18
Supplementary Techniques in Cases of Failure
Introduction
Supplementary techniques are applied only in the case of failure of conventional local anesthetic techniques, such as those mentioned above, therefore they are not first‐choice, primary techniques. All of these techniques have special characteristics:
- They are sufficiently powerful to achieve pulpal anesthesia.
- They are self‐limiting in their extension and their effect is very localized (they cover very few adjacent tissues), therefore they are not efficacious as primary techniques in the case of wider procedures that involve both soft and hard tissue.
- Their action is independent of anatomical variations, such as accessory innervations or cortical thickness, which usually affect the efficacy of conventional techniques.
- Anesthetic solutions enter the bloodstream easily and quickly, therefore it is important to take into account the following:
- The total dose administered is limited. Their advantage is that the dose required is very low.
- Aspiration is unnecessary since this is very often positive (almost intravascular).
- Anesthetics with a long‐lasting effect in the soft tissues, such as bupivacaine, etidocaine, and ropivacaine, are contraindicated because they do not improve the efficacy of pulpal anesthetic (Johnson et al. 1985; McLean et al. 1992; Hull and Rothwell 1998; Meechan 2002). In addition, since they enter the systemic bloodstream easily, they increase toxicity.
- They are usually painful when used as primary techniques.
In this chapter, we shall address four techniques. However, the intraseptal technique can be considered a hybrid of the periodontal ligament technique (PDL) and intraosseous techniques. The techniques are as follows:
- Intrapulpal.
- PDL.
- Intraseptal.
- Intraosseous.
Intrapulpal Anesthesia
This supplementary technique is applied when traditional methods fail, therefore the adjacent tissues are usually anesthetized, even if the dental pulp remains sensitive. The method consists of the injection of anesthetic solution directly into the dental pulp when the chamber is open. This approach is indicated in two situations:
- In endodontic treatments, where the pulp chamber is open and remains sensitive to contact with instruments (the most common situation).
- In surgical extractions in which the tooth is cut and remains sensitive (Berini and Gay 1997).
Below, we analyze two intrapulpal techniques, as follows:
- The traditional technique (the most frequent).
- The topical anesthesia technique.
Traditional Technique
Keys to a Successful Approach
- The pressure of the injection of anesthetic solution on the pulp (Birchfield and Rosenberg 1975; Van Gheluwe and Walton 1997). Experiments have shown that 100% of injections are unsuccessful if there is no pressure (Van Gheluwe and Walton 1997) and that injection of saline solution under pressure can be effective in a high percentage of patients (Birchfield and Rosenberg 1975; Van Gheluwe and Walton 1997).
- An anesthetic solution with vasoconstrictor such as the standard solution of lidocaine 2% with epinephrine 1:100 000 (10 μg/ml) (L‐100). Experiments have shown that a 90% success rate is achieved with saline solution, but that a 100% success rate is achieved with L‐100 (Van Gheluwe and Walton 1997). Higher concentrations of anesthetic and/or vasoconstrictor are not recommended because the anesthetic solution passes easily into the systemic bloodstream (Lamian and Simard‐Savoie 1979; Smith and Smith 1983a), although this step is limited by apical constriction and residual pulp (Smith and Smith 1983a).
These recommendations enable 100% pulpal anesthesia, even in patients with irreversible, anesthetic‐resistant acute pulpitis (Dreven et al. 1987; Cohen et al. 1993; Nusstein et al. 1998: Parente et al. 1998).
Intrapulpal Technique
- 27G or 30G short needle (20–25 mm). If the needle is to be inserted into the radicular pulp canal, then the finer the better. It is usually necessary to bend the needle along its stem to facilitate insertion. The needle should not be bent at the hub, which is the weakest part and where it most commonly breaks.
- A little hole should be made in the pulp chamber to insert the needle. If the hole is too big, the anesthetic cannot be inserted under pressure and the solution will leak from the chamber. This can be avoided by placing a cotton wool ball in tweezers and pressing it against the needle inserted into the chamber to prevent reflux and maintain pressure (Walton 1990) (Figure 18.1).
- The patient should be warned that he/she will feel “intense discomfort” at the beginning of the injection, although this will be very brief (Miles 1983).
- The needle should be placed firmly with the fingers in the orifice and a few drops should be injected under pressure into the pulp chamber. In the case of multirooted teeth, if discomfort is felt in a canal as result of the instruments, the tip of the needle is inserted into the entrance of the canal, the needle is held firmly, and the solution is injected under pressure in such a way that it reaches the apex (Smith and Smith 1983a). If it is not possible to maintain pressure, place a cotton ball (see above) to maintain pressure and prevent reflux.
- After the injection, wait 30 seconds before starting to work. The anesthetic is working if the instruments can be introduced into the canals without pain. If the patient continues to experience discomfort, repeat the maneuver with emphasis on maintaining pressure (Van Gheluwe and Walton 1997).
