16
Mandibular Anesthesia I: Pulpal Anesthesia
Mandibular block is the technique of choice for pulpal anesthesia of the mandibular molars and premolars. Infiltration is much less effective when applied to the mandible, owing to the higher density of the cortical bone in the mandible as compared to the maxilla (Table 3.2, Chapter 3), especially along the external oblique ridge. Mandibular block accounts for nearly 30% of all anesthetic injections performed in dentistry (Annex 1). Although it also known as inferior alveolar nerve block, the term mandibular block is more semantically precise because the block often involves not only the inferior alveolar but also the lingual and buccal nerves, and the nerve to the mylohyoid muscle.
Mental nerve block has been excluded from this chapter because of its two disadvantages:
- The mental foramen is difficult to locate. In clinical practice, it takes a full minute or longer to find when sought with a needle between the apexes of the two premolars in over 40% of cases (Joyce and Donnelly 1993).
- The risk of introducing the needle to the mental foramen and injuring the vascular nervous package is high. Clinical studies have shown that there is a 23% risk of hitting (Lustig and Zusman 1999) and a 12% risk of damaging the mental nerve (Joyce and Donnelly 1993). Buccal infiltration with potent a local anesthetic such as 4% articaine with 1:100 000 epinephrine (A‐100) is a technique more readily mastered that yields good results and entails lower risk.
Indirect mandibular block or the 1‐2‐3 technique, developed by Heinrich Braun (Lindsay 1929a) and furthered by Guido Fischer since 1910 (Fischer 1910), has likewise been excluded. Known by that name because it consists of a three‐phase attempt to reach the groove of the mandibular neck (sulcus colli) indirectly by varying the direction of the needle in the soft tissue (Figure 16.1), the technique calls for very thick, stiff caliber 20G needles (no longer in use) that neither break nor bend. It is characterized by major disadvantages, including needle breakage, increased technique sensitivity, and higher probability of injuring the periosteum or the medial (internal) pterygoid muscle (Lindsay 1929b). Although there are more modern variations (Clarke and Holmes 1959; Sittitavornwong et al. 2017), the 1‐2‐3 technique is of primarily historic interest and is seldom used today.
All the techniques listed below and described in this chapter are intraoral because extraoral approaches are mostly confined to hospital scenarios.
- Mandibular block for pulpal anesthesia of molars and premolars via the:
- conventional or direct approach
- Gow‐Gates approach
- Laguardia–Akinosi approach
- Double infiltration for pulpal anesthesia of the anterior mandibular teeth.
Mandibular Block: General Remarks
The first known mandibular block was performed by William Stewart Halsted on a medical student in 1884, who was administered 0.4 ml of a 4% solution of cocaine (Hall 1884). There is no record of whether the technique was intra‐ or extraoral, although the three techniques most commonly used today are intraoral.
The primary but not the sole aim of all these techniques is to introduce enough solution to anesthetize the inferior alveolar nerve before it enters the mandibular foramen (Berns and Sadove 1962; Galbreath and Eklund 1970). Given that the inferior alveolar nerve fibers are myelinated, at least three nodes of Ranvier (Blair and Erlanger 1939) or a total of 6 mm must be anesthetized since the nodes in this nerve are spaced at 0.5–1.8 mm (Rood 1978a,b).

Figure 16.1 Mandibular block, 1‐2‐3 technique.
Source: Redrawn from Andlaw and Rock (1994).
Zone Anesthetized
The various mandibular block techniques anesthetize the following nerve trunks, although to varying degrees.
- The following areas are anesthetized by the inferior alveolar nerve (all in same side, ipsilateral):
- Teeth, pulp, and periodontal ligament in the entire hemiarch on the respective side; molars and second premolar (via the inferior alveolar nerve itself) and first premolar, canine, and incisors via the incisive nerve, a branch of the inferior alveolar nerve.
- Interdental papillae, including fibromucosa, bone, and periosteum to the midline.
- Vestibule, via the mental nerve; fibromucosa (alveolar mucosa and attached gingiva), bone, and periosteum in the area between the premolars and the central incisor, including the molar zone in the 10% of cases where the buccal nerve is scantly developed (Hendy and Robinson 1994); the skin over the ipsilateral half of the chin and in particular half of the lower lip, from the corner of the mouth to the midline, denoting successful anesthetization of the alveolar nerve.
- The lingual nerve affects the lingual side fibromucosa (alveolar mucosa and gum), bone, and periosteum of the teeth, along with half of the floor of the mouth and the front two‐thirds of the tongue on the side involved.
- The buccal nerve inneravates the following structures (all ipsilaterally): the buccal fibromucosa (alveolar mucosa and attached gingiva), bone, and periosteum of the retromolar triangle; side of the lower molars (reaching the second premolar in 5%) (Hendy and Robinson 1994).
- Other nerves proximal to the inferior alveolar nerve may also be anesthetized:
- The auriculotemporal nerve, innervating the skin in the temporal region, in some cases as far as the border of the parietal, masseteric, frontal, and supraorbital regions. This nerve is only anesthetized in 20% of cases due to migration of the anesthetic, the odds of which are increased if the patient is in a reclined position (Kim et al. 2003).
- The mylohyoid nerve, primarily a motor nerve and branch of the mandibular division of the trigeminal nerve, is located on the floor of the mouth. It also innervates the anterior belly of the digastric muscle; when anesthetized, the patient may feel discomfort during swallowing. The nerve to mylohyoid may provide supplemental innervation to the pulp of the posterior and anterior teeth on the side in question and even the contralateral incisors (Chapter 3), as well as sensory innervation to the skin on the chin (Roberts and Harris 1973). This nerve trunk is frequently anesthetized in mandibular blocks.
Factors to Consider for the Mandibular Block
The factors that affect the scope and limitation of the mandibular block are discussed in this section.
Efficacy is Correlated to the Location of Tooth in the Mandible
Mandibular block delivers acceptable results in molars and premolars (Table 16.1). Pulpal anesthesia is successful in 60–70% of cases involving the posterior teeth within 10–15 minutes after injection of 1.8 or 3.6 ml of standard solution (2% lidocaine with 1:100 000 epinephrine, L‐100). In contrast, as the results are poor in the anterior teeth (Table 16.1), mandibular block can be said to be effective in posterior mandibular teeth only.
Table 16.1 Degree (%) of pulpal anesthesia in lower teeth 10 and 15 minutes after injecting one (1.8 ml) or two (3.6 ml) cartridges of a standard L‐100 solution for conventional mandibular block, as well as maximum success rate (%) and time of peak effect electric pulp tester data (see Annex 25).
| 1.8 ml | 3.6 ml | |||||
|---|---|---|---|---|---|---|
| Time after injection | Time after injection | |||||
| Tooth | 10 min | 15 min | Maximum success | 10 min | 15 min | Maximum success |
| Posterior (M and PM) | 60% | 65% | 80%/40 min | 65% | 70% | 80%/40 min |
| Lateral incisor | 30% | 35% | 55%/40 min | 30% | 40% | 55%/40 min |
| Central incisor | 10% | 15% | 25%/30 min | 15% | 25% | 35%/40 min |
M, molar; PM, premolar.
High Failure Rate
As mandibular block is characterized by a high failure rate even in posterior teeth, it must be reinforced, as discussed later.
Unreliability of Lower Lip Anesthesia
An anesthetized lower lip is indicative of anesthesia of the mental nerve which innervates it but not of mandibular dental pulp (Annex 25). A numb lower lip is specific but not sensitive: its absence definitely indicates that the pulps are not anesthetized, but its presence is not a reliable indicator that the pulps are anesthetized (Chavarria‐Bolaños et al. 2017). In other words, a numbed lower lip is a necessary but not a sufficient indication of pulpal anesthesia.
