23
General Complications of Dental Local Anesthesia
General or systemic complications are less common during dental treatment than local complications, and it is estimated that fewer than 1% of patients treated are affected (see Tables 23.1 and 23.2). General complications or systemic toxicity can result in serious harm or even death, but fortunately most cases are of little consequence. Approximately 75% of cases are caused or associated with dental local anesthesia (Table 23.3), and it has been observed that there are situations in which the frequency of general complications is increased, as follows:
- After multiple administrations of local anesthetic in the same patient (Persson 1969).
- Failure of local anesthetic (Persson 1969).
- Patients with a history of complications during administration of local anesthetic (Persson 1969).
- Patients at risk (ASA III) when treatment takes more than 30 minutes, especially patients with cardiovascular conditions (Hughes et al. 1966; Daubländer et al. 1997).
- Endodontic treatment and extractions increase the risk (Matsuura 1989; Malamed 1993).
Table 23.1 Vasovagal syncope as a percentage of general complications that appear during dental treatment.
| Reference | Origin | Complications observed | Years of study | Vasovagal syncope (%) |
|---|---|---|---|---|
| Fast et al. (1986) | United States | 16.773 | 10 | 67 |
| Matsuura 1989 | Japan | — | 5 | 63 |
| Malamed (1993) | United States | 13.835 | 10 | 30 |
| Girdler and Smith (1999) | UK | 814 | 1 | 73 |
| Mean | 58 ≈ 60 | |||
Table 23.2 Percentage of patients who experience vasovagal syncope in the office, excluding patients aged <14 years.
| Reference | Sample size | No. of cases of vasovagal syncope | Cases of vasovagal syncope (%) |
|---|---|---|---|
| First part, pre‐1980 | |||
| Moose (1959) | 1636 | 25 | 1.5 |
| Hannington‐Kiff (1969) | 3000 | 60 | 2 |
| McGimpsey (1977) | 9513 | 100 | 1.1 |
| Edmondson et al. (1978) | 6265 | 135 | 2.2 |
| Mean | 1.7 ≈ 1.5 | ||
| Second part, post‐1980 | |||
| Lemay et al. (1984) | 108 | 1 | 0.9 |
| Meechan and Blair (1989) | 440 | 1 | 0.2 |
| Hidding and Khoury (1991) | 1518 | 12 | 0.8 |
| Salins et al. (1992) | 1500 | 10 | 0.7 |
| D’Eramo (1992) | 199 045 | 278 | 0.4 |
| Daubländer et al. (1997) | 2731 | 12 | 0.4 |
| D’Eramo (1999) | 158 061 | 1114 | 0.7 |
| Lustig and Zusman (1999) | 1007 | 1 | 0.1 |
| Kaufman et al. (2000) | 179 | 1 | 0.6 |
| Moore et al. (2006) | 187 | 1 | 0.5 |
| Mean | 0.53 ≈ 0.5 | ||
Many patients in the first part (pre‐1980) were treated while seated in the chair, therefore we took the values in the second part because patients were lying back in the dentist’s chair (leading to fewer cases). The second part (post‐1980) is the current data.
Table 23.3 Percentage of general complications during dental treatment caused by or associated with dental local anesthesia.
| Percentage of complications during | |||
|---|---|---|---|
| Reference | Local anesthesia (%) | Dental treatment (%) | Total (%) |
| Hannington‐Kiff (1969) | 36 | 48 | 84 |
| Edmondson et al. (1978) | 45 | 22 | 67 |
| Matsuura 1989 | 55 | 23 | 78 |
| Malamed (1993) | 55 | 22 | 77 |
| Mean | 76.5 | ||
| Rounded mean | 75 | ||
The two main causes or triggers of complications associated with local anesthetic are as follows: (i) psychogenic reaction because of anxiety and needle phobia, and (ii) adverse reactions to the components of the local anesthetic solution.
Death is the most severe complication that can arise in the dentist’s office. Dental local anesthesia has proven to be very safe. Table 23.4 shows that when dental local anesthesia is administered with a minimum standard of recommended care, mortality is one case in 100 million injections, whereas with general anesthetic or deep sedation it is one case in 500 000, that is, a 200‐fold greater risk. Furthermore, death during general anesthesia is recorded mainly in healthy patients graded as ASA I or II, whereas cases of death as a result of dental local anesthesia usually involve patients graded as ASA III or IV (Driscoll 1974). Finally, general complications, especially those caused by local anesthesia in the dental clinical setting are as follows:
- Psychogenic reaction:
- Vasovagal syncope.
- Hyperventilation syndrome.
- Allergic‐like reactions.
- Toxicity induced by sympathomimetic vasoconstrictors (epinephrine and norepinephrine).
- Systemic toxicity induced by local anesthetics.
- Toxic methemoglobinemia caused by some local anesthetics.
- Allergic reactions to components of local anesthetic solutions.
Table 23.4 Frequency of death after dental local anesthesia and general anesthesia and deep sedation in dentistry.
| Reference | Origin | Study period | Deaths/patients | Frequency of death |
|---|---|---|---|---|
| Local anesthesia | ||||
| Selding and Recant (1955) | USA | 1943–1952 | 2/90 million | 1/45 million |
| Cawson et al. (1983) | UK | 1970–1979 | 10/700 million | 1/70 million |
| Matsuura 1989 | Japan | 1984–1985 | 9/300 milliona | 1/33 million |
| Perea et al. (2014) | Spain | 2000–2010 | 1/385 milliona | 1/385 million |
| Mean | 1/130 million | |||
| Rounded mean | 1/100 million a | |||
| General anesthesia and deep sedation | ||||
| Driscoll (1974) | USA | — | 11/5 285 750 | 1/480 000 |
| Tomlin (1974) | UK | 1963–1968 | 26/7 956 000 | 1/300 000 |
| Coplans and Curson (1982) | UK | 1970–1979 | 99/15 168 000 | 1/150 000 |
| Lytle and Stamper (1989) | USA | 1968–1988 | 7/4 700 000 | 1/670 000 |
| Nkansah et al. (1997) | Canada | 1990–1995 | 4/2 830 000 | 1/700 000 |
| D’Eramo (1992, 1999), D’Eramo et al. (2003) | USA | 1984–1999 | 8/5 377 000 | 1/670 000 |
| Mean | 1/495 000 | |||
| Rounded mean | 1/500 000 | |||
a The data for Japan are estimated based on double the population of the UK since Japan has twice as many inhabitants. The data for Spain are based on 35 million cartridges per year (Rosso 2015). The figures for Japan may be underestimated and those for Spain may be overestimated, therefore we established the figure of 1/100 million.