Topical Anesthetic Technique
This approach involves placing topical anesthetic gel (generally benzocaine 20%) into the root canals with endodontic files (DeNunzio 1998). Although this technique can be used as an alternative to the traditional technique, it is mainly used in cases of sensitive, twisted, and narrow canals where the needle cannot be appropriately positioned to maintain injection pressure.
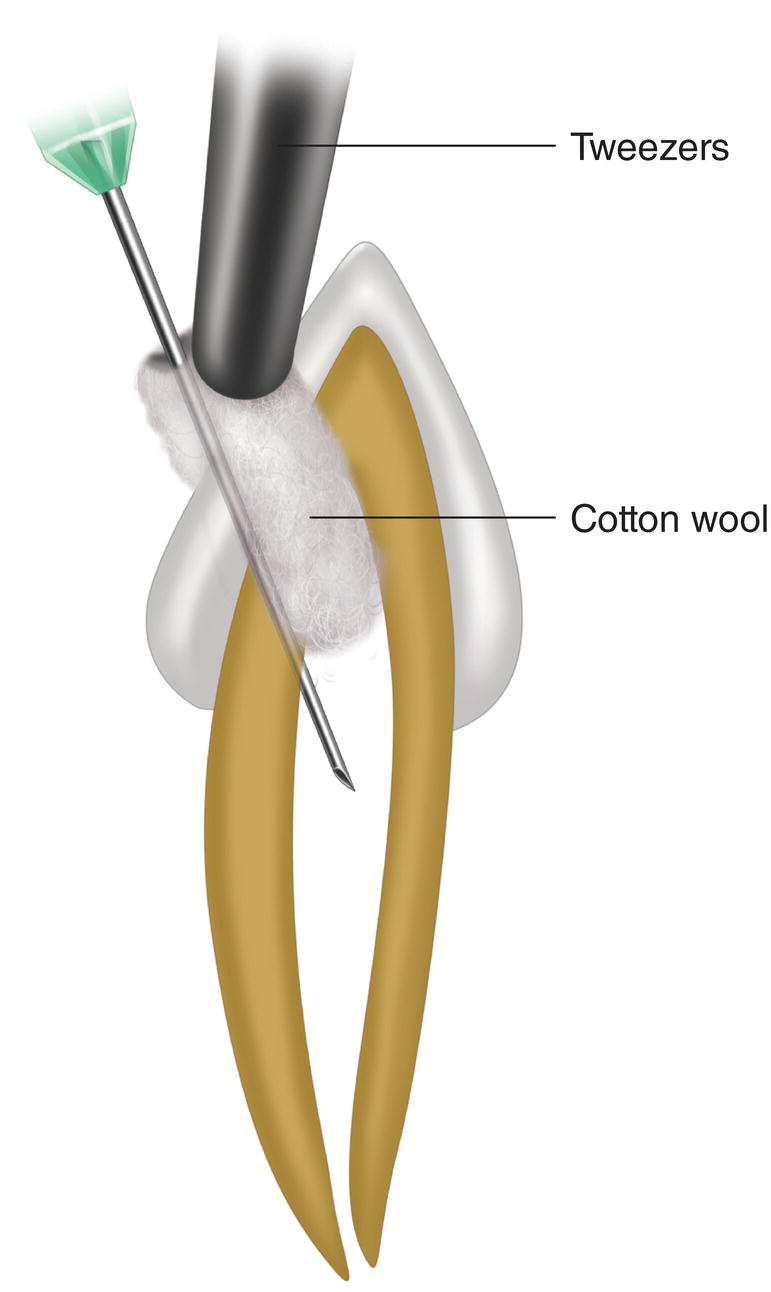
Figure 18.1 Traditional intrapulpal technique in which a cotton wool ball has been placed in the pulp chamber to prevent reflux and maintain pressure during the injection.
Technique
- Cover the tip of a no. 10 or 15 file with benzocaine 20% gel. It is very important for the gel to be viscous so that it adheres to the metal, therefore it should be kept at a low temperature. If the gel is very thin, having a liquid‐like consistency due to high ambient temperatures, it can be placed in the refrigerator.
- Insert the file into the canal and file for a few seconds. One or two applications is usually sufficient, except in extremely sensitive patients, who may require more time and more applications.
- Any benzocaine gel remaining in the chamber can act as a reservoir for anesthesia of other canals in multirooted teeth.
- Once anesthesia is achieved, abundant irrigation can be applied to remove any remaining anesthetic from the canal. If irrigation is with hypochlorite, the benzocaine can turn a dark reddish‐orange color. This also occurs if benzocaine mixes with blood. The color has no clinical relevance.