Sequential Nature
The lower lip and teeth are anesthetized sequentially. The lower lip is anesthetized first, followed by pulpal anesthesia of the molars, premolars, and anterior teeth in that order (Table 16.2). The conclusion is that anesthetic onset is longer than previously thought. Clinicians should wait at least 10–15 minutes after administering the anesthetic, which is when pulpal anesthetic onset is most rapid. After that time, anesthetic onset continues but much more slowly (Annex 25).
The Longer the Time, the More Intense the Anesthesia
In 80% of cases, maximum pulpal anesthesia in posterior teeth is attained after 40 minutes (Table 16.1), although waiting 40 minutes is not normally practical today. The same applies to the soft tissue anesthesia peaking in the lower lip after 40 minutes (Hersh et al. 1995).
Minor Effect of the Type of Anesthetic
In mandibular block, the different local anesthetics available have little impact on success and all are effective (Annex 24). A mandibular block is effective if the anesthetic is injected close to the inferior alveolar nerve, spanning the lingula and a few aponeurotic membranes, to position the solution in a place from which it can spread passively toward the nerve essentially unobstructed. That is not the case in buccal infiltrations, in which the potency of the anesthetic is instrumental to efficacy because the solution must cross barriers (periosteum, cortical, and spongy bone) to reach the dental apex and anesthetize the pulp. In mandibular blocks, other factors such as accessory pulpal innervation (mylohyoid nerve, buccal nerve), anatomical variations (high lingula, double alveolar ducts), and the greater complexity of the technique affect the outcome, inducing failed pulp anesthesia even when the inferior alveolar nerve is successfully blocked (deeply numbed lower lip).
The anesthetic of choice for mandibular blocks is 2% lidocaine solution with 1:100 000 or 1:80 000 (L‐100 or L‐80) for the following reasons:
- It is just as effective as even the most potent solutions (with high anesthetic or vasoconstrictor concentrations) such as 4% articaine with 1:100 000 epinephrine (A‐100) or 2% lidocaine with 1:50 000 epinephrine (L‐50) (Annex 24).
- Lidocaine is less concentrated, which means that more volume can be administered before reaching the maximum recommended dose (MRD). In more concentrated local anesthetics, such as 3% mepivacaine or 4% articaine, the MRD is achieved at a lower volume. For patients weighing at least 70 kg, up to 8.5 cartridges (1.8 ml) of 2% lidocaine can be administered as the maximum dose (Annex 10), whereas with other solutions only 5.5 to seven cartridges can be injected. This is especially important when treating small children, as local anesthetic overdose and toxicity is more of a concern.
Table 16.2 Reported and mean electric pulp tester‐measured times (minutes) of lower lip and pulpal anesthesia in first molar (first M), first premolar (first PM) and lateral incisor (LI).
Lower lip Reference Sample size Subjective Objective First M First PM LI Vreeland et al. (1989) 30 8.8 6.2 8.4 — 13.2 Chaney et al. (1991) 30 4.7 7.7 8.2 10.2 13.0 Hinkley et al. (1991) 30 6.1 10.6 8.8 10.6 12.3 McLean et al. (1993) 30 5.0 10.7 10.8 11.8 17.8 Kanaa et al. (2006) 38 — — 5.4 8.9 13.3 Steinkruger et al. (2006) 51 — — 8.8 10.8 13.0 Steinkruger et al. (2006) 51 — — 9.2 10.8 13.0 Goldberg et al. (2008) 40 — — 8.0 7.0 12.0 Kanaa et al. (2009) 36 — — 6.8 8.9 10.9 Mean 6.2 8.8 8.3 9.9 13.6 - It has been listed by the US FDA as pregnancy risk B (safe).
- There is less risk for neurotoxic injury to the inferior alveolar nerves when applied as a block. This is not a property that is inherent to lidocaine, but rather due to the lower lidocaine concentration (2%), as compared to 4% solutions of articaine and/or prilocaine, which has been implicated in such side effects (see Chapter 22).
Impact of the Volume Injected
As Table 16.1 shows, injecting two cartridges of the standard solution (3.6 ml of L‐100) improves pulpal anesthesia after 10–15 minutes in 5% of posterior teeth (Annex 25).
Minor Effect of the Specific Mandibular Block Technique
The Gow‐Gates technique was initially believed to deliver better results than the conventional or direct technique, but as discussed throughout this chapter that has not been proven. Overall, the conventional or direct technique affords the best clinical results of the three mandibular block approaches (Table 16.3) and is the easiest to master.
Bilateral Mandibular Blocks
Bilateral mandibular blocks (on the right and left sides simultaneously) can be utilized when bilateral mandibular anesthesia is necessary. This procedure was initially believed to entail the risk of serious consequences, such as soft tissue (tongue and lip) injury due to inadvertent biting or discomfort for patients (i.e. dysgeusia, dysphagia as the tongue is anesthetized.) Nonetheless, the only problem reported to date is minor discomfort when swallowing or drinking (Adatia and Gehring 1972). Even in children, bilateral mandibular block has been found (anti‐intuitively) to lead to less self‐injury than its unilateral counterpart for two reasons: (i) as bilateral blocks entail more extensive, lengthier treatment, the child’s soft tissues are anesthetized for less time after leaving the dentist’s office and (ii) as the soft tissue anesthesia is felt symmetrically, children are less inclined to explore and bite the tongue and cheeks, as they do not feel a contrast in sensation between the two sides (College et al. 2000).
Long, Caliber 25G Needles
Mandibular block should be performed using caliber 25G needles (a slightly less optimal alternative is caliber 27G, in as much as 25G needles are not readily available today) for the following reasons (see Chapter 11):
- They deviate less across the linear insertion.
- They ensure good aspiration.
- They do not cause more pain (pain myth, Chapters 11 and 13).
- They are less likely to break.
The 25G needle must be of sufficient length to traverse 20–30 mm of soft tissue before reaching the target and should never be inserted into the soft tissue up to the hub because they are more liable to break.
Table 16.3 Comparison of conventional, Gow‐Gates, and Laguardia–Akinosi mandibular block techniques: clinical variables.
| Mandibular block technique | ||||
|---|---|---|---|---|
| Variable | Reference | Conventional | Gow‐Gates | Laguardia–Akinosi |
| % Positive aspirations | 10% | 5–10% | 5% | Annex 22 |
| % Lower lip failure After 5 min After 10 min |
10% 5% |
30% 5% |
30% 20% |
Annex 28 |
| % Lingual nerve anesthesia | 95% | 80% | 85% | Annex 29 |
| % Buccal nerve anesthesia | 60% | 70% | 70% | Annex 29 |
| Grade A anesthetic efficacy | 85% | 80% | 80% | Annex 30 |
Slow Injection
As noted in Chapter 13, the injection speed presently recommended is 40–60 seconds for a 1.8‐ml cartridge to:
- Reduce pain because tissues are not distended abruptly.
- Reduce toxicity in the event of intravascular injection. For some authors this is the single most important measure for preventing adverse reactions, more even than aspiration (Malamed 2004).
- Enhance clinical efficacy. Higher pulpal anesthesia success rates according to clinical trials (Kanaa et al. 2006).
Mandibular Block: Conventional or Direct Technique
The conventional or direct technique, also denominated the classic or standard (or inferior alveolar nerve block), is much more commonly used than others worldwide because of its greater efficacy and relative simplicity. It consists of inserting the needle, directed from the lower premolars on the opposite side, into the pterygotemporal depression and subsequently into the pterygomandibular space (Figure 3.14, Chapter 3) and from there to the sulcus colli in the ramus of the mandible above the lingula (Figure 16.2), where the anesthetic solution is deposited and where the inferior alveolar nerve lies in a wide open mouth. It is called “direct” because the needle is inserted directly to the target, with no need for prior maneuvering.
