inserts into the upper lip and into the ala of the nose ( Figure 7-4 ).
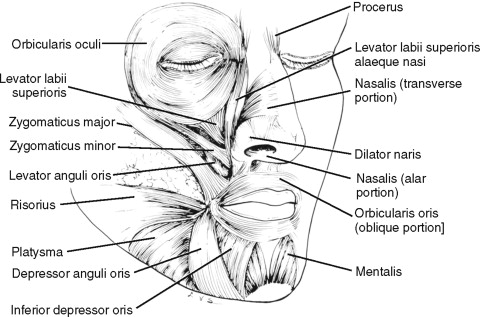
The muscles connected with the nose typically are not well developed. The depressor septi inserts into the base of the columella and the lowest part of the nasal septum. As the name implies, it pulls the septum downward. Lateral to it, the nasalis muscle arises from the maxilla and inserts into the lower edge of the alar cartilage. Alar base cinch involves primarily the nasalis muscles, which are compressors and dilators of the nares.
SURGICAL ANATOMY
BONES
In the anterior view of the skull, the two maxillae form the border of the piriform aperture and the inferior and medial border of the orbit. The fused nasal crests extend upward from the palatine process to form the inferior portion of the nasal septum. The crests end anteriorly in the anterior nasal spine, and posteriorly, they articulate with the vomer. Nasal cartilage forms the anterior-inferior portion of the nasal septum, and the upper part of the bony septum is the perpendicular plate of the ethmoid bone ( Figure 7-2 ). The maxilla contains the maxillary sinus, which defines its anterior surface, and the canine fossa just above the alveolar process. Above the canine fossa and slightly below the infraorbital rim, the infraorbital foramen is located between 8 and 20 mm from the nasal floor ( Figure 7-3, A ). The vascular and neural contents of the infraorbital canal supply the blood flow and sensation to the skin of the cheek, the upper lip, and the lateral aspect of the nose. Superolaterally, the body of the maxilla articulates with the zygoma, and the roof of the maxillary sinus forms the predominant part of the floor of the orbit. Superomedially, the frontal process of the maxilla extends upward between the nose and the orbit, forming the lateral wall of the nasal cavity, and articulates with the frontal and nasal bones. Inferomedially, the perpendicular plate of the palatine bone runs upward as a posterior medial wall of the maxillary sinus, and it contains the descending palatine neurovascular bundle. During osteotomy of the lateral nasal wall, care is taken to extend the osteotomy no farther than 25 to 30 mm posteriorly from the piriform rim. The mean length of the medial sinus wall from the piriform rim to the descending palatine canal is approximately 34 mm.
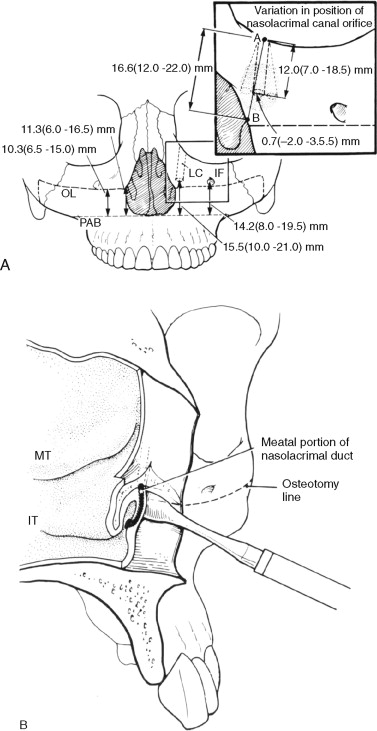
The nasolacrimal duct is located within the bony wall between the maxillary sinus and the nasal cavity. The duct terminates below the inferior turbinate in the inferior meatus. The location of the nasolacrimal duct underneath the inferior turbinate is 10 to 14 mm posterior from the piriform aperture and 10 to 21 mm from the nasal floor. The maxillary height is correlated with the height of the infraorbital foramen. Atrophic rhinitis is a potential complication of inferior turbinectomy performed during Le Fort I superior repositioning. When the osteotomy is made just beneath the infraorbital foramen and extends into the piriform rim at the level of the anterior attachment of the inferior turbinate, it is not very likely to cause injury to the nasolacrimal duct ( Figure 7-3, B ). Although it is an extremely rare event, injury to the lacrimal system can occur with Le Fort I superior repositioning.
