17
Mandibular Anesthesia II: Complementary Anesthesia
Introduction
Mandibular block does not always lead to anesthesia of the lingual nerve, and, therefore, of the tissue in the area of the tongue. Similarly, it does not anesthetize the buccal nerve or the tissues of the buccal area of the molars (Annex 29). Consequently, when working on the soft and hard tissue in this area, it is appropriate to anesthetize these nerve trunks.
The potency of anesthetic solutions – in terms of the anesthetic itself and the concentration of anesthetic and vasoconstrictor – is not important for surgery will be successful, since the buccal and lingual nerves are very superficial and not covered by periosteum, cortex, or aponeurosis. They therefore become anesthetized with a small volume of anesthetic solution. In this chapter, we review the following techniques:
- lingual nerve block
- buccal nerve block.
Indications
These techniques do not aim to achieve pulpal anesthesia but rather complementary anesthesia for mandibular block in the following cases:
- Oral surgery and extractions.
- Scaling and root planning.
- Subgingival preparations in the following cases:
- Subgingival restorations.
- Restorations by cervical caries.
- Placement of a retraction cord.
- Retraction of the gingiva at the level of the papilla.
- Insertion of subgingival matrix bands.
- Placement of clamps for a rubber dam that penetrate or pinch the gum in the buccal or lingual area.
Lingual Nerve Block
The lingual nerve is generally anesthetized using mandibular block techniques (Annex 29). However, when this approach is unsuccessful or it is necessary to anesthetize the lingual nerve only, the technique is simple and almost 100% successful because the nerve is both superficial and accessible.
Anesthetized Area
The anesthetized area corresponds to the whole area supplied by the lingual nerve (see Chapter 3). This includes the following:
- Fibromucosa (alveolar mucosa and attached gum), bone, and periosteum in the lingual area of the whole ipsilateral hemimandible up to the midline.
- Fibromucosa of the floor of the mouth on the ipsilateral side up to the midline.
- Anterior two‐thirds of the tongue, on the ipsilateral side up to the midline. The nerve also provides proprioceptive sensation to the musculature of the tongue (Barker and Davies 1972).
Technique
- Use a long needle (35 mm) owing to the very posterior position to be reached (here, the depth of the insertion is not important). The caliber used is 25G or 27G: as the technique is often complementary to mandibular block, we generally use the same needle.
- Position of the dentist and patient.
- Dentist at 8:00–9:00 o’clock.
- Patient semireclined with the head slightly turned toward the dentist. The patient’s mouth is held wide open so that the dentist can reach the floor of the mouth.
- Separation of the tongue. Using a mirror in the support hand (left hand in right‐handed persons), the dentist gently separates the tongue from the lingual surface of the second and third mandibular molars, thus revealing the floor of the mouth at this level (Figure 17.1).
- The point of insertion of the needle is located on the floor of the mouth alongside the second and third molars (Sicher 1946) because at this level the lingual nerve enters the floor of the mouth relatively close to the lingual bone plate. The nerve then courses forward within the floor of the mouth, pulling away from the lingual bony plates, and advances toward the center/interior to reach the base of the tongue (Figure 17.2).
- The needle is inserted 2–4 mm into the floor of the mouth. The insertion is short since the nerve runs below the mucous membrane but above the mylohyoid muscle (Figure 3.4, Chapter 3), which forms the base of the floor of the mouth.
- The injection is performed following the minimum intervention technique (minimum volume/minimum injection time), which considerably reduces the pain caused by the injection. The procedure is as follows:
- Initially inject only one or two drops of anesthetic solution in 1–2 seconds and wait 60 seconds after withdrawing the needle. Thus, the soft tissue is anesthetized at the injection site.
- Perform a second injection at the same site (the blood spot formed by the first injection may be visible). Again, inject one or two drops over 1–2 seconds. This time wait only 30 seconds after removing the needle.
