Osteosarcoma is a common primary malignant tumor in long bones; it generally occurs in young adults. It is considered infrequent in the head and neck regions, where it is usually associated with poor outcomes and rates of survival. From a histopathologic point of view, osteosarcomas are commonly classified as osteoblastic, chondroblastic, or fibroblastic, although several unusual microscopic subtypes have also been reported. The purpose of this article was to present a case report of a maxillary chondroblastic osteosarcoma involving the maxillary sinus and the maxilla of a young woman who was diagnosed during early postorthodontic treatment follow-up. Treatment, prosthetic rehabilitation, and follow-up details are provided. Most importantly, this patient shows the importance of complete and systematic oral examinations during any routine dental treatment.
More than 90% of all oral cancers are squamous cell carcinomas, which are epithelial malignant tumors. However, several categories of primary malignant lesions can be seen in the orofacial region, and they can be either epithelial, mesenchymal, or hematolymphoid. The general incidence of oral malignant tumors is higher in elderly patients, but the male-to-female ratio seems to be decreasing, whereas its incidence appears to be increasing in younger adults. Although rare, head and neck malignant mesenchymal tumors (sarcomas) are a heterogeneous group of tumors with variable clinical presentations, pathologic classifications, and biologic behaviors. Osteosarcoma and rhabdomyosarcoma are the most common types of sarcomas in the craniofacial region. Osteosarcomas primarily affect the mandible and less frequently the maxilla, and the mean age for diagnosis is 30 years with heterogeneous sex distribution.
Generally, the signs and symptoms of osteosarcomas in the oral region are discreet and include regional swelling, low-intensity pain, paresthesia, changes in tooth position, loose teeth, and changes in the fit of prosthesis. They are often nonspecific and account for the considerable delay before the correct diagnosis is made. Thus, the treatment must be more aggressive, resulting in serious secondary effects that can impair the patient’s quality of life and also reduce the overall rate of survival. Currently, the etiology remains to be elucidated, but some risk factors such as a previous history of ionizing radiation therapy, retinoblastoma, and benign bone lesions such as Paget’s disease and fibrous osseous dysplasia have been associated with the development of head and neck osteosarcomas.
The radiographic features of jaw-bone osteosarcoma can be variable and usually show osteolytic, osteogenic, or mixed images. Additionally, there is an association between oral osteosarcomas and some radiographic images with a “sun-ray pattern.” This is the result of a periosteum reaction that deposits bone spicules on the surface of the lesion. Widening of the periodontal-ligament space and enlargement of the mandibular canal are also widely described as important radiographic features of osteosarcoma. All of these characteristics can be observed in periapical, occlusal, and panoramic radiography. On the other hand, the radiographic aspects of jaw-bone osteosarcomas are not pathognomonic and, as such, can be difficult to interpret or distinguish from the images of fibrous dysplasia or osteomyelitis. Thus, incisional biopsy and histopathologic analysis are essential for the final diagnosis and further treatment.
Worldwide, a rise in the incidence of oral cancers in young patients has been reported; this emphasizes the importance of early detection of malignant oral lesions. Dentists must therefore be educated on the need for comprehensive and systematic examinations of the oral cavity because of their essential role in early detection of premalignant and malignant orofacial disorders. The purpose of this article was to describe a case of maxillary osteosarcoma that was not identified by the patient’s orthodontists during early postorthodontic treatment follow-up.
Case report
A 28-year-old woman attended the Oral Medicine Clinic of the School of Dentistry of Araçatuba (State University of São Paulo) in Brazil with a chief complaint of a lump in the upper left maxilla. She had noticed the lesion during oral hygiene procedures 7 months before attending our clinic and had no previous radiotherapy or systemic relevant disease. She recently finished a 2-year orthodontic treatment and was being followed up ( Fig 1 , A ). According to her, the lesion was never examined by her orthodontists during the treatment or the follow-up. After the patient consulted her orthodontic team regarding the origin of the oral lesion, they suggested that it was a “normal osseous exostoses” and did not refer her for further examination by a specialist.
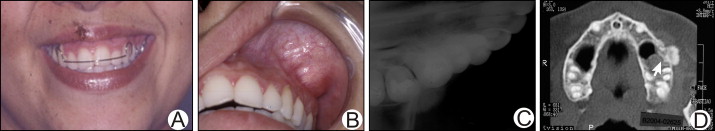
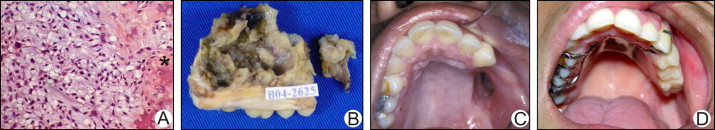
When we examined the patient, a nodule, 4 cm in diameter, was noticed in the upper left buccal vestibule close to the molar region; it was hard and painless on palpation, and had normal overlying mucosa ( Fig 1 , B ). Periapical, occlusal, and panoramic radiography scans and a computed tomography scan were taken. The panoramic and periapical radiographic examinations showed no signs of bone destruction, root resorption, or widening of periodontal-ligament space. The occlusal x-ray suggested an osteogenic image in the buccal surface of the left maxillary molar region, with a discreet “sun-ray pattern” ( Fig 1 , C ). The computed tomography (axial slice) showed exophytic osseous formation in the lateral wall of the left maxillary sinus with soft-tissue extension and partial involvement of the left maxillary sinus ( Fig 1 , D ).
An incisional biopsy was performed, and the histopathologic assessment showed a sarcomatous tissue composed of variable shaped cells (spindle and oval), mild cellular pleomorphism, osteoid areas, and deposition of an osseous matrix within the atypical cells, providing the microscopic diagnosis of osteosarcoma ( Fig 2 , A ).