Periodontal Ligament Technique (PDL)
This technique is also known as the intra‐alveolar, intraperiodontal, intrasulcular, intraperiosteal, transligamentary, intraligamentary, or peridental technique (Nevin and Puterbaugh 1949; Mulkey 1976). The method involves trying to inject the anesthetic solution under pressure across the periodontal ligament and cancellous bone to reach the apex.
According to Nevin and Puterbaugh, this technique was first used in 1895 (Nevin and Puterbaugh 1949). The oldest reference we were able to find was by Emilie Sauvez from Paris in 1905 (Sauvez 1905), although it is not referenced as the original. Cassamani wrote a doctoral thesis on this technique in 1924 (Cassamani 1924), but this remained outside the scientific literature until the 1970s, when it was discussed in the studies of Robert Lafargue and Chenaux (Lafargue 1973; Chenaux et al. 1976). In 1981, a study by Richard Walton and Bernard Abbott made this technique known in English (Walton and Abbott 1981). Since then the number of his published scientific studies has increased.
Indications and Contraindications
Indications
- When the habitual anesthetic techniques fail (Council on Dental Materials, Instruments, and Equipment 1983; Johnson et al. 1985; Cowan 1986; Walton 1990; Meechan 1992). This is the basic indication since the duration of pulpal anesthesia is short and post‐injection discomfort is common, as is the risk of periodontal lesions (see below).
- In patients with severe hemophilia‐associated coagulation disorders (Sachs et al. 1978; Pin 1987; Spuller 1988) or patients with high international normalized ratio (INR) taking anticoagulants (see Chapter 8), truncal block techniques (such as mandibular block, high‐tuberosity technique, or transpalatal technique) can be replaced by the PDL technique.
Contraindications
- In primary teeth (Brännström et al. 1984). Even though experimental studies in animals have demonstrated that solution injected using this procedure is distributed between the bony crypt and the enamel organ without penetrating the organ and with minimal apparent risk (Tagger et al. 1994a), experiments in monkeys revealed increased enamel abnormalities in the permanent teeth below the primary teeth that are injected using the PDL technique (Brännström et al. 1984), although these abnormalities are minimal. The exceptions to this contraindication are as follows:
- Children with severe coagulation abnormalities (Spuller 1988) (see above).
- Computer‐controlled PDL injections (The Wand) because pressure is controlled (Table 18.2) and there are no enamel abnormalities (Ashkenazi et al. 2010).
- Teeth with advanced periodontal disease (Rakusin et al. 1986), given that this can compromise periodontal support. Logically, teeth with periodontal disease that are to be extracted are an exception.
- Infection at an injection site with cellulitis or abscess, given that this can be very painful and it may not be possible to achieve deep anesthesia (Reader et al. 2011; Council on Clinical Affairs 2015).
Diffusion of the Solution
With the needle inserted in the gingival sulcus and firmly placed between the alveolar crest and the neck of the root of the tooth, the strong pressure exerted on the anesthetic solutions leads the solution to diffuse through two sites (Figure 18.2):
- The periodontal ligament (Dreyer et al. 1983; Fuhs et al. 1983). Small quantities pass through to the periodontal ligament. Larger quantities cannot pass in humans, the width of the ligament is 0.13–0.21 mm (Coolidge 1937), the interval ranges from 0.06 to 0.35 mm (Kronfeld 1931), and the finest 30G needle has a caliber of 0.3 mm, thus restricting direct passage to the ligament. However, part of the solution penetrates via the alveolar wall fenestrations to reach the medullary cavities of the alveolar bone (Garfunkel et al. 1983).