Posteriorly, the maxillary tuberosity defines the posterior border of the maxilla, and the pterygomaxillary fissure lies between the maxillary tuberosity and the pterygoid plates of the sphenoid bone. This anatomic landmark is important in the pterygomaxillary disjunction during Le Fort I osteotomy because the descending palatine artery is located medially within 10 mm from the maxillary tuberosity as the osteotome is driven anteriorly and medially through the pterygomaxillary articulation.
MUSCLES
The orbicularis oris muscle, the main functional unit of the nasolabial region, serves as the attachment for several other lip and cheek muscles. The orbicularis oris surrounds the stomion, and its fibers arise from the buccinator, the depressor, and the levator anguli oris. Risorius, the smiling muscle, arises from the fascia over the parotid gland and blends into the angle of the mouth. Superolaterally, the zygomaticus major inserts into skin at the angle of the mouth and is continuous with the orbicularis oris. The four muscles that run downward into the upper lip include the zygomaticus minor (origin: zygomatic bone), the levator labii superioris (origin: maxilla), the levator labii superioris alaeque nasi (origin: frontal process of the maxilla), and the levator anguli oris (origin: maxilla). The levator labii superioris alaeque nasi inserts into the upper lip and into the ala of the nose ( Figure 7-4 ).
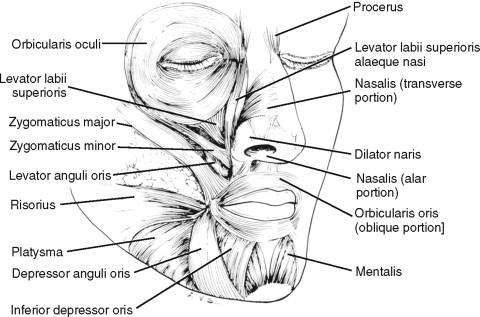
The muscles connected with the nose typically are not well developed. The depressor septi inserts into the base of the columella and the lowest part of the nasal septum. As the name implies, it pulls the septum downward. Lateral to it, the nasalis muscle arises from the maxilla and inserts into the lower edge of the alar cartilage. Alar base cinch involves primarily the nasalis muscles, which are compressors and dilators of the nares.
VASCULAR ANATOMY
The maxilla and its soft tissues are surrounded by a rich vascular network. The maxillary artery arises as one of the terminal branches of the external carotid artery at the posterior border of the ramus of the mandible, passing medial to the mandibular ramus. Here it gives rise to the middle meningeal artery and the inferior alveolar artery. The maxillary artery runs next to the lateral pterygoid muscle, where it gives off the masseteric artery. Its terminal branch passes deeply through the pterygomaxillary fissure into the pterygopalatine fossa ( Figure 7-5, A through C ). The internal maxillary artery enters the pterygopalatine fossa approximately 16 mm above the nasal floor. It gives off the posterior superior alveolar arteries (PSAs) that run downward onto the posterior surface of the maxilla. In the deeper dissection, the infraorbital artery can be identified as it emerges at the infraorbital foramen. A large descending palatine artery, which is the major vessel encountered most commonly during maxillary osteotomies, descends through the hard palate as greater and lesser palatine arteries ( Figure 7-6 ). The average distance from the most inferior point of the pterygomaxillary junction to the posterior superior alveolar artery is 15 mm, to the infraorbital artery is 32 mm, and to the descending palatine artery is 25 mm.
The pterygoid plexus is venous and surrounds the maxillary artery deep to the lateral pterygoid muscle. It drains into the maxillary vein and into the facial vein via the deep facial vein, accompanying the branch of the maxillary artery. It reaches the cavernous sinus with the V3 nerve through the foramen ovale to the middle meningeal veins through the foramen spinosum.
Bell highlighted the importance of collateral perfusion of the maxilla via the ascending pharyngeal, ascending palatal, and soft palate vessels. This is important when the descending palatine arteries are severed during maxillary osteotomy and preservation of the soft tissue pedicle has a profound effect on the maxillary blood supply. Anatomic dissections also show that with interruption of the descending palatine arteries, the blood supply to the maxilla is preserved via the ascending palatine branch and the anterior branch of the ascending pharyngeal artery within the posterior palatal tissue pedicle. These ascending arterial branches enter the soft palate at a position approximately 10 mm posterior to the pterygomaxillary junction. The fact that vascular perfusion of the ipsilateral hemimaxilla is maintained by the ascending arterial branches within the soft tissue pedicle underscores the importance of ensuring soft tissue integrity during the osteotomy procedures.