- After aspiration, perform a third injection at the same site. However, this time the amount of anesthetic is larger (±1/8 of a cartridge, 0.2–0.25 ml) and is injected slowly over 7–10 seconds. Wait 30 seconds.
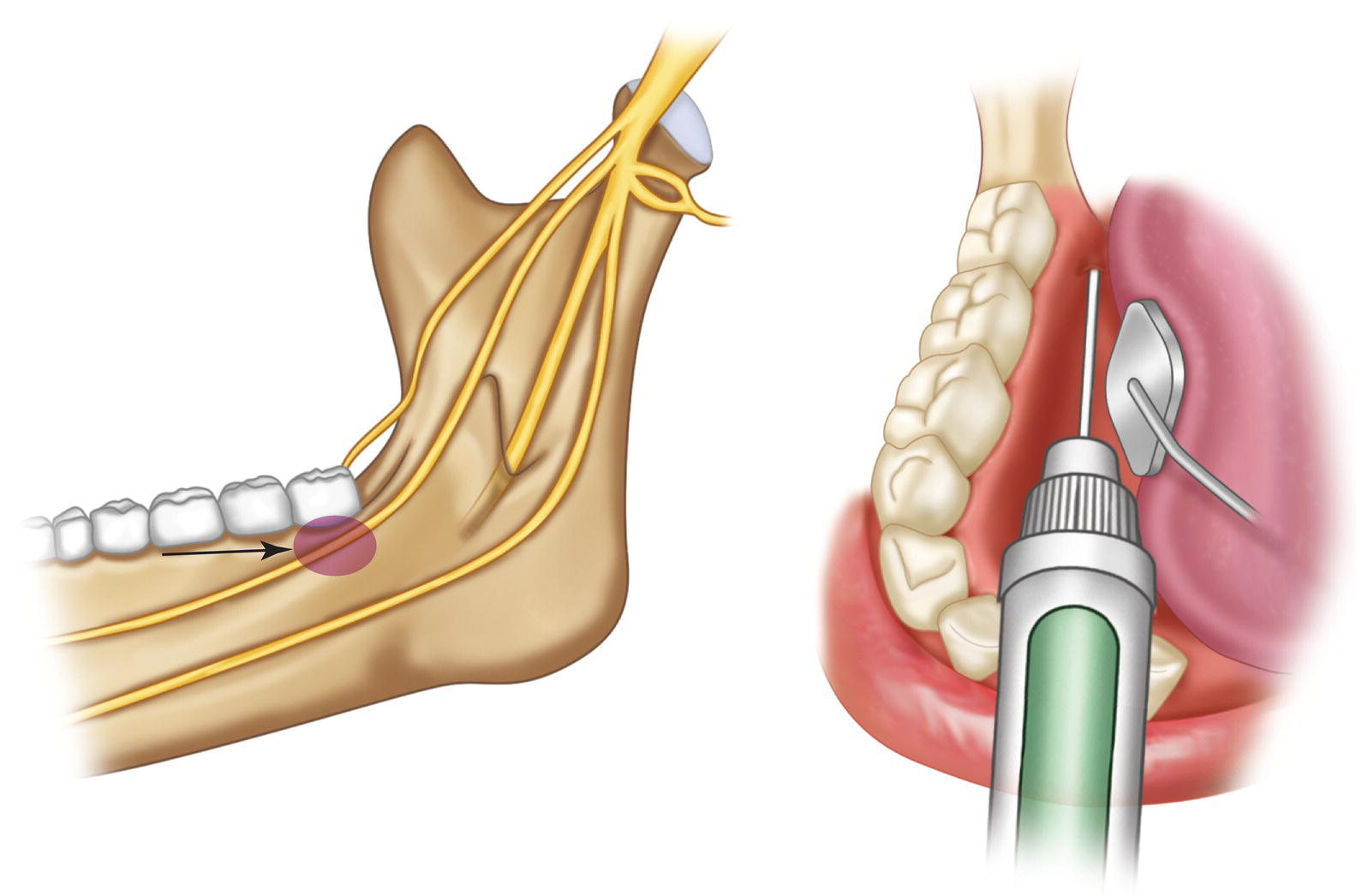
Figure 17.1 Anesthesia of the lingual nerve. Injection site.