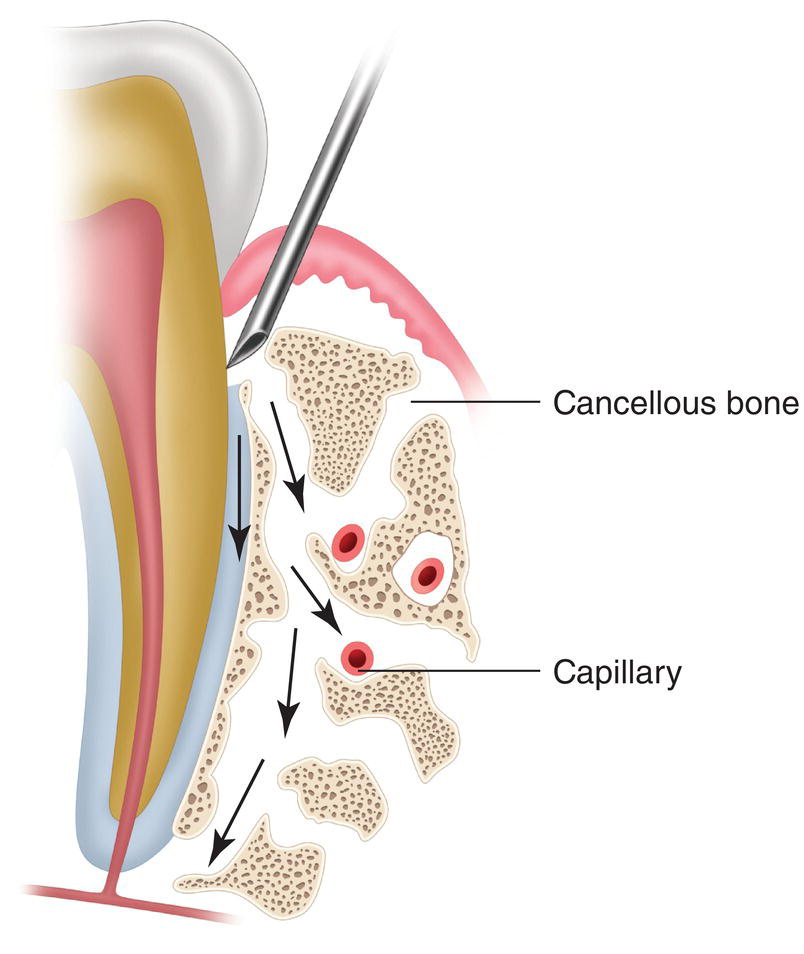
Figure 18.2 Diffusion of the anesthetic solution along the periodontal ligament and along the fenestrations of the alveolar bone wall and of the subperiosteal orifices.
- Along the outer surface of the alveolar bone, below the periosteum and crossing through the cortical cavities to the medullary cavities of the alveolar cancellous bone (Tagger et al. 1994a; Tagger et al. 1994b).
In both cases, the anesthetic penetrates the medullary cavities of the alveolar cancellous bone (Fuhs et al. 1983; Dreyer et al. 1983; Garfunkel et al. 1983; Smith and Walton 1983b; Tagger et al. 1994a, 1994b), thus infiltrating wide areas of the bone under pressure and moving toward the apex at some distance from the injection site (Garfunkel et al. 1983; Smith and Walton 1983b). Furthermore, as it reaches the vessels and capillaries of the medullary cavities, it is considered to be equivalent with an intravascular injection (Smith et al. 1983c; Rawson and Orr II 1985; Pashley 1986), although experiments in humans have found that, compared with intravascular injection, blood levels are 25–40% without a vasoconstrictor, 10–15% with epinephrine, and 10–50% with felypressin (Cannell et al. 1993). In summary, the PDL technique functions in much the same way as the intraosseous technique (Garfunkel et al. 1983; Smith and Walton 1983b; Smith et al. 1983c; Pashley 1986), but with lower levels of anesthetic.
Factors that Determine Efficacy
Major Factors
- The pressure exerted is essential for successful anesthesia. Resistance during injection is highly indicative of successful anesthesia (Walton and Abbott 1981; Smith and Smith 1983a) because the pressure is necessary for the anesthetic solution to be distributed along the periodontal ligament and bone marrow to reach the apex (Edwards and Head 1989).
Table 18.1 Percentage of success with intraligamentary (periodontal ligament technique) anesthesia achieved with high‐pressure syringes (pistol‐grip) or traditional cartridge syringes.
Success (proportion) Reference High‐pressure syringe Standard syringe Treatment Malamed (1982) 89% (54/61) 82% (32/39) Ob, En, Ex, C Smith and Walton (1983b) 65% (39/60) 62% (55/88) En D’Souza et al. (1987) 72% (13/18) 50% (12/24) Cold Proportion 75% 65% Ob, obturation; En, endodontics; Ex, extraction; C, cutting.
Cold, dry ice stimulation.
χ 2 = 3.9537 (P < 0.05).
- Use of pressure syringes (pistol‐type). This type of syringe is more successful than traditional cartridge‐type syringes (Table 18.1), thus reinforcing point 1 above. This point reinforces the first point, since pressure syringes are designed to exert more pressure during the injection (Pashley 1986; D’Souza et al. 1987; Walmsley et al. 1989), to the extent that it is almost double (Table 18.2).
- Use of local anesthetic solutions with epinephrine. The best results are observed with standard solutions of lidocaine 2% with epinephrine 1:100 000 (Malamed 1982; Johnson et al. 1985; Kim 1986; Schleder et al. 1988) and 1:80 000 (Gray and Rood 1987; Meechan 2002), and articaine 4% with epinephrine 1:100 000 (Berlin et al. 2005).
Lidocaine 2% with epinephrine 1:50 000 (high concentration of epinephrine) also yields favorable results, which are even better and last longer than pulpal anesthesia, although they also increase the risk of adverse effects (such as tachycardi, palpitations, or tremors) (Kaufman et al. 1984). This better result is due not only to the fact that the vasoconstrictor retains the anesthetic by preventing its absorption, but also to the fact that epinephrine partially reduces blood flow in the dental pulp, thus leading to a partial reduction in A delta nerve fiber impulses (Edwards and Head 1989).