Preventive Measures
The main preventive measures we can take when administering local anesthetic in the office are as follows:
- A complete clinical history and health questionnaire to obtain information about the patient’s illnesses (e.g. diabetes, hypertension, history of myocardial infarction), current medications (e.g. beta‐blockers, digoxin, insulin, tricyclic antidepressants), or general reactions to previous local anesthetics that the patient has experienced and require anesthetic techniques or solutions to be modified or reactions that simply contraindicate local anesthetic (Chapters 8–10).
- Reassure the patient (Abasi 1987). The methods for administering local anesthetic are discussed in the chapter on basic injection techniques (Chapter 13). It is important to remember the repercussions of anxiety (Annex 17). Other techniques (e.g. pharmacologic therapy, hypnosis) in patients with considerable anxiety or medical problems are beyond the scope of this book.
- Prevent pain (Abasi 1987), both during administration of the local anesthesia and during the dental procedure (in cases where deep anesthesia is necessary). It is important to remember the repercussions of pain (Annex 17).
- Aspirate before the injection to prevent inadvertent intravascular injection of solution entering the bloodstream (Chapter 13). Although some authors have not found an association between positive and negative aspirations and systemic reactions (Forrest 1959; Goldman and Gray 1963; Persson et al. 1974; Blair and Meechan 1985; Lipp et al. 1988), possibly because toxic reactions to anesthetics are often confused with other types of reaction (e.g. vasovagal syncope), there is general consensus that aspirating reduces the risk of intravascular injection (Malamed 2004; Horowitz et al. 2005). Furthermore, aspiration is recommended at each stage to prevent intravascular injection (Lloyd 1992). It is important to remember that intravascular injection can sometimes increase toxicity by up to 200‐fold (Meechan and Rood 1992).
To ensure correct aspiration, it is very important to use 25G or 27G needles (25G is better) since they enable evaluation of the blood that colors the cartridge; this is not possible with 30G needles because the smaller lumen of the needle makes detection of aspiration unreliable and difficult, thus little blood enters the cartridge (see Chapter 11).
- The injection should be administered slowly. The currently recommended rate is 1.8 ml in 40–60 seconds (Chapter 13), which enables us to reduce the toxicity of the anesthetic solution since fast injections can lead to rapid increases in plasma levels, especially in the case of inadvertent intravascular injections (Adriani and Campbell 1956; Adriani et al. 1959; Campbell and Adriani 1958; Scott and Hirschman 1982). Slow injections enable the anesthetic solution to dilute in the bloodstream (Adriani and Campbell 1956; Campbell and Adriani 1958; Forrest 1959), in turn enabling the lungs to retain some of the drug and attenuate the toxic effect (Tucker and Mather 1979; Scott 1986). Some authors consider slow injections to be the most important factor for preventing adverse reactions in dental local anesthesia, even more than aspiration (Malamed 2004).
- Do not exceed the maximum dose for dental treatment. Remember the patient’s weight and height, especially in preschool children and children younger than 6–8 years (Annex 10) and in low‐weight adults with reduced body mass, who are very often elderly, to minimize the risk of overdose (Goodson and Moore 1983; Hersh et al. 1991; Virts 1999). It is also important to remember that topical anesthesia contributes to the dose administered and should be added to the total dose (Cannell 1996; Meechan 1998). It is very useful to keep the empty cartridges until the procedure has finished to know at all times the dose administered, especially in the case of repeated injections.
Basic Management of Complications
This book does not address the management of general complications in the office: the reader can consult the several excellent texts available (Bennett and Rosenberg 2002; Malamed 2007; Grimes 2013) and guidelines such as those of the European Resuscitation Council (Monsieurs et al. 2015; European Resuscitation Council 2020) and the American Heart Association (Panchal et al. 2020; Topjian et al. 2020). However, we do wish to provide accepted guidelines on how to manage general complications.
Initial Measures
The steps to be taken in the case of a general complication associated with local anesthesia are as follows:
- Suspend the dental treatment being administered to address the complication that has arisen.
- Patient position.
- If the patient is conscious and is having difficulty breathing and/or shows signs of chest discomfort or is anxious or nervous, the best approach is to allow him/her to find a position that is comfortable. This generally involves the patient sitting up.
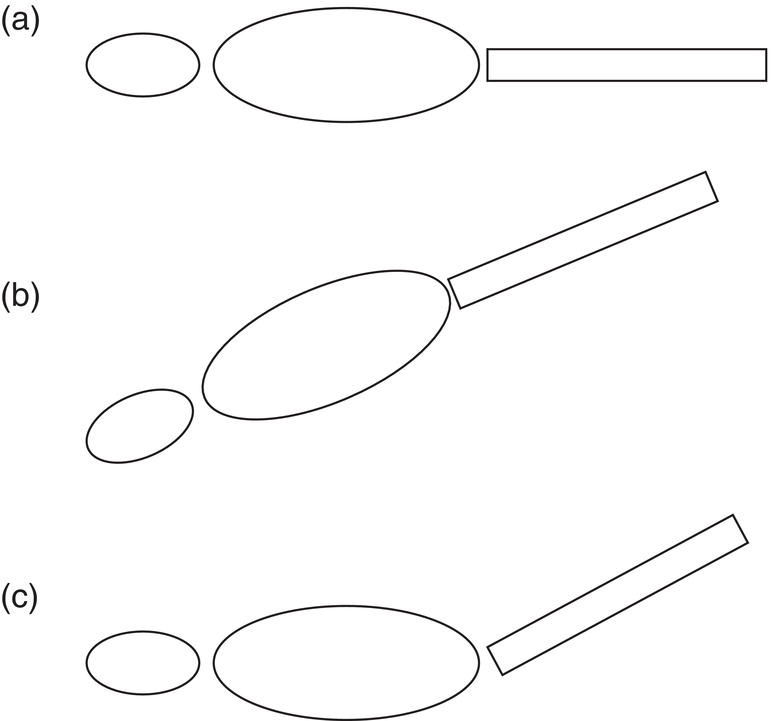
Figure 23.1 (a) Patient lying in the horizontal position (supine decubitus). (b) Patient in the Trendelenburg position. (c) Correct position, horizontal with the legs raised.