This technique was initially introduced by Parisian clinician Pageix in 1906, although he directed the needle from a point on the midline too high (15–20 mm) over the occlusal plane (Lindsay 1929a). Boris Levitt (New York) developed the technique as it is known today (Levitt 1924), while Ashley Lindsay (Toronto) was instrumental in its popularization (Lindsay 1929a,b). Nonetheless, a host of minor variations on the technique are in place and each dentist could almost be said to have their own.
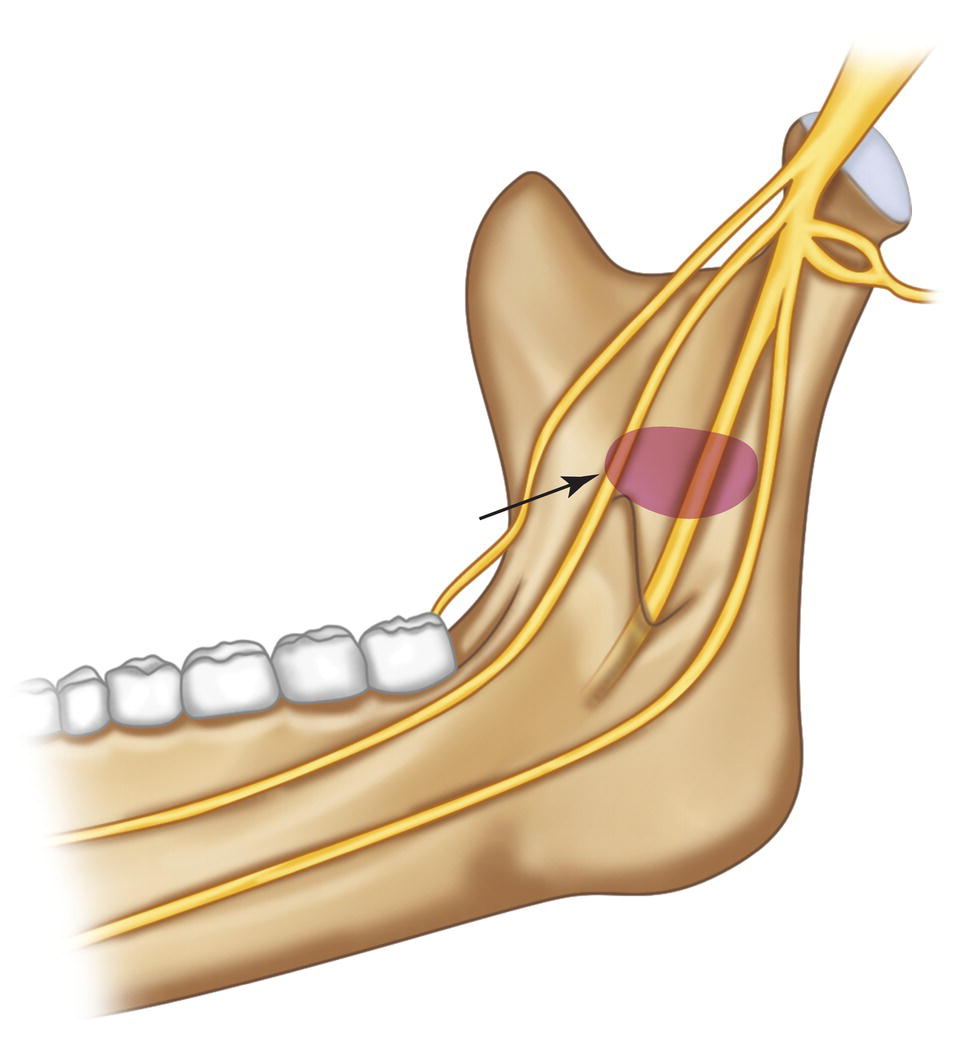
Figure 16.2 Sulcus colli above and behind the lingula, where the anesthetic solution is deposited in conventional mandibular block.
Distribution of the Anesthetic Solution
The anesthetic solution normally spreads rapidly across the pterygomandibular space and it remains there for several minutes (Petersen 1971). It is confined between the anterior and posterior edges of the ramus of the mandible, although the course taken cannot be predicted because the path of least resistance is determined by the fascial planes and the structures inside the pterygomandibular space (Berns and Sadove 1962; Galbreath and Eklund 1970). That said, it tends to travel upward and backward (sigmoid distribution) (Berns and Sadove 1962; Galbreath and Eklund 1970; Petersen 1971), therefore the success rate is lower if the anesthetic is positioned too high and too far back of the inferior alveolar nerve (Galbreath and Eklund 1970; Petersen 1971). In such situations, while the solution tends to spread to the parapharyngeal space, it does so more slowly (Petersen 1971).
The greatest factor in achieving a successful direct mandibular block is the position of the needle, which must be as close as possible to the beginning of the mandibular foramen and behind and close to the lingula (<5 mm), but this does not guarantee a perfect success rate (Berns and Sadove 1962; Galbreath and Eklund 1970). In contrast, placing the tip of the needle more than 5 mm away from and behind the mandibular foramen is associated with a large number of failures (Berns and Sadove 1962; Galbreath and Eklund 1970; Petersen 1971).
Zone Anesthetized
The zone anesthetized is as described in the general remarks, although the degree to which each element is numbed varies from one technique to another. All techniques must anesthetize the inferior alveolar nerve, often indicated by soft tissue (the lower lip ipsilateral to the injection site). In 95% of cases, the lingual nerve is also anesthetized with this technique and the buccal nerve in 60% (Table 16.3 and Annex 29).