In addition to vascular perfusion, pulpal blood flow to the dentition and the gingival tissue must be considered ( Figure 7-7 ). Human research has shown that ischemic episodes in mobilized maxillary segments occur for a brief time after Le Fort I osteotomy. Laser Doppler flowmetry has shown a significant increase in pulpal blood flow between the first and third weeks after Le Fort I osteotomy, although gingival blood flow is not altered significantly.

SURGICAL TECHNIQUE
The patient should be positioned with the head elevated 10 to 15 degrees in reverse Trendelenburg position. This prevents pooling of the blood in the cephalad direction. The head position must be as neutral as possible, and the head is not hyperextended; this relaxes the soft tissues of the face and best simulates the upper lip drape over the incisors in repose. When the surgeon is planning to use an external reference point, the medial palpebral fissure or nasion is included in the surgical field. Local anesthesia is injected into the labial sulcus with the use of 1% lidocaine with 1 : 100,000 epinephrine. Palatal injection is unnecessary because this may elicit vasoconstriction in the palatal mucosa. Mean maxillary gingival blood flow decreases significantly during the intraoperative course of Le Fort I osteotomy; the addition of a vasoconstrictor to the local anesthetic may affect gingival blood flow even farther. However, the benefits of using a vasoconstrictor in reducing blood loss outweigh the risks of transient ischemia.
Initially, a horizontal circumvestibular incision is made in the buccal vestibule 2 to 3 mm apical to the mucogingival junction, extending between the first molars ( Figure 7-8, A ). The surgeon must be cognizant of the patient’s smile line, and the incision must be made more superiorly if the patient has a particularly animated smile and heightened gingival display, because the scar line may be visible in a full smile ( Figure 7-8, B ). If significant bleeding is encountered when the incision is made, the most likely source of bleeding is the posterior superior alveolar artery, which should be dissected and cauterized judiciously.
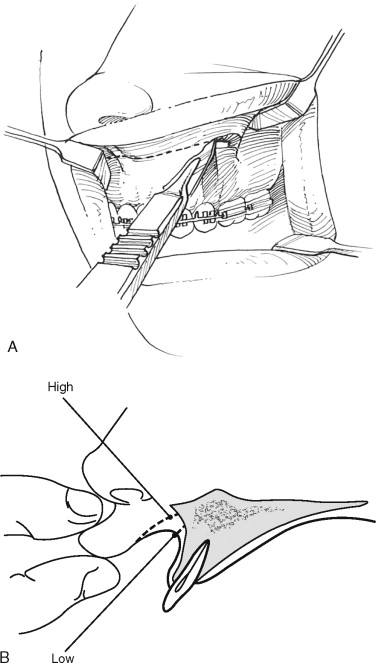
Surgical exposure of the maxilla can be divided into anterior, superior-lateral, and posterior dissections. The anterior dissection is directed toward the piriform aperture to expose the piriform rim. A periosteal or Cottle elevator is used in a superior-inferior swipe to create a pocket, and the nasal floor mucosa is elevated posteriorly approximately 10 to 15 mm from the nasal aperture. The periosteal elevator is left in place to protect the nasal mucosa ( Figure 7-9 ). The superior-lateral dissection starts with the reflection of the mucoperiosteum to expose the infraorbital neurovascular bundle as it exits from the infraorbital foramen. The posterior dissection is carried to the zygomaticomaxillary suture, the zygomatic buttress, and the pterygomaxillary fissure. A reverse curved retractor is placed in the pterygomaxillary fissure, and care is taken to maintain the integrity of the periosteum to prevent herniation of the buccal fat pad into the surgical field.