- If the patient becomes dizzy and it seems that he/she is going to lose consciousness, the best position is lying down (supine decubitus), with the head at the same height as the rest of the body and heart, to help blood reach the brain. In addition, the legs should be raised 15–30° to favor venous return of the peripheral blood to the heart (Figure 23.1c).
- Two important observations about posture:
- Do not place the patient in the Trendelenburg position, with the whole body in a straight line with the head pointing downwards (Figure 23.1b). In this posture, even though the head is lower than the heart, the abdominal organs exert pressure on the diaphragm, which in turn exerts pressure on the lungs, thus restricting respiration.
- Pregnant women in the third trimester should not be placed horizontally face up, since the gravid uterus exerts pressure on the inferior vena cava, which ascends pressing against the spinal column, leading to aortocaval compression syndrome. In these cases, the best approach is to place the patient in the left lateral recumbent position (McGimpsey 1977).
- If the patient is conscious and is having difficulty breathing and/or shows signs of chest discomfort or is anxious or nervous, the best approach is to allow him/her to find a position that is comfortable. This generally involves the patient sitting up.
- Loosen tight clothing such as belts, ties, and shirt collars so as not to interfere with blood flow (Edmonson et al. 1978; Kuster and Udin 1985).
Unconscious Patient
A loss of consciousness indicates a more dangerous phase, when we should adopt the PABC approach (Malamed 2007; Haas 2010) or the PCAB approach (Field et al. 2010).
P: Posture
The approach described is for a patient who reports dizziness, lightheadedness, or feeling faint, among other signs of impending unconsciousness, namely, lying down with the feet raised 15–30°. If the patient does not recover consciousness after a few seconds with this maneuver, then we should suspect a more severe underlying condition (i.e. arrhythmia, myocardial infarction, cerebrovascular accident, hypoglycemia) (Greenwood 2008; Sambrook et al. 2011).
A: Airway
- Remove any apparatus from the mouth, for example gauze, cotton rolls, removable dental prosthesis, removable orthodontics devices, rubber dam, clamps, etc.
- Clear the airway of obstruction by soft tissue, mainly a closed tongue, which falls backwards. Leave the patient’s head in a horizontal position by removing the extra head supports before performing the following maneuvers:
- Head tilt‐chin lift maneuver (standard maneuver) (Figure 23.2).
- The dentist places him/herself to the side of the patient’s head and, with the palm of the hand on the forehead, pulls downward. With the index and middle finger of the other hand placed on the symphysis menti, the dentist pulls upward until the imaginary line that joins the earlobe with the chin is perpendicular to the floor. Thus, the head is turned backward and the neck extended.
- During this maneuver, we should ensure that the patient’s mouth is not fully closed and that the full extension of the neck does not obstruct the airway.
- Jaw‐thrust technique (Figure 23.3). Sometimes, the previous technique may not be sufficient to clear the upper airway. The head tilt‐chin lift maneuver may not be applicable if the patient has a limited range of motion, such as one acquired by having a cervical spinal fusion or cervical disc herniation. The jaw‐thrust technique allows manipulation of the airway without movement of the head or cervical spine. The technique is as follows:
- The dentist places him/herself behind the patient’s head and places his/her index and middle fingers behind the posterior border of the mandibular ramus, with one hand on each side, and pulls the mandible upward.
- The lower lip can be pulled back with the thumbs to help the patient exhale through the mouth and nose.
- This maneuver is uncomfortable. However, any audible complaint from the patient is a positive sign because it shows that the degree of unconsciousness is not so deep.
- Head tilt‐chin lift maneuver (standard maneuver) (Figure 23.2).
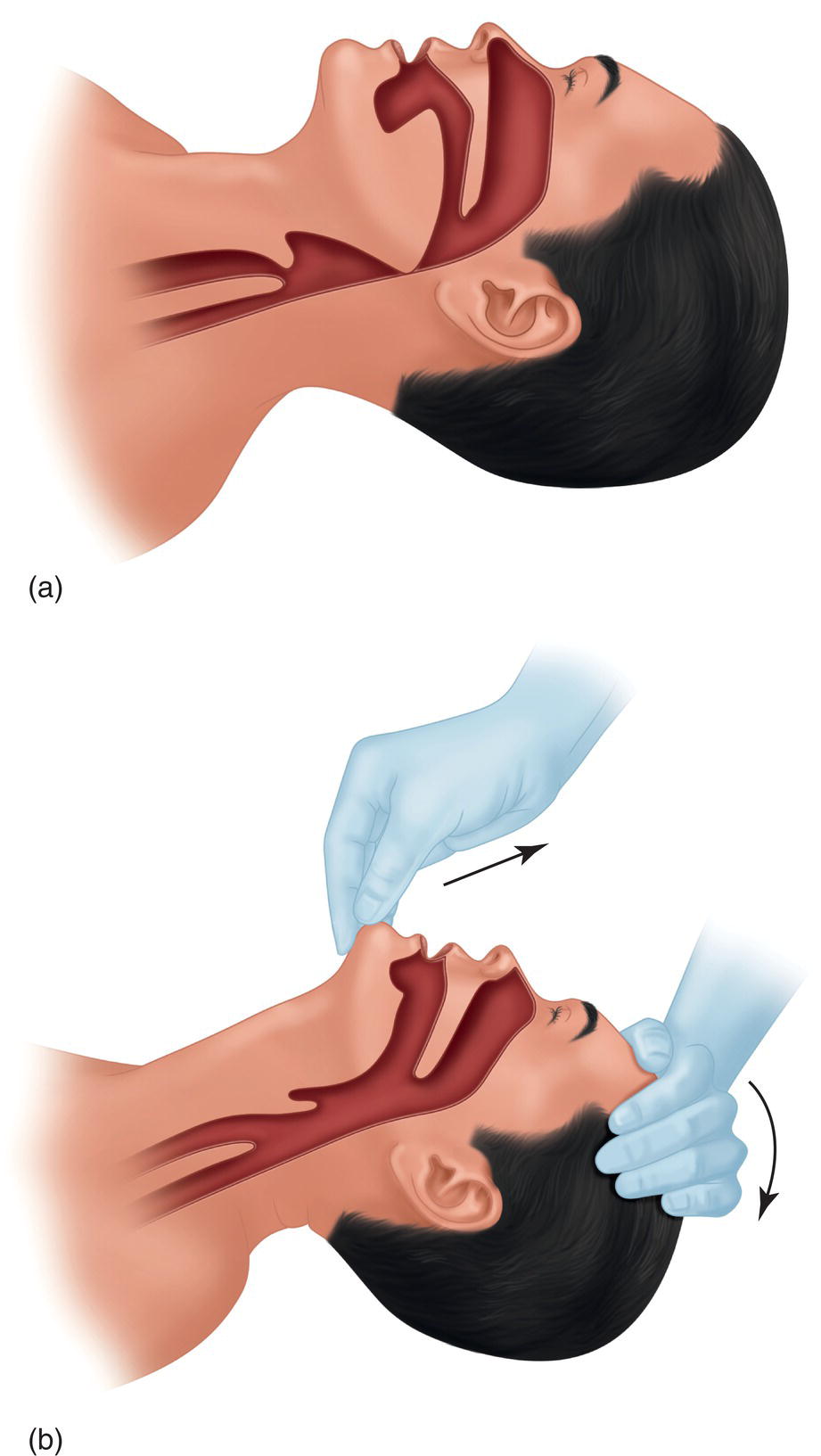
Figure 23.2 Head tilt‐chin lift maneuver, used to open the airways: (a) airway closed and (b) airway open.