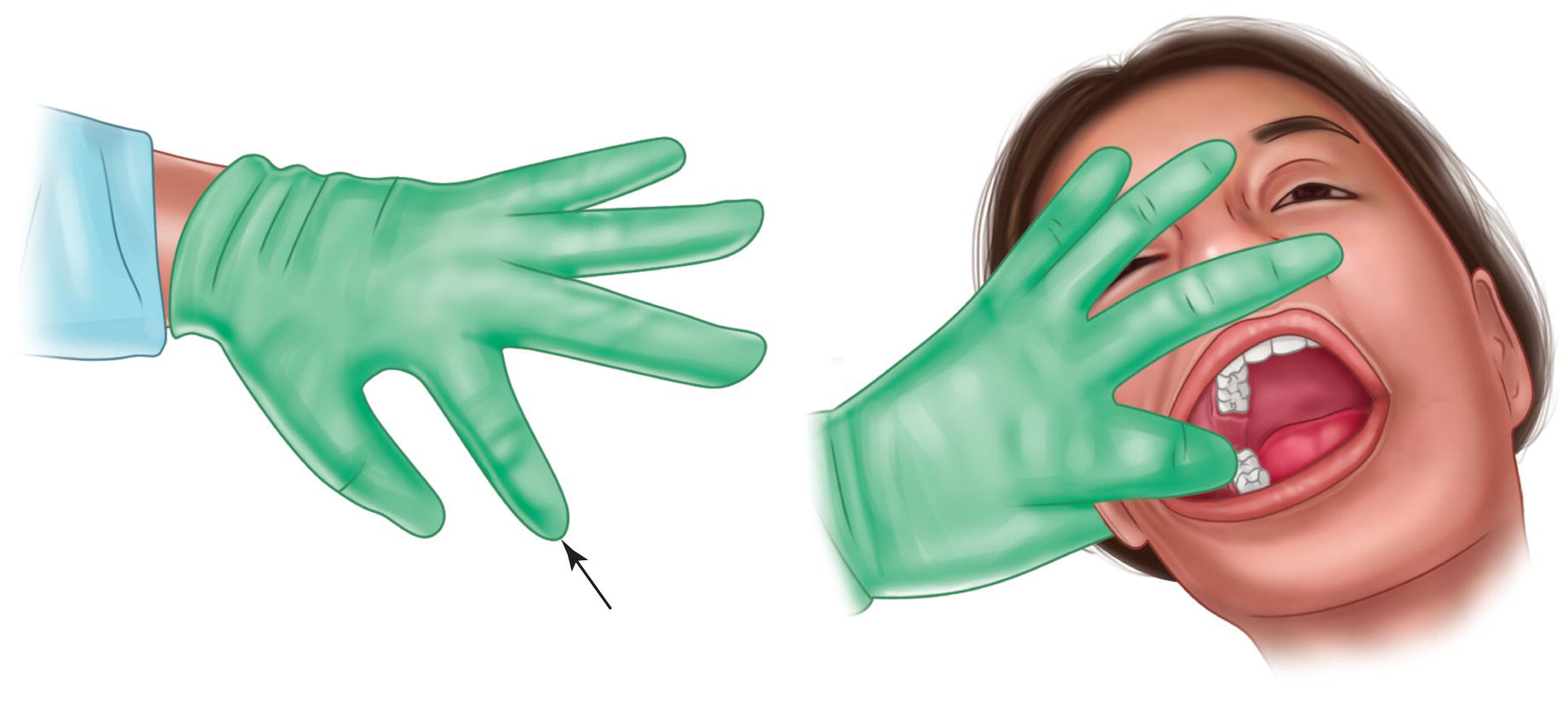
Figure 16.3 Index figure of non‐injection hand inside patient’s mouth for approach from right side, with other fingers stretched across patient’s face.
Technique
- Use a long (35–42 mm) needle, given the depth of the insertion. Caliber 25G is ideal because it affords good aspiration and as it is thick and stiff, it deviates very little. If caliber 25G is not available, 27G can be used, although this is less effective because deflection is somewhat greater.
- Solution. In most cases standard 2% lidocaine with 1:100 000 (L‐100) or 1:80 000 (L‐80) epinephrine is the option of choice (Annex 24).
- Patient positioning
- Supine or semisupine in dentist’s chair.
- Mouth opened maximally throughout the injection to facilitate direct visualization of intraoral landmarks and ensure that the inferior alveolar nerve lies against the sulcus colli on the inner side of the ramus of the mandible (target area).
- Head turned slightly to the same side as the side being injected (i.e. right in right‐side blocks and to the left in left‐side blocks).
- Tongue at rest and low in the posterior part of the mouth (Keetley and Moles 2001).
- Dentist’s position and position of the non‐dominant hand (i.e. left hand in right‐handed clinicians), depending on the side to be anesthetized
- Right side:
- Dentist at 8:00 o’clock.
- Index finger in the patient’s mouth (Figure 16.3).
- All other fingers stretching across the patient’s face to block their vision and control the position of the mouth.
- Left side:
- Dentist at 9:00–10:00 o’clock.
- Thumb of the non‐dominant hand in the patient’s mouth, requiring the right‐handed dentist to pass their left arm over the patient’s forehead (Figure 16.4).
- Dentist’s non‐injection palm and wrist blocking patient’s vision.
- Right side:
- Intraoral finger or thumb. The finger in the patient’s mouth should rest on the anterior edge of the ramus of the mandible, in the concavity known as the coronoid notch (Figure 16.5). It should also be parallel to the occlusal plane of the mandibular molars to:
- Bring the pterygotemporal depression into view.
- Help visualize the zone and locate the needle insertion site.
- Tighten and stretch the soft tissue to make needle insertion less traumatic.
In 10% of cases the coronoid notch cannot be readily reached because it is underdeveloped or the adjacent soft tissue is very thick (anterior edge of the temporal muscle or adipose tissue and mucosa) (Angelman 1945). In such cases, clinicians should gently exert greater pressure to palpate the area and identify the anatomic landmarks.
- Insertion zone. The insertion zone lies in the pterygotemporal depression, which consists of a fold or cleft in the oral mucosa that is elliptical and elongated in shape and runs parallel and outside to the pterygomandibular raphe or ligament (medial limit) (Figure 16.6) (Khoury et al. 2011). Its lateral limit is the deep tendon that attaches the temporal muscle to the temporal crest, exactly where the finger is rested on the coronoid notch (Figure 3.14, Chapter 3) and thus highlights the pterygotemporal depression.
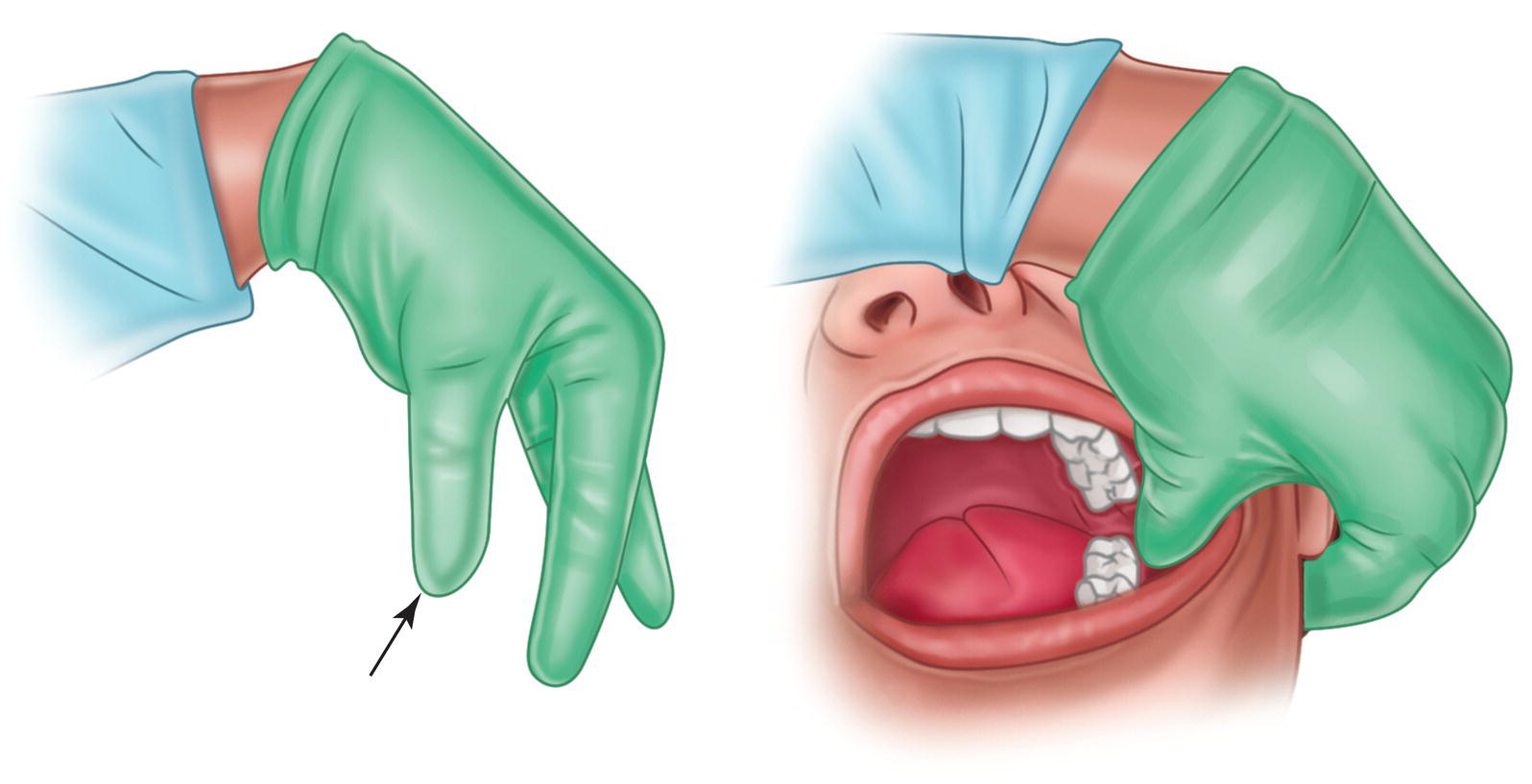
Figure 16.4 Thumb of non‐injection hand inside patient’s mouth for approach from left side, with dentist’s palm and wrist blocking patient’s vision.