Poorer results are observed with anesthetic solutions that do not contain epinephrine (Malamed 1982; Kaufman et al. 1984; Kim 1986; Gray and Rood 1987; Meechan 2002), have low doses of epinephrine (1:200 000), or contain weaker vasoconstrictors (norepinephrine, levonordefrin, felypressin) (Malamed 1982; Kaufman et al. 1984, 1994; Johnson et al. 1985).
Minor Factors
- Treatments where efficacy is evaluated.
- The best results are observed with extractions, obturations, and periodontal procedures (Malamed 1982; Faulkner 1983; Kaufman et al. 1983; Miller 1983; Grundy 1984; Gray and Rood 1987), undoubtedly because these procedures require less deep pulpal anesthesia (Handler and Albers 1987; Walton 1990).
Table 18.2 Maximum pressures achieved with standard high‐pressure syringes (pistol‐type) in the PDL and infiltrative techniques.
Factors evaluated Pressure PSI kg/cm2 Reference Maximum pressure achieved Anesthetic technique Type of syringe PDL Traditional 340 23.9 Pashley et al. (1981) Traditional 325 22.8 Walmsley et al. (1989) The Wand 232 16.0 Nusstein et al. (2005a) The Wand STAa 294 20.3 Hochman et al. (2006) High‐pressure 616 43.3 Walmsley et al. (1989) Infiltrative Traditional 153 10.8 Maita and Horiuchi (1984) The Wand STAa 11.5 0.8 Hochman et al. (2006) Palatal injection The Wand STAa 68 4.7 Hochman et al. (2006) Mandibular block The Wand STAa 5 0.35 Hochman et al. (2006) Cartridges: resistance to breakage Glass 1474 101.2 Meechan et al. (1990) Plastic 655 45.2 “ kg/cm2, kilograms per square centimeter; PDL, periodontal ligament; PSI, pounds per square inch.
1 kg/cm2 = 14.5 PSI; 1 PSI = 0.069 kg/cm2.
a The Wand STA injection 0.005 ml/second, mean pressure values.
- The poorest results are observed with endodontic procedures (Malamed 1982; Faulkner 1983; Kaufman et al. 1983; Miller 1983; Grundy 1984) and tooth cutting (Malamed 1982; Kaufman et al. 1983; Miller 1983) because these approaches require deep pulpal anesthesia.
- The best results are observed with extractions, obturations, and periodontal procedures (Malamed 1982; Faulkner 1983; Kaufman et al. 1983; Miller 1983; Grundy 1984; Gray and Rood 1987), undoubtedly because these procedures require less deep pulpal anesthesia (Handler and Albers 1987; Walton 1990).
- Teeth in which a PDL injection is made. Thus, the worst results are noted for the anterior teeth (incisors and canines) and the best results in the posterior teeth (molars and premolars) (Kaufman et al. 1983; White et al. 1988; Meechan 2002). These data are also shown in Table 18.3.
- The clinician’s experience with this technique also improves on the results of clinical trials (Grundy 1984).
Instrument Set
The PDL technique can be performed with the traditional instrument set or with a more specific set, which is worthy of analysis in terms of both syringes and needles.
Syringes
- Traditional syringe. This is the classic cartridge‐type metal syringe, although it has certain disadvantages with respect to the PDL technique: (i) it exerts half the pressure of a high‐pressure syringe (pistol‐type) (Table 18.2), therefore its anesthetic effect is reduced (Table 18.1) given that pressure is a key factor for the success of this technique; (ii) women tend to exert 30% less pressure than men with the traditional syringe (Walmsley et al. 1989); and (iii) if the cartridge breaks because of excess pressure, the syringe does not have the security foil that high‐pressure syringes have to prevent glass fragments from falling into the patient’s mouth (Malamed 1982; Miller 1983).
- Pen‐type high‐pressure syringe (Citoject®) (Figure 18.3). This type of high‐pressure syringe is easier to hide in the hand, with the result that it is less “threatening” for the patient (Primosch 1986), although it is less stable and requires considerable pressure with the fingers (Cowan 1986). Each trigger pull injects 0.06 ml. In terms of clinical efficacy, this syringe is 65% successful as a primary technique (Cowan 1986).
Table 18.3 Percentage of pulpal anesthesia, evaluated using an electrical pulp tester, after administration of the standard solution (L‐100) with the PDL technique and a high‐pressure pistol‐type syringe in the maxillary teeth (max) and mandibular teeth (mand).