Figure 23.3 Jaw‐thrust technique, used to open the airways.
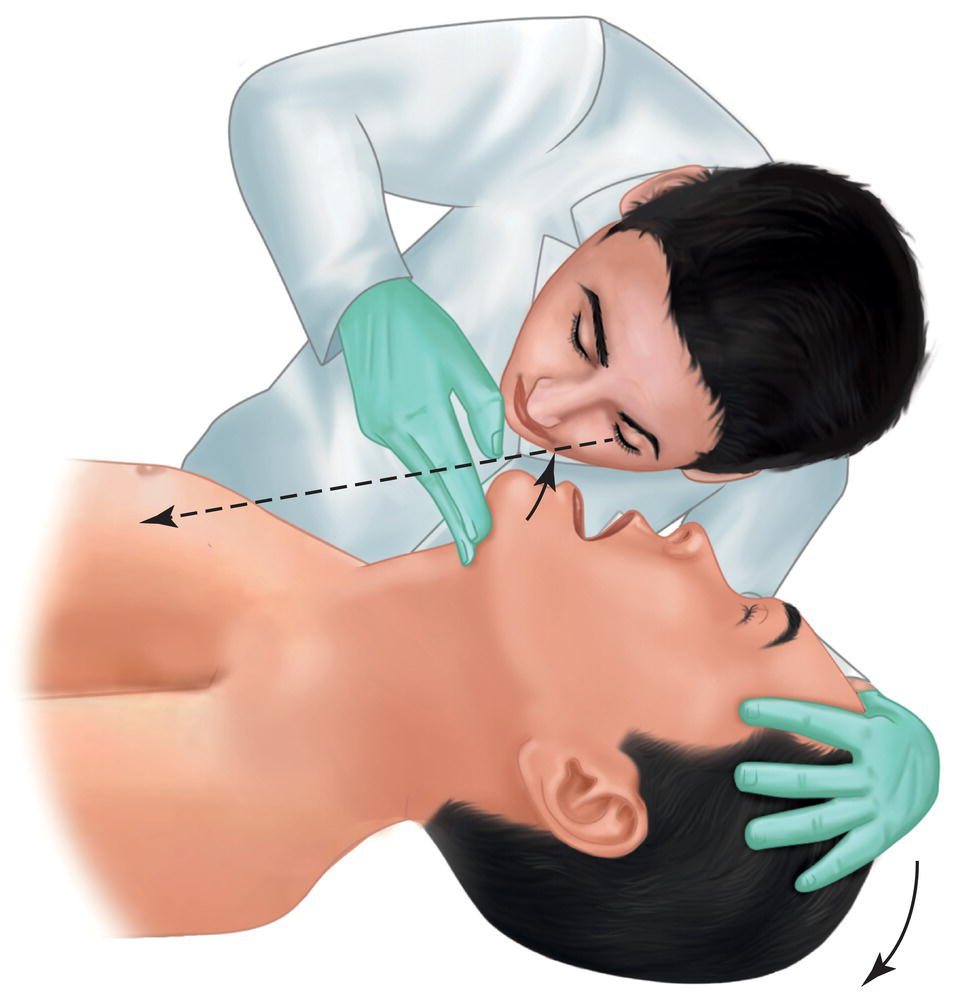
Figure 23.4 With the patient in the head tilt‐chin lift position, the dentist places his/her head with the ear approximately 2 cm from the patient’s nose and mouth, with the face looking toward the patient’s chest.
B: Breathing
- With the hands on the patient’s face to maintain the head tilt‐chin lift position, the dentist places his/her head with the ear approximately 2 cm from the patient’s nose and mouth and with the face looking toward the patient’s chest. This position enables the following (Figure 23.4):
- The dentist can hear and feel air entering and leaving the patient’s nose and mouth (very reliable).
- The dentist can see the movements of the patient’s chest. This is not as reliable since, while it shows that the patient is trying to breathe, it does not guarantee that gas exchange is taking place (as the diaphragm may be working against an obstructed upper airway). Sometimes, the patient’s clothing prevents the dentist from observing the movement of the chest.
- A bubbling/gurgling noise indicates that the airway is partially obstructed by blood, saliva, water, secretions, or vomit and should be cleared. The approach to adopt is as follows:
- The dentist positions the head downward and places the patient’s head turned to one side to facilitate expulsion and prevent the aspiration of liquids and debris.
- The dentist opens the patient’s mouth with the index and middle finger and inserts an aspirator to suck out liquids and debris. The cannula can even be inserted – carefully – in the posterior part of the mouth and lower pharynx to remove any remaining debris. The cannular should be plastic (not metal) so as not to further damage soft and hard tissue.
- If the patient is not breathing and there is no debris, the dentist should undertake artificial respiration maneuvers (not covered in this book). Please consult guidelines such as those of the European Resuscitation Council and the American Heart Association.
C: Circulation
At this point, the most important action is to palpate the carotid artery. With the patient in the low head tilt‐chin lift position, remove the hand from the chin and, as the patient has his/her neck stretched, palpate the thyroid cartilage (Adam’s apple). The carotid pulse is checked by placing the index and middle fingers between the thyroid cartilage and the sternocleidomastoid muscle.
If the pulse is weak but present, maintain the position until the patient recovers or until the emergency services arrive (see below) in the case of a patient whose condition remains unchanged or worsens.