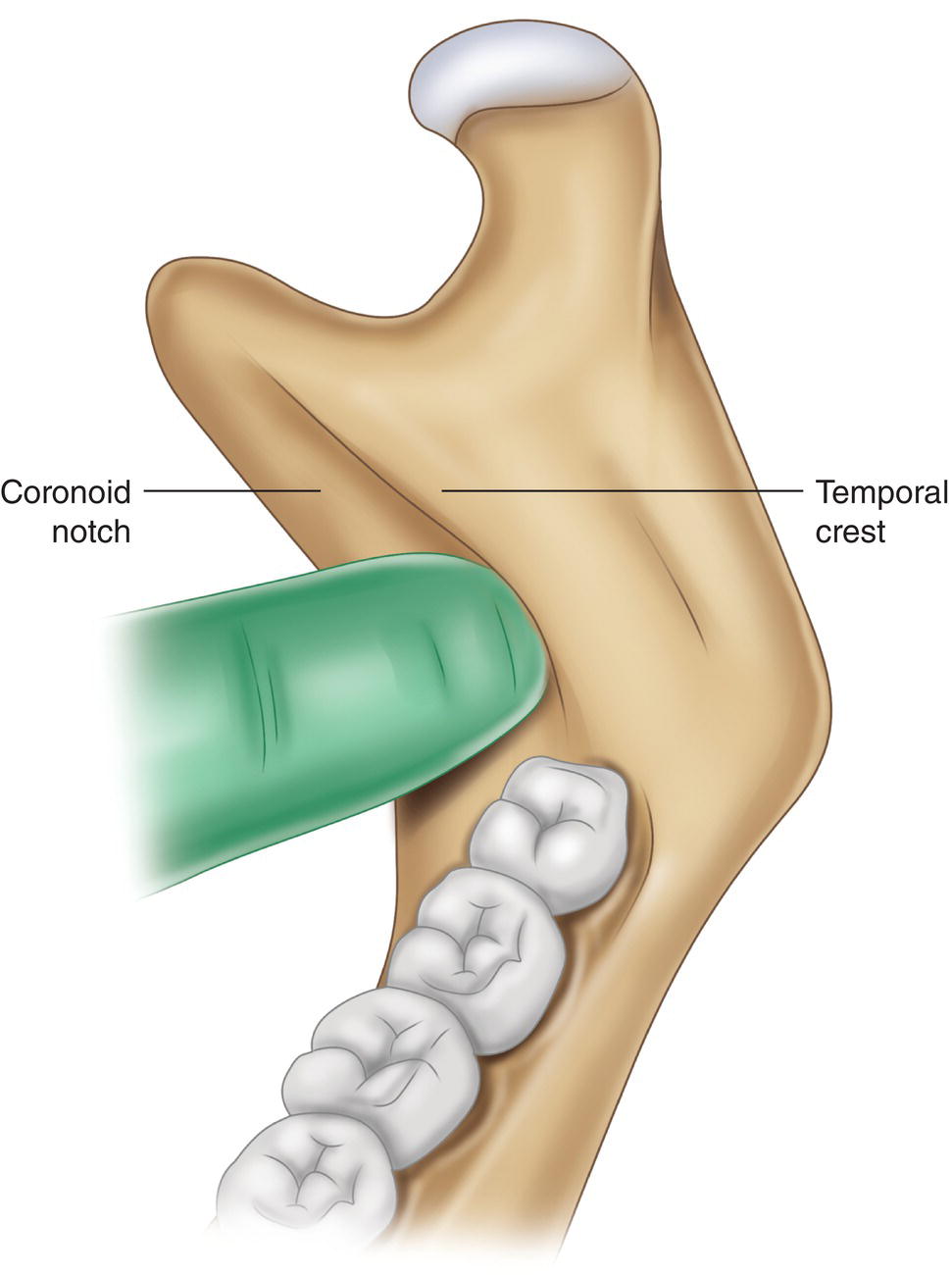
Figure 16.5 Intraoral index finger or thumb resting on the anterior edge of the mandible in the hollow of the coronoid notch.
Source: Redrawn from Evers and Haegerstam (1981).
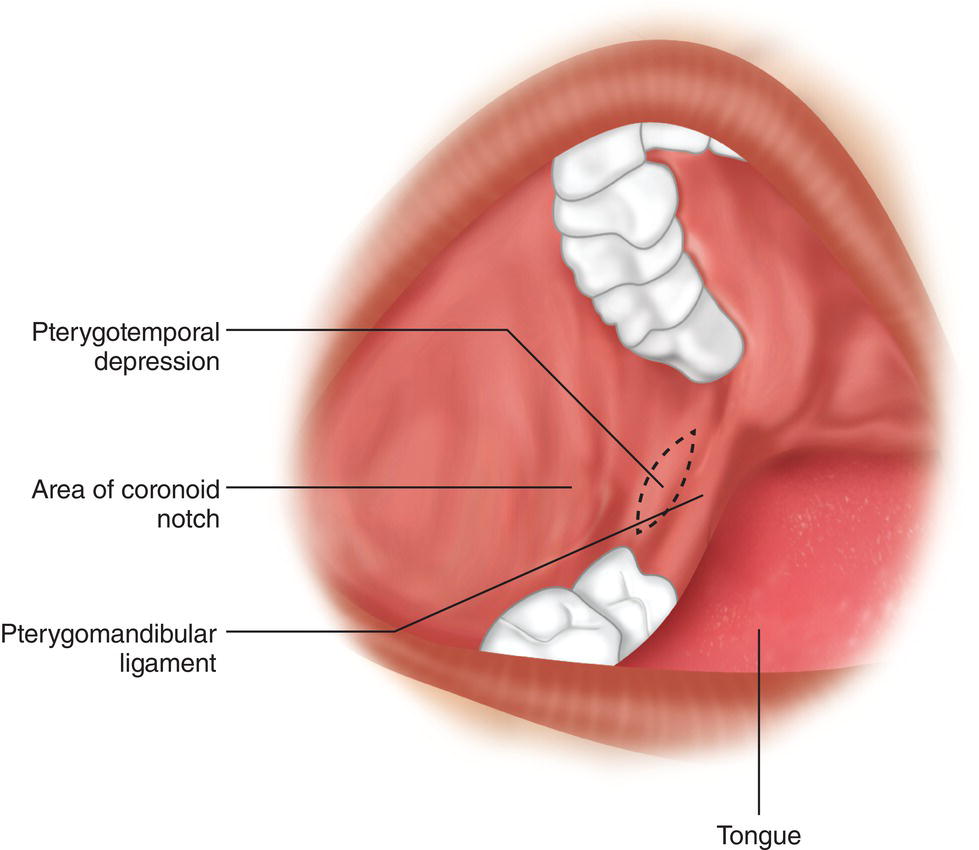
Figure 16.6 Pterygotemporal depression outward of the pterygomandibular ligament or raphe.