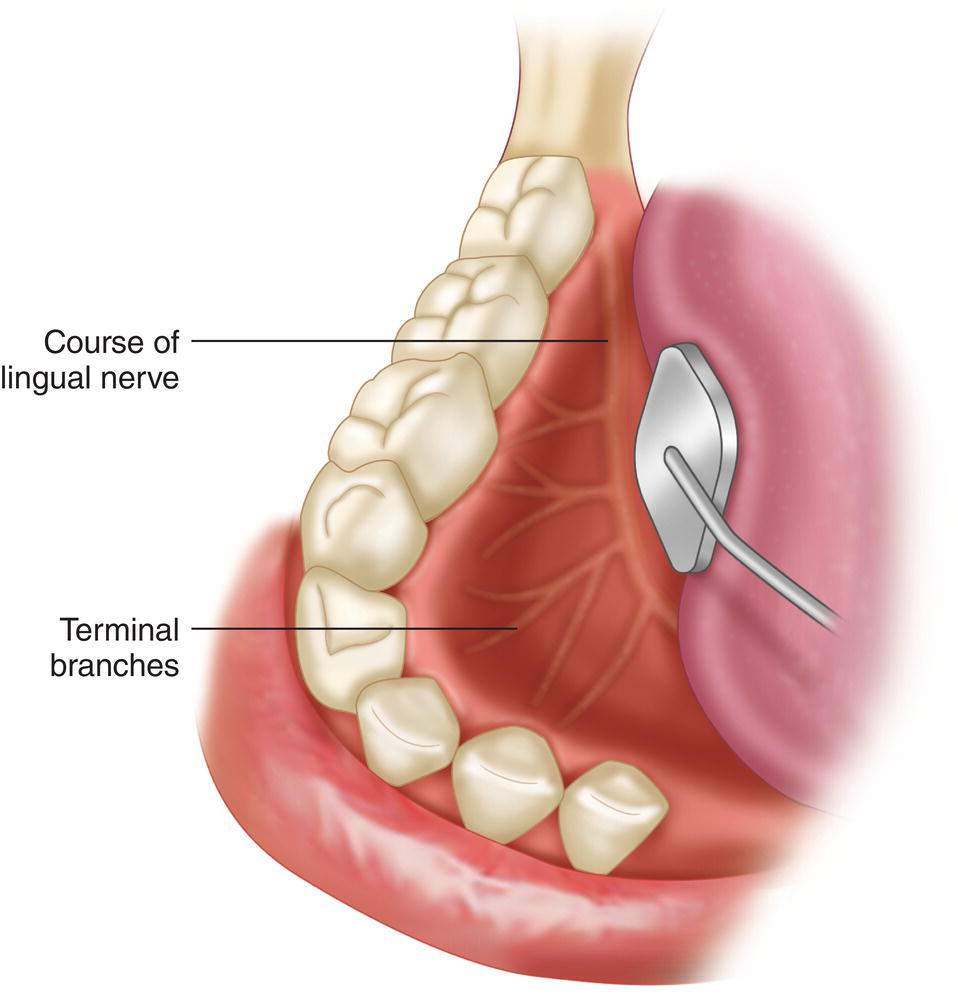
Figure 17.2 Course of the lingual nerve along the floor of the mouth and its terminal branches.
- Aspiration is positive in 1% of cases (Annex 22).
- Subjective symptoms of soft tissue anesthesia, defined by patients as dullness, numbing, tingling, and swollen tongue sensation (Table 13.1, Chapter 13) in the anterior and lateral areas of the tongue, appears after a few minutes and lasts 1–2 hours.
Complications of this Technique
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