If no pulse is felt for 10 seconds, start cardiopulmonary resuscitation. These maneuvers are beyond the scope of this book, although they are very well explained in other books and guidelines (Bennett and Rosenberg 2002; Malamed 2007; Monsieurs et al. 2015; Panchal et al. 2020; Topjian et al. 2020).
Note: The assistant can place a stethoscope on the patient’s chest to evaluate the heart rate and take the patient’s blood pressure with a sphygmomanometer. If the situation persists, the patient should be assessed every 5 minutes (heart rate, blood pressure, and breathing rate).
Routes of Administration of Drugs
Specific maneuvers may be necessary depending on the complication, and it may even be necessary to administer drugs. We can make a series of comments on the routes of administration:
- Intravenous route. While this route is the fastest, it also requires specific training. It is necessary to apply a tourniquet and to find the appropriate vein in the arm, hand, forearm, or antecubital fossa.
- Sublingual route (Mercurio 1967). The drug is injected into the floor of the mouth underneath the tongue if the injection is intraoral (Figure 23.5a); if the injection is extraoral, the submental technique is used (Figure 23.5b). This technique has somewhat slower onset than the intravenous technique, although it is faster than the intramuscular technique (Sklar and Schwartz 1965; Nichols and Cutright 1971). In some cases, it may be a good alternative to the intravenous technique for dentists who find it difficult to insert an intravenous line. One important caveat to this is that injecting into a highly vascular area, such as the floor of the mouth, can result in a hematoma that can worsen an already obstructed airway (Weaver 2011).
- Intramuscular route. This route is slower than the others. The drug can be injected into the deltoid muscle (shoulder), gluteus muscle (upper lateral quadrant so as not to inject the sciatic nerve or the vessels of the leg), or the vastus lateralis muscle of the leg (medial‐lateral area of the thigh), which is the preferred route in children. This route is one of the best for dentists.
- Subcutaneous route. This is the slowest route.
Parenteral injection techniques are addressed in various texts (Bennett and Rosenberg 2002; Malamed 2007).
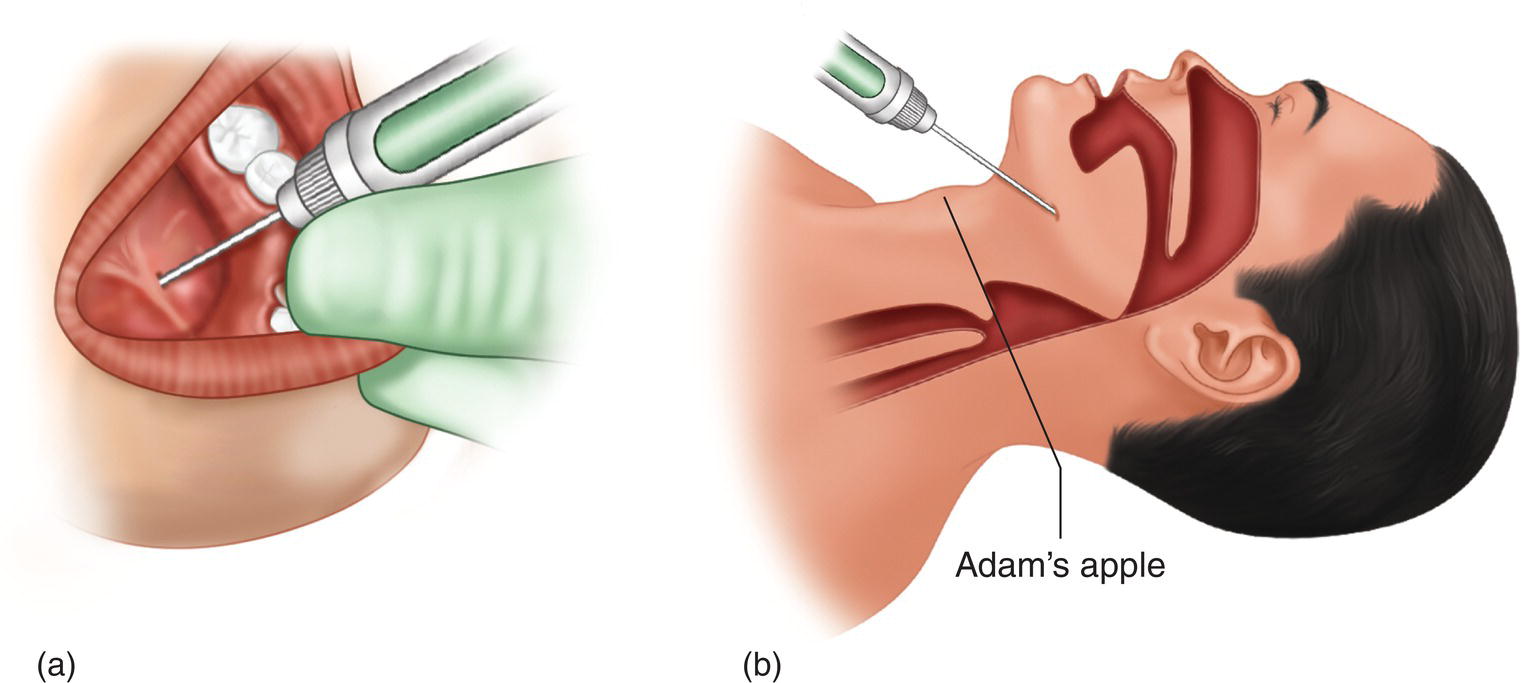
Figure 23.5 Sublingual injection techniques. (a) Injection into the floor of the mouth under the tongue if the drug is administered intraorally. (b) Submental approach if the drug is injected extraorally.
Calling the Emergency Services
If the dentist observes that (i) the patient does not improve and the situation does not resolve, (ii) the patient’s condition worsens, or (iii) his/her instinct indicates that the course of the complication is problematic, then the emergency services should be called so that the patient can be treated in situ by specialized staff with specialized equipment or taken to a hospital. The emergency telephone number is 911 in the United States, 112 in the European Union, and 999 in the UK.
Psychogenic Reactions
Psychogenic, or psychosomatic, reactions are the most frequent general complications and can be classified into three types:
- Vasovagal syncope: the most common.
- Hyperventilation syndrome.
- Allergic‐like reaction: this is exceptional.
General Causes
In all of the psychogenic reactions to be discussed, we can identify two key factors:
- The emotional situation of anxiety, tension, fear, or panic. This is the basic factor.