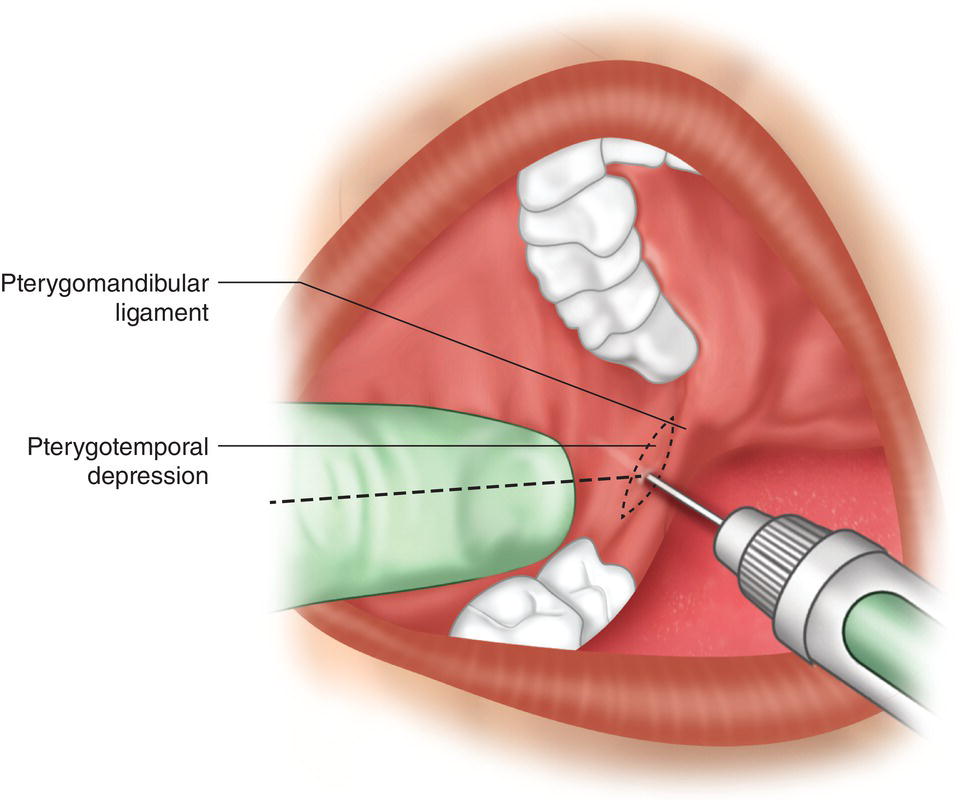
Figure 16.7 Needle insertion site in conventional technique outside the pterygomandibular ligament, in the pterygotemporal depression, around 10 mm over the occlusal plane of the mandibular molars, with imaginary line projected distally from mid‐finger to help find the insertion site.
Some clinicians draw an imaginary line along the middle of the intraoral finger, parallel to the occlusal plane, and project it distally to pinpoint the insertion site (Figure 16.7).
In children under the age of 7 years (Via 1953) and in 35% of adults (Angelman 1945) this depression and its vertex lie under a mucosal pad and are difficult to distinguish (Lindsay 1929b). In such cases, the tip of the intraoral finger should stretch the proximal buccal mucosa and insert the needle outside the pterygomandibular ligament (always present), in the area where the vertex of the pterygotemporal depression is assumed to lie (Lindsay 1929b).
- Injection height.
- A site around 10 mm above the occlusal plane of the mandibular molars is recommended because in 95–100% of cases this ensures by‐passing the lingula (Table 3.7, Chapter 3), leaving the path to the sulcus colli clear.
- The exception is the occlusal plane of the third molar (wisdom tooth), unless it is aligned with the other two molars (Bremer 1952). The occlusal plane of the premolars can also be used as a reference if the molars are missing.
- One aid to finding the insertion height is, as noted earlier, to draw an imaginary line backwards down the middle of the finger on the non‐injection hand (that rests on the coronoid notch) toward the pterygotemporal depression (Figure 16.7) (Angelman 1945).
- Modification of the injection height.
- It should be higher (>10 mm) in:
- Toothless patients, for as the alveolar ridge is reabsorbed, the lingula is higher.
- Patients with a wide gonial angle and wide ramus of the mandible, typical of class III Angle’s malocclusion with mandibular hyperplasia (Hetson et al. 1988).
- It should be lower (<10 mm) in:
- Children under 10 years and especially children under 6 years (Benham 1976) (Table 3.8, Chapter 3) (Figure 16.8).
- Patients with a narrow gonial angle and ramus of the mandible, typical of class II Angle’s malocclusion with mandibular hypoplasia (Hetson et al. 1988).
- Some clarifications are in order regarding modification in height.
- In patients with a wide gonial angle and narrow ramus of the mandible or vice versa, the needle insertion height should be 10 mm.
- Between its posterior and anterior the ramus of the mandible is 30 mm wide on average, ranging from 20 to 40 mm (Table 3.6, Chapter 3).
- The gonial angle is 120° on average, but may range from 93° to 143°.
- Syringe direction.
- In around 90% of cases the syringe is positioned over the mandibular premolar zone on the opposite side, with the needle traveling toward the pterygotemporal depression and touching bone at the sulcus colli.
- The divergent angle between the ramus of the mandible and the sagittal or medial plane is 0–27° (Figure 3.11, Chapter 3). In the nearly 10% of cases where it is greater than 18° (Simon and Kömives 1938), the syringe must be positioned further back to reach the sulcus colli, alongside the mandibular molars, for with such a wide angle, if it lies above the premolars the needle would run behind the ramus of the mandible without touching bone (Figure 16.9).