Adjacent teeth Tooth Reference Sample size Pulpal anesthesia Duration (min) Mesial Distal Molars and premolars (M and PM) First M max White et al. (1988) 20 75% 7 45% 60% First M mand White et al. (1988) 38 79% 6 33% 62% Cohen et al. (1993)a 10 80% — — — First PM max White et al. (1988) 24 58% 4 17% 42% First PM mand Handler and Albers (1987) 7 57% 22 — — Moore et al. (1987) 19 79% 10 16% 63% Schleder et al. (1988) 75 87% 20 45% 78% White et al. (1988) 39 63% 8 21% 45% McLean et al. (1992) 24 38% 12 — — Meechan (2002) 16 79% 16 — — Second PM D’Souza et al. (1987)b 42 60% — — — Average 68.6% 11.7 30% 58% Rounded average 70% 10 Incisors and canines (LI, C) C max Johnson et al. (1985) 20 35% 10 — — LI max White et al. (1988) 23 39% 16 30% 26% Kaufman et al. (1994) 40 50% 5 — — Meechan (2002) 16 75% 16 — — LI mand White et al. (1988) 22 18% 7 9% 9% C max Johnson et al. (1985) 20 55% 17 — — Average 45.3% 11.8 20% 18% Rounded average 45% 10 The table also shows the extension to adjacent teeth both mesially and distally.
L‐100 is the standard solution of lidocaine 2% with epinephrine 1:100 000 (10 μg/ml).
a Cold stimulus with dichlorodifluoromethane in irreversible pulpitis, instead of an electric pulp tester.
b Cold stimulus with carbon dioxide, instead of an electric pulp tester.

Figure 18.3 High‐pressure pen‐type syringe (Citojet®).
- Pistol‐type high‐pressure syringe (Ligmaject® and Peripress® or similar syringes) (Figure 18.4).
This type of syringe first appeared in the 1970s. It has a pistol grip and a barrel with a lateral window that enables the clinician to see how much solution remains in the cartridge and any possible breakage in the cartridge (Primosch 1986). The syringe has a Mylar sheath that encases the cartridge in the barrel to prevent pieces of glass from entering the patient’s mouth in the case of breakage (Khedari 1982; Malamed 1982; Miller 1983; Saadoun and Malamed 1985; Primosch 1986). It is important to remember that with this technique the cartridge can break in 1.5% of cases (Primosch 1986). Each trigger pull injects 0.2 ml of the anesthetic solution (Council on Dental Materials, Instruments, and Equipment 1983).

Figure 18.4 High‐pressure pistol‐type syringe (Ligmaject® or Peripress®).
The pistol grip provides better control and stability, thus enabling the following: (i) application of considerable pressure (Chenaux et al. 1976; Khedari 1982; Pashley 1986; D’Souza et al. 1987), almost twice that of a traditional syringe (Table 18.2), and (ii) a measurable difference in applied pressures between male and female providers has not been detected (Walmsley et al. 1989). Therefore, as a primary technique, this type of syringe has a success rate of 75% (Table 18.1).
Needles
Traditional cartridge‐type syringes require 27G or 25G short needles (20–25 mm). Since 25G needles are more rigid, they are easier to manage (Walton and Abbott 1981; Malamed 1982; Walton 1990).
High‐pressure syringes require 30G or 27G extrashort needles (8–12 mm), and although the 30G needle is the most widely used, it is also the caliber that most frequently bends under the pressure applied during injection (Malamed 1982; Smith and Smith 1983a). Therefore, the extrashort 27G needle (8 mm) is preferable, since it bends less and is sufficiently fine to fit between the tooth and the alveolar crest.
Cartridges
Glass cartridges are preferred because they can bear twice as much pressure as plastic cartridges before breaking (Table 18.2). Plastic cartridges do not break, although they deform at half the pressure of a glass cartridge, thus enabling the anesthetic solution to leak out (Meechan et al. 1990).
Anesthetized Area
The area anesthetized with the PDL technique is well‐defined, as in all supplementary techniques.
- Tooth (pulp and periodontal ligament) on which the technique is performed, extending mesially – and more often distally – to the adjacent teeth.
- Vestibule and tongue area, both the fibromucosa (alveolar mucosa, gum, and interdental papillae) and the bone and periosteum of the anesthetized tooth. It is important to remember that this technique is applied in a very well‐defined area.
Technique
- If a dental dam is in place, then it must not be removed (Nusstein et al. 2003). This is an advantage.
- As a primary technique, this approach is considered painful (Annex 23), but it is not painful in practice because it is used as a supplementary technique when all other approaches have failed and therefore all the adjacent tissues, but not the dental pulp, are anesthetized.