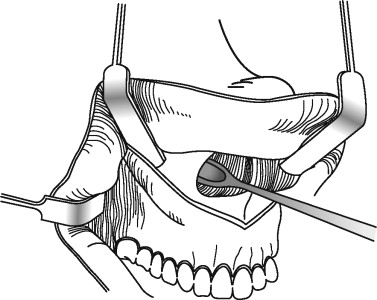
At this point, internal reference marks can be placed on the lateral maxillary walls. First, the projected osteotomy line is demarcated by making drill holes 4 to 5 mm above the apices of the maxillary canine and the first molar. The location of the root apices can be identified by noting the bony eminence for the canine and by performing radiographic measurements of the first molar root. Next, internal reference markings are made above and below the projected osteotomy line, and the distance is measured with a caliper ( Figure 7-10 ). Alternatively, an external reference can be established by placement of a Kirschner wire in the nasal bridge or a screw in the nasion, and the distance between the external reference point and the orthodontic bracket can be measured with a caliper ( Figure 7-11 ).
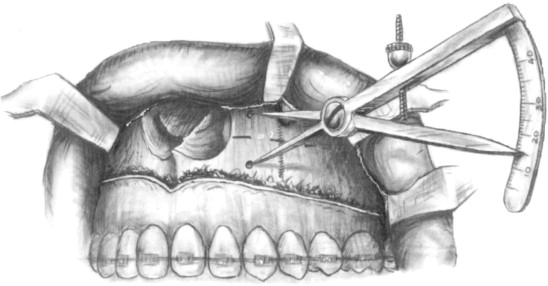
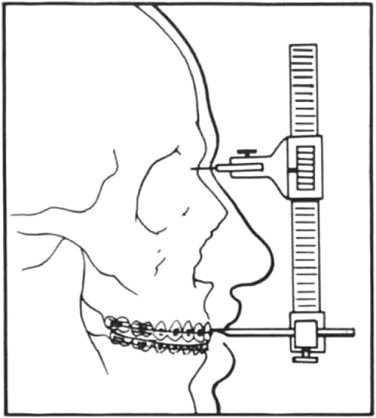
The medial palpebral fissure also can be used as a reference point instead of a metallic marker. By comparing two different methods of measuring distance with the use of a stable bony landmark (nasion) and what appears to be a less stable soft tissue landmark (medial palpebral fissure), Kahnberg et al found no statistically significant difference between the two methods. Nevertheless, with both external and internal reference points providing reasonable accuracy in repositioning the maxilla, the final decision on which technique to use is left to the individual surgeon’s preference and familiarity with the technique. Experienced surgeons are aware of the discrepancies between predicted and actual change in the surgically repositioned maxilla. In general, the use of an external reference is considered more accurate and reproducible for vertical maxillary repositioning, especially when the maxilla is moved in both horizontal and vertical vectors. Ultimately, orthognathic surgery planning is based on the accuracy of records, model surgery, and the use of the mandible as a guide to maxillary repositioning. The final anterior-posterior and transverse positions of the maxilla are determined with the intact mandible as the reference guide, assuming that the condyles are properly seated in the fossa. Therefore, it is prudent to capture the accurate position of the maxilla during the facebow transfer. This also requires close clinical attention to the three-dimensional maxillomandibular relationship, ensuring that the condyles are seated in the fossa intraoperatively as the maxilla is repositioned and fixed in the new position. The technique will be described later.
After the reference points are recorded, a reciprocating saw is used to section the lateral wall of the maxilla from posterior to anterior while the assistant retracts the buccal soft tissue. The horizontal osteotomy line is made parallel to the occlusal plane. When the saw cut is made through the lateral nasal wall, injury to the descending palatine artery during Le Fort I osteotomy can be avoided by not extending the osteotomy more than 25 to 30 mm posterior from the piriform rim. If the maxilla must be intruded, drill holes are made superior to the first osteotomy line at the distance measured by a small caliper that reflects the amount of intrusion at the canines and the first molars; the second osteotomy line is made with the saw as it connects these two points. A strip of bone from the lateral maxillary wall can be removed at this time and saved in sterile saline to be used as a graft later on. A reverse cut is made with the saw from inside out through the posterior wall of the maxilla, completing the osteotomy ( Figure 7-12, A and B ). Alternatively, the osteotomy line can be modified for maxillary inferior repositioning. When posterior maxillary inferior repositioning of 3 mm or less is desirable, a curvilinear cut is made in the posterior maxilla; this allows the maxilla to rotate clockwise as the maxilla is advanced, obviating the need for bone graft ( Figure 7-13 ). Inferior repositioning of the maxilla farther than 3 mm requires a bone graft for added stability.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