- The onset of intense and unexpected pain. This factor is closely associated with the first one because it triggers the emotional situation by creating a profound emotional experience of anxiety (McGimpsey 1977; Edmondson et al. 1978; Salins et al. 1992).
Anxiety is such an important factor that it is worth pointing out some associated characteristics:
- People who are naturally anxious. Approximately 10% of people have high levels of anxiety and fear when receiving dental treatment and a further 5% suffer from a phobia (Table 8.1, Chapter 8).
- Dental local anesthesia is the factor related to dental treatment that causes the highest levels of anxiety. Seeing the syringe and needle and feeling the prick of the needle generate the most anxiety (Chapter 8).
- It is difficult to differentiate between the behavior of anxious and non‐anxious adults in the office (McGimpsey 1977; Kleinknecht and Bernstein 1978; Ayer et al. 1983; Scott et al. 1984), therefore the health questionnaire should contain a direct question on fear of dental treatment, which could be classified into five categories (from none to considerable fear) to identify the most anxious patients and to consider the risk of general complications and the need for concomitant treatment to sedate the patient and control anxiety (Kleinknecht and Bernstein 1978; Scott and Hirschman 1982; Ayer et al. 1983).
It is interesting to highlight how nervousness before dental treatment can induce vasovagal syncope, even before the treatment is administered (D’Eramo 1999).
Vasovagal Syncope
Vasovagal syncope (neurocardiogenic syncope) is defined as a sudden and marked drop in blood pressure (hypotension) and heart rate (bradycardia) caused by anxiety, fear, and pain that is accompanied by weakness, sweating, and pallor. In its most severe form it involves a sudden, transitory loss of consciousness (syncope or faint) due to the drastic reduction in blood flow to the brain.
Vasovagal syncope is the most common complication during administration of dental anesthesia and dental treatment, accounting for 60% or more of all general complications (Table 23.1) and affecting 0.5% of patients treated (one in every 200) (Table 23.2). Other authors report a frequency of one case every 6 months (Girdler and Smith 1999).
It is important to draw attention to the fact that this type of reaction is easily confused with toxic reactions to local anesthetics or vasoconstrictors and with allergic reactions (Verrill 1975; McCarthy 1982; Milgrom and Fiset 1986; Daubländer et al. 1997; Batinac et al. 2013).
Pathophysiology
The severe emotional reaction induced by anxiety leads to three types of reaction:
- Severe hypotension. This is the main type of syncope. The emotional reaction and pain activate the parasympathetic nervous system in the brain (cholinergic), which acts via the vagus nerve (cranial nerve X), leading to the following:
- Dilation of the vessels of the abdominal viscera (splanchnic circulation) (Bourne 1980).
- Dilation of the vessels of the skeletal muscles in the absence of physical activity due to the lack of a fight or flight reaction (Harrison 1973; Edmondson et al. 1978; Bourne 1980).
- Reduction in heart rate (bradycardia).
These factors in turn lead to a severe reduction in blood pressure and therefore a reduction in blood flow to the brain. Curiously, the effect of this reaction can be triggered by stimulation of the autonomic nervous system (Taggart et al. 1976).
- Hyperventilation syndrome. This syndrome does not always accompany vasovagal syncope, although when it does, the level of carbon dioxide (CO2) falls, leading to a marked reduction in the concentration of this gas in blood (hypocapnia) and respiratory alkalosis caused by the increase in pH resulting from the reduction in carbonic acid. CO2 is a key factor in the self‐regulation of cerebral blood flow, which is independent of arterial pressure, therefore the reduction in CO2 causes cerebral vasoconstriction, reducing blood flow to this organ (Harrison 1973; Campbell et al. 1976; Noble 1977; Salins et al. 1992) and peripheral vasodilation (Noble 1977).
- Hypoglycemia. The parasympathetic reaction leads to increased insulin levels, which in turn reduces the blood glucose level (hypoglycemia). This also deteriorates because the hyperglycemic effect of epinephrine is reduced in situations of respiratory alkalosis due to hyperventilation, as reported elsewhere (Salins et al. 1992). Interestingly, blood sugar levels tend to self‐regulate after the vasovagal syncope (Salins et al. 1992).
Predisposing Factors
As we have seen, anxiety, fear, and pain are the main triggers of vasovagal syncope, although other factors can favor its appearance. Here, we classify them as more important and less important:
- More important, main factors (Table 23.5):
- Patient age. In general, patients aged under 30–35 years account for 80% of cases. However, in children aged <14 years, the frequency of this type of reaction is very low (one per 2000 = 0.05%) because children react to emotional tension differently than adults. They do not repress the fight or flight response, but rather scream, cry, and kick up a fuss. They resist the injection and therefore do not experience a vasovagal reaction (Kuster and Udin 1985). It is estimated that around one‐third of young adults are prone to this type of reaction (Yjipaavalniemi and Sane 1981).
- Male sex. This is the main factor in 75% of cases. It is important to remember that males account for 40% of visits (Annex 1). The reason is that society teaches males not to show emotions such as fear or pain, therefore they repress the fight or flight reaction, thus leaving themselves open to vasovagal syncope.
- Previous history. Patients with a history of fainting or syncope in other dental treatments or injections, blood donation, and vaccination. This is the case in almost half of all patients treated.
- Less important, additional factors (Table 23.5):
- Lack of sleep.
- Receiving dental treatment on an empty stomach.
- Excess heat and humidity.
Clinical Manifestations
Vasovagal syncope occurs in 75% of cases during administration of the local anesthetic or shortly after during dental treatment (Table 23.6) and can progress through several phases:
- Early phase, presyncope, or prodrome. This phase lasts several minutes and is characterized by the following:
- The patient is ill at ease, dizzy, and weak, with facial flushing.
- The first typical cutaneous signs appear, especially on the face, with pallor and cold sweat, sometimes accompanied by nausea (rarely vomiting) (McGimpsey 1977).
- Occasionally, palpitations resulting from the increase in heart rate, as well as respiratory abnormalities with more frequent, superficial, or deep breathing (hyperventilation).
Table 23.5 Factors predisposing to vasovagal syncope.
Factor Harrington‐Kiff (1969)
(%)McGimpsey (1977)
(%)Edmondson et al. (1978)
(%)Salins et al. (1992)
(%)Rounded average (%) Main factors Younger age 82 81 83 — 80 Male sex 76 81 70 — 75 Previous history 50 28 48 — 45 Additional factors Lack of sleep — — 0, 7 12 5 Empty stomach 28 80 8 19 35 Heat 24 — 23 — 25 Data expressed as percentages for main and additional factors.