- Given our previous comments, the most advisable approach would be to use a pistol‐type high‐pressure syringe with an extrashort 27G needle (8 mm) and a local anesthetic solution with epinephrine (if there are no contraindications), similar to the one being used in the area (remember not to mix two different anesthetic solutions at the same site). For example, if articaine 4% with epinephrine 1:100 000 (A‐100) is used in a buccal maxillary infiltration, then the same solution should be injected; if a mandibular block is performed with standard lidocaine 2% with epinephrine 1:100 000 (L‐100) and then reinforced with a buccal infiltration a of A‐100, then the procedure should be continued with A‐100 in the intraligamentary technique.
- Clean the gingival area of food particles, debris, plaque, or tartar beforehand (Chenaux et al. 1976; Brännström et al. 1982; Kaufman et al. 1983; Council on Dental Materials, Instruments, and Equipment 1983; Faulkner 1983) to prevent them from entering the tissues.
- Insert the needle into the gingival sulcus. This is the most important step, and often the most difficult (Council on Dental Materials, Instruments, and Equipment 1983).
- Insert the needle mesially into the mesial‐buccal and mesial‐lingual angles, distally into the distal‐vestibular and distal‐lingual angles (Figure 18.5).
- With an angle of approximately 30° with respect to the axis of the tooth to respect the convexity of the enamel of the neck of the tooth (Figure 18.6).
- The bevel should be facing outwards.
- The needle should be forced firmly between the alveolar crest and the cervical surface of the root of the tooth, pressing toward the apex.
- It is occasionally necessary to bend the stem of the needle to reach the most posterior teeth (Chenaux et al. 1976; Khedari 1982; Primosch 1986).
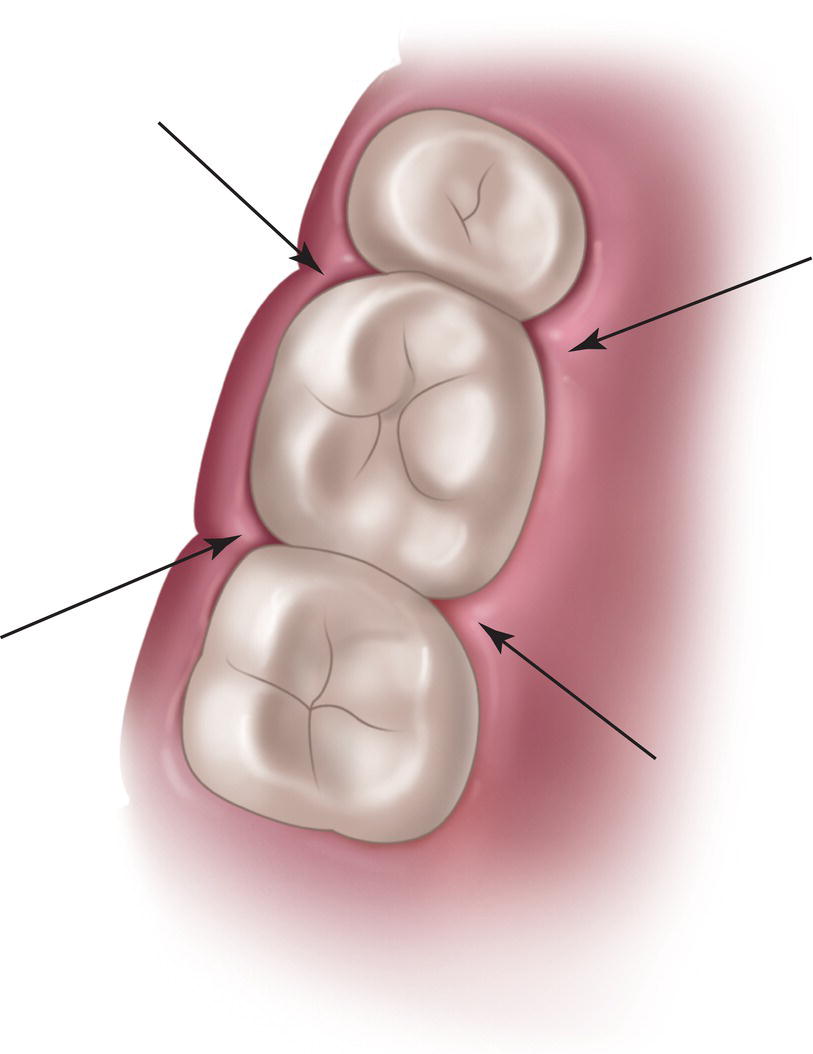
Figure 18.5 Mesio‐vestibular, mesio‐lingual, disto‐vestibular, and disto‐lingual angles where the needle is inserted.

Figure 18.6 30° angle with respect to the axis of the tooth for insertion of the needle. Note that the bevel is turned outwards.
- Aspiration is not necessary since the anesthetic solution, once injected, is thought to reach the systemic bloodstream quickly (Smith and Walton 1983b; Rawson and Orr II 1985). Some clinical trials report positive aspirations in 94% of cases (Medvedev et al. 2012).