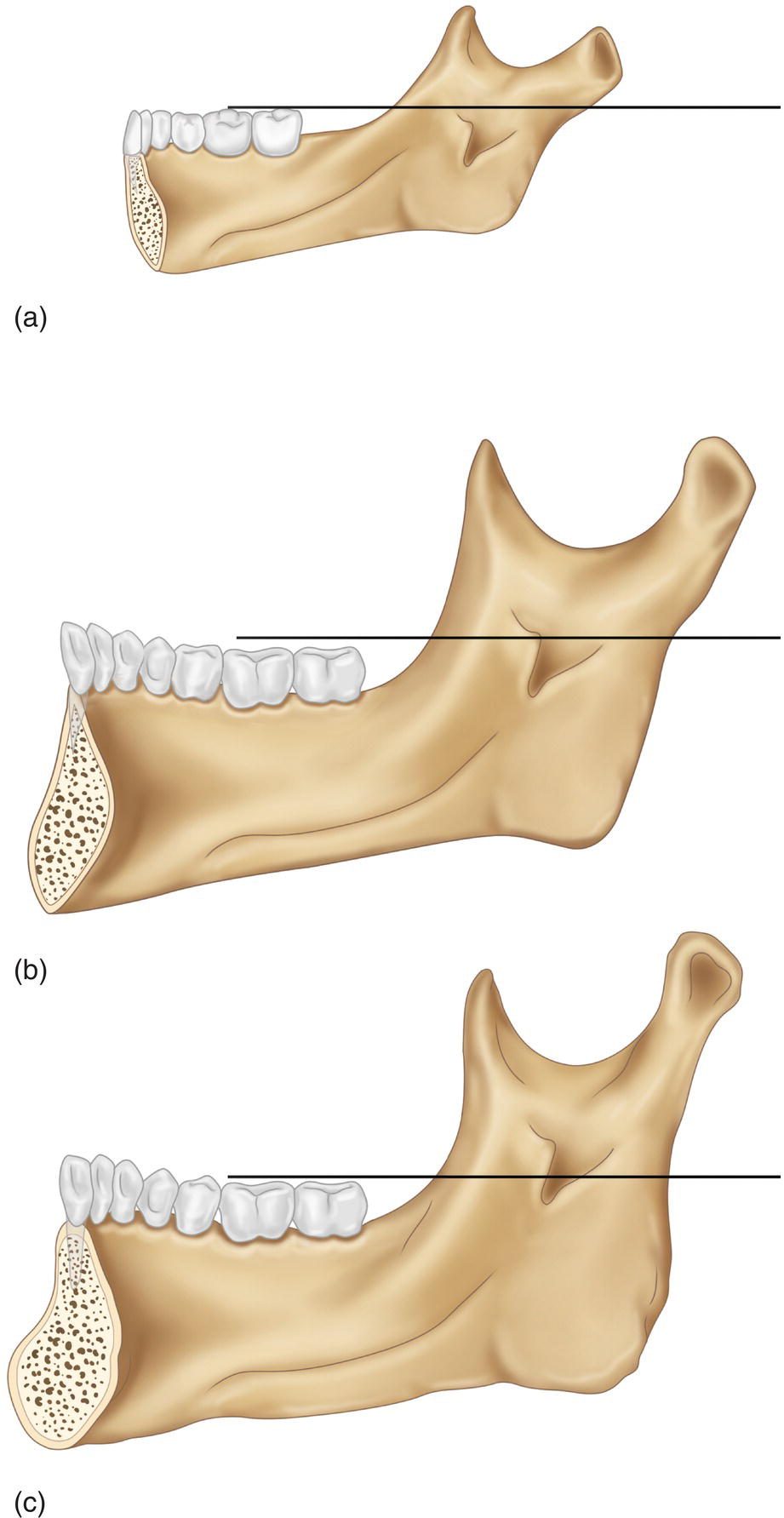
Figure 16.8 Height of lingula relative to occlusal plane in (a) 4‐year‐old child, (b) 8‐year‐old child, and (c) adult.
- Needle insertion. The following is recommended to minimize discomfort associated with injection:
- The intraoral finger should stretch and tighten the mucosa overlying the pterygotemporal depression.
- A light but firm tap followed by quick insertion is regarded as the optimal technique. The site is lightly but firmly tapped with the non‐dominant hand while at the same time quickly inserting the needle to hit bone. This maneuver is crucial because if the pain threshold’s peak traumatic stimulus (the needle advancing through the soft tissues) lasts too long it will exceed the initial threshold, giving rise to pain (Fuller et al. 1979). Slower insertion triggers the initial threshold and if a few drops of anesthetic are injected as the needle advances the pain rises (Nusstein et al. 2006; McCartney et al. 2007; Chapter 13 Appendix); moreover, the anesthetic does not take immediate effect. The factor that causes most pain in truncal blocks is needle movement (Annex 23).
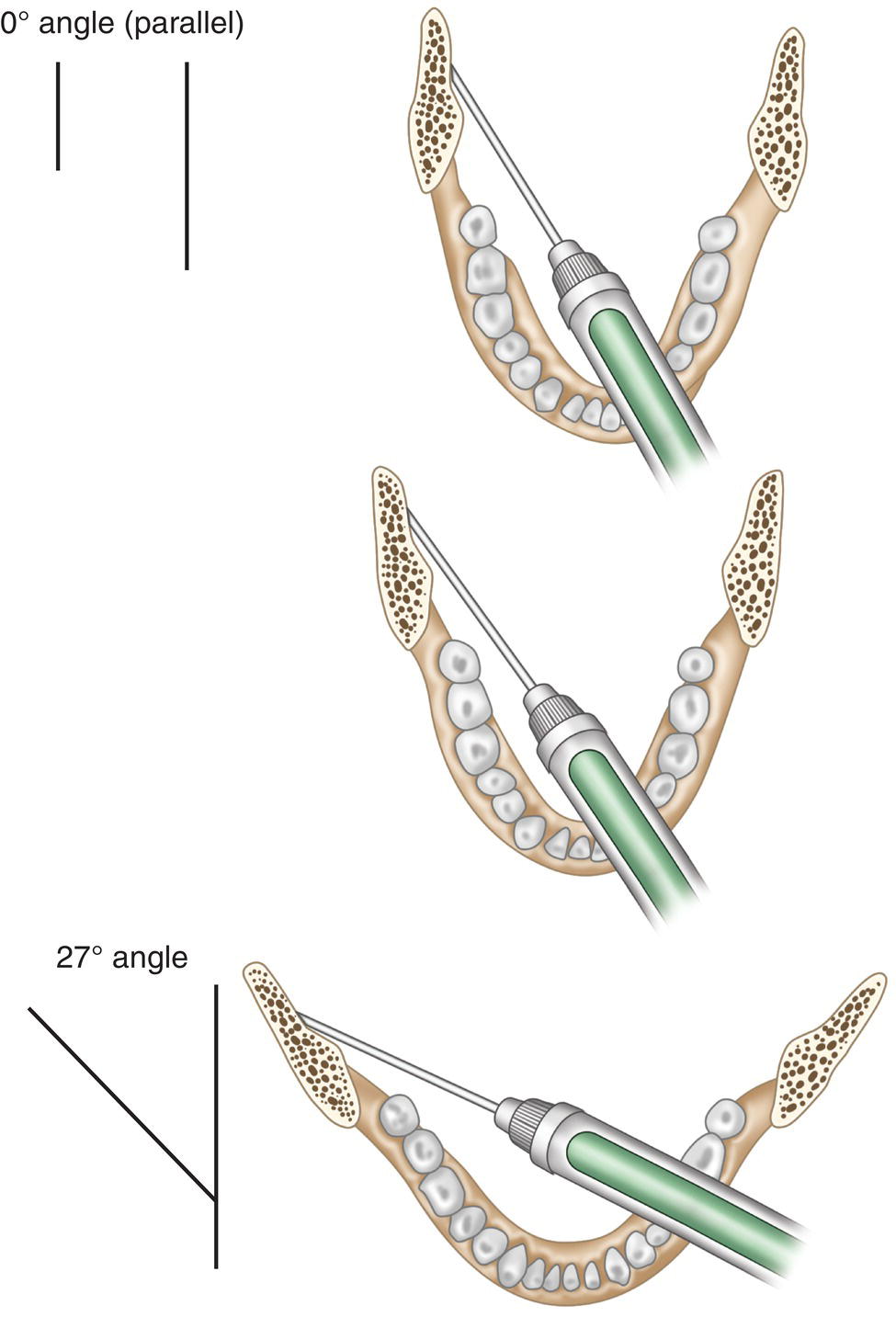
Figure 16.9 Syringe positioned at contralateral mandibular molars (rather than premolars) when the divergent angle of the ramus of the mandible is >18° (conventional approach).
Source: Redrawn from Roberts and Sowray (1987).
- Insertion depth.
- The insertion depth is the distance between the anterior edge (pterygotemporal depression) and the sulcus colli, where the inferior alveolar nerve lies in a wide‐open mouth. That distance is around 20–25 mm, ranging from 15 to 30 mm (Table 16.4), and in children under 6–8 years old it is 15–20 mm.
- Inserting the needle into the hub is a technical error for two reasons: this is the weakest area and may result in needle breakage as well as the fact that the depth is excessive to hit the landmarks for anesthesia of the inferior alveolar nerve.