Table 23.6 Time of onset of vasovagal syncope.
Reference Sample size During anesthesia (%) During extraction (%) Total: anesthesia and extraction (%) Hannington‐Kiff (1969) 50 — — 84 McGimpsey (1977) 100 31 47 78 Edmondson et al. (1978) 139 45 22 67 Mean 75 - Less frequently, ringing in the ears (tinnitus), blurred vision, and mouth opening, such as when yawning.
- Examination of cardiovascular parameters at the onset of this phase reveals increased blood pressure and heart rate due to anxiety (Campbell et al. 1976), although this all changes radically during the next phase.
- Late phase or syncope (faint). The main characteristic of this phase is loss of consciousness (syncope or fainting) due to severe hypotension and bradycardia. It is important to point out that this does not occur in all patients who experience vasovagal syncope: if the patient realizes what is happening and starts treatment during the first phase, it can be avoided relatively easily. In older studies on extractions, 30% of patients fainted (Hannington‐Kiff 1969; McGimpsey 1977), although today, and with the patient lying down, this percentage is much lower. Thus, we can observe the following:
- Loss of consciousness (fainting or syncope). If timely measures are taken, as we will see, the fainting episode lasts less than 1 minute and rarely more than 2 minutes (Hannington‐Kiff 1969; McGimpsey 1977).
- The faint may be accompanied by dilation of the pupils (mydriasis).
- Trembling or shaking is relatively common.
- The cardiovascular examination reveals the biphasic response. Low blood pressure, which may fall to lower than 50–60 mmHg (systolic) and at which point the patient faints (Harrison 1973; Campbell et al. 1976; Kuster and Udin 1985), and bradycardia (under 50–60 beats per minute).
- Recovery phase, which is characterized by recovery of consciousness, accompanied by confusion, disorientation, weakness, and, occasionally, headache.
Management by the Dentist
When the patient is conscious, it is essential to apply the initial measures we saw in the section on basic management of complications, as follows:
- Place the patient lying down (supine decubitus) with the head at the same height as the heart so that the blood can reach the brain and raise the legs 15–30° to facilitate venous return.
- Unfasten tight clothing, belts, ties, and shirt collars so as not to interfere with blood flow.
Note: Some professionals tend to place the patient in a seated position with the head between the legs at the level of the heart to help blood reach the head. This posture is not recommended because it prevents us from monitoring the patient’s breathing and consciousness and from raising the patient’s legs to favor venous return (McCarthy 1982).
Most patients recover with these measures and therefore do not reach the next phase:
- When the patient is already unconscious, we apply the basic PABC or PCAB management protocol. However, it is important to implement the following:
- Maintain the posture: patient lying down with the legs raised.
- Provide 100% oxygen through a mask (Hannington‐Kiff 1969; Verrill 1975; McCarthy 1982; Milan et al. 1986).
- Initiate support measures:
- Inhalation of ammonia salts arousal and consciousness (McCarthy 1982; Kuster and Udin 1985).
- Placement of cold towels on the patient’s head and forehead (McCarthy 1982; Kuster and Udin 1985).
- If the patient is cold, cover him/her with a blanket (McCarthy 1982; Kuster and Udin 1985).
- If possible, check blood glucose.
If the patient does not recover within 30–60 seconds of applying these measures, call the emergency services: the patient may have a more severe underlying problem (i.e. myocardial infarction, cardiac arrhythmia, cerebrovascular accident, hypoglycemia) (Greenwood 2008; Sambrook et al. 2011).
- When the patient has recovered:
- Do not allow him/her to stand up until total resolution of symptoms.
- Provide a sugary drink to raise the low sugar levels resulting from the vasovagal syncope (Edmondson et al. 1978; Salins et al. 1992). Hypoglycemia may also be a contributing factor to the syncopal episode, which often occurs as patients may skip a meal and come to the dental appointment.
- Decide whether the patient should continue with the treatment. We suggest the following:
- If the loss of consciousness lasts less than 10–15 seconds, the total recovery time takes less than 15 minutes, and the patient is less than 35 years old, treatment can be continued if the patient agrees.
- If the loss of consciousness lasts more than 1 minute, the total recovery time takes more than 30 minutes, and the patient is older than 40 years of age, suspend treatment, recommend the patient to see a doctor and not to drive, and ask a relative or friend to take the patient home.
- If in doubt, suspend treatment.
- Decide whether the patient should continue with the treatment. We suggest the following:
- When the patient is already unconscious, we apply the basic PABC or PCAB management protocol. However, it is important to implement the following:
Prevention
Although vasovagal syncope is easily controlled in healthy patients, in ASA III patients with cardiovascular abnormalities, who tolerate anxiety and pain poorly, the situation may become life‐threatening:
- Position during treatment
Ever since the contour dental chair was introduced in the 1960s, we have been working with the patient lying back, the dentist seated (Golden 1959; Anderson 1960), and a high aspiration rate (Thompson 1967). Not only does this form of working improve precision dental work, but with the patient lying back, cerebral blood flow is better. In addition, the risk of vasovagal syncope is higher with the patient seated and the dentist standing (Bourne 1957, 1970).
Table 23.4 shows that the frequency of vasovagal syncope in the pre‐1980, when patients were seated while the dentist stood, was higher than when dental work was carried out with the patient lying down and the dentist seated (1.5% vs. 0.5%).
- Control of anxiety
Patients with high levels of anxiety should be offered techniques to reduce anxiety and approaches that are beyond the scope of this book (conscious sedation, intravenous sedation). To determine the level of anxiety, we propose two key questions in the health questionnaire (Chapter 8):
- How frightened/anxious are you about dental treatment?
Not at all □ A little □ Some □ Quite a lot □ A lot □
If the patient selects the last two options (quite a lot or a lot), and especially the last, we should obtain more detailed information.
- Have you ever had an abnormal reaction, felt dizzy, or fainted at the dentist’s or doctor’s office when receiving a local anesthetic or vaccination or giving blood?
Yes □ No □
An answer in the affirmative should lead us to question the patient, given that a previous history is a major predisposing factor (see above) (Table 23.5).
- How frightened/anxious are you about dental treatment?