- Inject under pressure.
- Pressure is very important for the success of the technique and is a sign that the needle has been inserted correctly (Walton and Abbott 1981; Smith and Smith 1983a). If the injection is made at several points in a tooth, then there should be resistance to the injection in at least one point. If there is no resistance, then the anesthetic solution has been distributed through the soft tissue but has not reached the apex.
- If there is no resistance, remove the needle and reposition it by reinserting it and forcing it toward the apex (Khedari 1982).
- Pressure should be maintained at each point for 10–20 seconds while injecting slowly (Meechan 1992) in order to:
- Prevent excess pressure from breaking the cartridge.
- Ensure that the anesthesia penetrates the tissue, preventing reflux of the anesthetic into the mouth. Despite these measures, some of the anesthetic often flows back into the patient’s mouth, and in 70% of cases he/she notices the bitter taste of the solution (Grundy 1984).
- The gum adjacent to the injection point turns white and pale owing to the ischemic effect of the pressure and the vasoconstrictor.
- Amount to be injected.
- Each trigger pull injects 0.2 ml (Chenaux et al. 1976; Council on Dental Materials, Instruments, and Equipment 1983). Thus:
- In monoradicular teeth, the solution is injected into one or two of the abovementioned sites mesially and/or distally (total 0.2–0.4 ml).
- In the case of multirooted teeth, the solution is injected at two or four sites mesially and distally (total 0.4–0.8 ml).
- These amounts are indeterminate since an unknown quantity of solution flows back into the patient’s mouth.
- Each trigger pull injects 0.2 ml (Chenaux et al. 1976; Council on Dental Materials, Instruments, and Equipment 1983). Thus:
- Onset of pulpal anesthesia is very fast (10–30 seconds) (Walton and Abbott 1981; Kaufman et al. 1983; Gray and Rood 1987; White et al. 1988; Childers et al. 1996). In 93% of cases where anesthesia is successful, the pulp is already anesthetized at 15 seconds (Walton and Abbott 1981). The anesthetic effect has a short duration, on average 10 minutes (Table 18.3) and generally less than 20 minutes (Childers et al. 1996).
- As the effect is very localized and there are scarcely any subjective symptoms (soft tissue anesthesia), the only guarantee of success is treatment. If the technique is used as a supplementary approach (the most common situation), the soft tissue anesthesia is from the techniques that have failed.
- As primary anesthesia (very uncommon), anesthesia of the soft tissues lasts 25–40 minutes (Johnson et al. 1985).
- If the approach fails, a new attempt can be made after 30–60 seconds (Cohen et al. 1993), thus improving the results (Table 18.4). There is generally no risk of toxicity, even though the technique is considered to inevitably result in intravascular administration, since the dose administered is small and the technique is only used in specific teeth when standard techniques have failed. Moreover, part of the injected solution flows back into the mouth.
Efficacy of This Technique
The efficacy of the technique is evaluated using an electric pulp tester, which tells us that the success rate is 70% in posterior teeth and 45% in anterior teeth, with a duration of around 10 minutes (Table 18.3). These data are for pistol‐type high‐pressure syringes and a single injection of standard solution (L‐100). Furthermore, we can observe that the neighboring teeth are also anesthetized, especially the distal teeth (Table 18.3). Evaluation of clinical success (more subjective and less rigorous method) reveals a success rate of 90%, although this can be with one or two injections (two if the first fails) (Tables 18.4 and 18.5).
Specific Complications of the Technique
Complications Due to Performance of the Technique
- 30G needles usually bend because they are not very rigid and it is necessary to apply a certain degree of pressure (Malamed 1982; Kaufman et al. 1983; Smith and Smith 1983a), therefore it is more appropriate to use extrashort 27G needles in high‐pressure syringes because these are more rigid and resistant. If the needle bends, it should be replaced.
Table 18.4 Percentage of successful clinical outcome after the first injection and after the first and second injections, both with pistol‐type syringes.
Success Reference Treatment First injection First and second injection Smith and Walton (1983b) En 65% 85% Gray and Rood (1987) Ob, Ex, En 71% 92% Cohen et al. (1993) En 80% 90% Cohen et al. (1993) En 70% 100% Average 72% 92% Rounded average 70% 90% Ob, obturation; En, endodontics; Ex, extraction.
Table 18.5 Percentage of clinical success with the periodontal ligament injection using a pistol‐type syringe and the standard injection solution (L‐100).
Reference Sample size Treatment Success Malamed (1982) 100 Ob, Ex, En, C 86% Faulkner (1983)a 200 Ob, Ex, En 86% Kaufman et al. (1983) 258 Ob, Ex, En 84% Miller (1983) 361 Ob, Ex, En, C 96% Smith and Smith (1983a) 60 En 85%
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