Table 16.4 Needle insertion depth in soft tissue in conventional mandibular block.
Reference Sample size Factor assessed Mean (mm) Range (mm) Angelman (1945) 300 Patient — 18–33 Bremer (1952) 100 Dry mandible 24 ± 3.1 16–32 Waikakul and Punwutikorn (1991) 68 Patient 20–25 — Kronman et al. (1994) 39 Corpse 22 ± 1.8 15–28 Delgado‐Molina et al. (1999) 246 Patient 21 10–34 Hannan et al. (1999) 40 Patient 19 18–20 Tofoli et al. (2003) 20 Patient 20–25 — Simon et al. (2010) 38 Patient 19 ± 3.2 — Mean 21.7 15.4–29.4 Rounded mean 20–25 15–30 - The insertion depth may vary (Angelman 1945) depending on:
- The divergent angle between the ramus of the mandible and the sagittal or medial plane; the greater the divergent angle, the deeper the insertion.
- The width of the ramus of the mandible; the wider, the deeper.
- The thickness of the mucosa and adipose tissue that comprise the wall of the pterygotemporal depression; the thicker, the deeper.
- Interestingly, the dimensions in a given individual may vary by 1–4 mm between sides (Angelman 1945).
- If the needle is not successfully inserted because it fails to touch bone after 30 mm or because it touches bone too soon, in less than 15 mm, the recommendation is to aspirate and slowly remove the needle, injecting 0.25 to 0.5 of a cartridge (0.5–0.9 ml) to anesthetize the pterygomandibular space and facilitate a second, less painful maneuver in a second attempt after a 1‐minute wait.
- The insertion depth may vary (Angelman 1945) depending on:
- Pre‐injection aspiration.
- Once bone has been reached with the tip of the needle the clinician should avoid exerting undue pressure to prevent injury to the periosteum (causing post‐injection pain) and barb formation on the tip of the needle. If a barb forms outwardly, when the needle is withdrawn from the pterygomandibular space, the following structures may become injured: nerves (leaving persistent paresthesia in the lingual or inferior alveolar nerves), muscles (trismus due to injury to the medial pterygoid or temporal muscles), and the inferior alveolar artery and vein (hematoma) (Stacy and Hajjar 1994).
- After touching bone the needle is drawn back 1–2 mm to aspirate. Aspiration is positive in 10% of cases (Annex 22), one of the highest rates in dental local anesthesia.
- Injection of the anesthetic solution and lingual nerve anesthesia.
- A 1.8‐ml cartridge should be slowly injected, in 40–60 seconds. To anesthetize the lingual nerve the needle is slowly withdrawn along the same path as it was inserted through; at mid‐distance and prior to removing the needle, a second aspiration is performed and the last ±0.3 ml in the cartridge is injected to anesthetize the lingual nerve.
- In the absence of this maneuver, the lingual nerve is often anesthetized by diffusion across the pterygomandibular space. However, this maneuver ensures anesthesia of the lingual nerve.
- Many clinicians aspirate every 0.25–0.50 ml, seeking to further guarantee the safety of the injection with a series of negative aspirations (McClure 1968; Lloyd 1992); this also helps retard the injection by curbing the natural tendency to move faster.
- Amount to be injected
- In adults, teenagers, and older children, a 1.8‐ml cartridge is used (1.5 ml during deposition and ±0.3 ml while removing the needle to anesthetize the lingual nerve).
- In children <6–8 years old, only ½ of a cartridge is needed.
- Subjective symptoms of anesthesia.
- Soft tissue anesthesia appears in the lower lip on the anesthetized side. Soft tissue anesthesia may be described as tingling, numbing, itching, dullness, feeling “pins and needles,” and feeling a “fat lip” sensation (Table 13.1, Chapter 13). The onset of soft tissue anesthesia is approximately 2 minutes after injection (Annex 27) and in nearly 90% of cases in less than 5 minutes (Annex 28).
Table 16.5 Electric pulp tester readings of anesthesia in first mandibular molar after conventional mandibular block with a supplemental buccal injection using A‐100 anesthetic solution.
Mandibular block Supplementary buccal infiltration Success rate (%) Reference ml/LAS ml/LAS (absolute values) Haase et al. (2008) 1.8/A‐100 1.8/A‐100 96% (70/73) Kanaa et al. (2009) 2.0/L‐80 2.0/A‐100 92% (33/36) Gazal (2015) 1.8/M‐100 1.8/A‐100 100% (23/23) Mean 96% ≈ 95% LAS, local anesthetic solution; A‐100, 4% articaine with 1:100 000 (10 μg/ml) epinephrine; L‐80, 2 lidocaine with 1:80 000 (12.5 μg/ml) epinephrine; M‐100, 2% mepivacaine with 1:100 000 (10 μg/ml) epinephrine.
- In approximately 10% of cases the lower lip is not anesthetized in the first 5 minutes (Annex 28). Such cases are regarded as failures in practice and a second mandibular block is recommended (Cohen et al. 1993; Reisman et al. 1997; Nusstein et al. 1998; Fan et al. 2009).
- Soft tissue anesthesia is denoted by the following.
- In the lower lip ipsilateral to the injection site it is a sign of anesthesia of the inferior alveolar nerve, the primary aim of the procedure.
- In the tongue ipsilateral to the injection site it is an indication of anesthesia of the lingual nerve. In 50% of cases, this precedes lip numbness (Angelman 1945; Ay et al. 2011).
- In the auricular and temporal region ipsilateral to the injection site it is a sign of anesthesia of the auriculotemporal nerve. With this technique it occurs in only 20% of cases (Kim et al. 2003).
- Supplemental buccal infiltration.
- After the first 5 minutes soft tissue anesthesia appears in the lower lip (an initial sign of mandibular block onset), verifying anesthesia of the inferior alveolar nerve, and supplementary buccal infiltration is recommended in posterior mandibular teeth requiring good pulpal anesthesia. This procedure raises the pulpal anesthesia rate from 60–70% (Table 16.1) to 95% (Table 16.5).
- The infiltration is performed after 5 minutes to avoid the risk of masking or concealing mandibular block failure due to the overlapping of the effects of mandibular block and infiltration in the soft tissue.
- The infiltration anesthetics recommended are:
- In adults a potent solution such as a whole cartridge (1.8 ml) of 4% articaine with 1:100 000 epinephrine (A‐100) on the buccal aspect of the posterior teeth to be treated.
- In teenagers and older children, a cartridge (1.8 ml) of the standard lidocaine solution (L‐100).
- In children under 6–8 years, half a standard L‐100 cartridge (0.9 ml).
- It takes an additional 5–10 minutes (10–15 minutes in all after starting mandibular block) for pulpal anesthesia to be fully effective.
- Duration of soft tissue anesthesia. This usually lasts 3–4 hours (200 minutes), a fact of which the patient should be notified after treatment.
- Injection height.
Efficacy of this Technique
The efficacy of this technique, measured with an electric pulp tester in posterior teeth after injection of one or two cartridges of standard 2% lidocaine with 1:100 000 epinephrine (L‐100), is 60–70% after 10–15 minutes (Table 16.1) and 95% when reinforced by buccal infiltration with 1.8 ml of a potent solution such as 4% articaine with 1:100 000 epinephrine (A‐100) (Table 16.5).
When measured with less rigorous methods such as the system to determine grade A anesthesia used for routine procedures (normally extractions), the success rate for non‐reinforced mandibular block is 85% (Annex 30).
Complications Specific to this Technique
- Technical error. Inappropriate maneuvering leads to failed mandibular block and other complications, depending on the injection position (Figures 3.13 and 3.14, Chapter 3
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