Hyperventilation Syndrome
Hyperventilation syndrome or reaction, which is also known as psychogenic dyspnea (Gardner 2000), was first described in 1937 (Kerr et al. 1937). Its definition should be refined since many of its components are confusing (Gardner 2000; Malmberg et al. 2001). Nevertheless, doctors frequently use it. The signs and symptoms of hyperventilation syndrome are often associated with vasovagal syncope, with some overlap between both conditions, although the vasovagal components are usually much more predominant than the respiratory components.
We can define hyperventilation syndrome as rapid and continuous respiration caused by anxiety that leads to a reduction in carbon dioxide (CO2) in blood (hypocapnia) and causes vasoconstriction of the cerebral vessels. This in turn leads to reduced blood flow in the central nervous system (CNS) and respiratory alkalosis, which decreases ionized calcium concentration and causes musculoskeletal reactions.
Hyperventilation syndrome is estimated to account for 8% of general complications (Matsuura 1989; Malamed 1993) and rarely appears in children for the same reasons as vasovagal reaction.
Pathophysiology
The main cause of the syndrome is the patient’s emotional status (anxiety, fear, hysteria, phobia), which increases the respiratory rate, thus reducing the level of carbon dioxide in blood and leading to hypocapnia, also known as hypocarbia. CO2 is a basic factor in the self‐regulation of cerebral blood flow that is independent of arterial blood pressure, with the result that the constriction of the cerebral vessels reduces the quantity of blood in the brain (Campbell et al. 1976; Noble 1977; Chapman 1984; Milan et al. 1986; Salins et al. 1992; Gardner 2000) and leads to peripheral vasodilation (Noble 1977).
The reduction in the pressure of CO2 in blood reduces carbonic acid levels, therefore blood pH increases (respiratory alkalosis) from 7.4 (normal) to 7.55, leading to two phenomena:
- The Bohr effect, which describes the effect of changes in blood pH on the avidity with which hemoglobin binds oxygen. In acidic conditions, the hemoglobin binds oxygen with less affinity and makes it more available to the tissues. In alkaline conditions, such as with hypocarbia, the hemoglobin binds oxygen with more affinity, thus making it more difficult to release and worsening oxygenation of the brain (Chapman 1984).
- Reduction in ionized calcium, leading to musculoskeletal irritation, which manifests as cramps, shaking, and tetany (muscle spasms) (Harrison 1973; Chapman 1984).
Anxiety also leads to increased activity of the sympathetic nervous system and release of epinephrine and norepinephrine, which in turn produces cardiovascular manifestations in the form of increased arterial pressure and heart rate (tachycardia) (Harrison 1973; Chapman 1984; Milan et al. 1986). Finally, a vicious cycle is created: anxiety leads to hyperventilation, which in turn increases anxiety (Compernolle et al. 1979).
Clinical Manifestations
Clinical manifestations can be classified as follows:
- Manifestations due to anxiety.
- 80% with dizziness, disorientation, weakness that rarely progresses to loss of consciousness (syncope/fainting) (Compernolle et al. 1979; Chapman 1984); in 60% accompanied by anxiety, nervousness, and agitation (Compernolle et al. 1979).
- 60% with palpitations owing to the increased heart rate (Compernolle et al. 1979).
- 60% with pallor and excessive sweating (diaphoresis) (Compernolle et al. 1979; Chapman 1984).
- Other manifestations are headache, blurred vision, ringing in the ears (tinnitus), nausea, and, more rarely, vomiting (Harrison 1973; Compernolle et al. 1979).
- During the examination, the state of agitation reveals an increase in heart rate (tachycardia) and arterial blood pressure.
- Sometimes the patient feels a sensation of chest tightness (distress) that may be made worse by breathing, although it is neither serious nor irradiated (Harrison 1973; Chapman 1984). The sensation is caused by irritation of the intercostal muscles and diaphragm due to increased respiratory effort (Chapman 1984).
- Respiratory manifestations.
- Increased respiratory rate (tachypnea) in 75% of cases, which reaches 25–30 breaths per minute instead of the normal rate (9–16). The breaths are deep or superficial. This is a basic sign (Harrison 1973; Noble 1977; Chapman 1984; Milan et al. 1986).
- Sensation of asphyxia and difficulty breathing (dyspnea), occasionally with a “lump in one’s throat” (globus sensation) in 50% of cases (Compernolle et al. 1979).
- Frequent movements to open the mouth and dry mouth sensation caused by anxiety and continuous breathing with the mouth open.
- Musculoskeletal manifestations (caused by reduced ionized calcium levels). Typical findings for this manifestation include the following:
- Feeling of numbness, tingling, and dullness (paresthesia) in the fingers and hands in 80% of cases, feet in 50% of cases, and face (tongue and lips) in 40% of cases, with muscle cramps and pain that can lead to muscle stiffness.
- Tetany (50% of cases), which is characterized by muscle spasms in the hands and feet (carpopedal spasm) involving the following:
- Stiffness of the hands (fingers and wrists) in flexion or extension, which is often painful (Geffner and Murgatroyd 1980).
- Feet (less common), with stiffness of the toes and ankles in flexion.
Differential Diagnosis
- Vasovagal syncope. Hyperventilation syndrome does not involve loss of consciousness or reduced heart rate/arterial blood pressure; in addition, it does not improve with the patient lying down.
- Asthma or allergic respiratory manifestations (Gardner 2000). Hyperventilation syndrome does not involve breath sounds (wheezing) because there is no constriction of the bronchioles. In addition, it improves with treatment.
- Heart attack (angina pectoris or myocardial infarction). The chest pain is not severe and does not irradiate to the arms or shoulders. Furthermore, it improves with treatment.
Management by the Dentist
We apply the basic measures (initial measures) seen above, although here we place emphasis on the patient’s position. As the patient experiences difficulty breathing, he/she should be seated, not lying horizontally (in contrast with the approach to a vasovagal syncope) (Harrison 1973; Chapman 1984). Furthermore, specific measures for these cases are presented in increasing order of importance, as follows:
- Explain to the patient what is happening to reassure him/her and ask him/her to breathe more slowly (six to eight breaths per minute) and thus reduce the respiratory rate (Harrison 1973; Chapman 1984). This measure is usually successful.
- Breathe into a paper or plastic bag. This approach should only be applied when the previous measure has failed. The patient is asked to place a paper bag over his/her nose and mouth and breathe into the bag (a plastic bag is also suitable, although as it is softer, it collapses easily over the nose and mouth). Thus, by breathing his/her own air, CO2 re‐enters the patient’s lungs and the signs and symptoms tend to improve (Harrison 1973; Compernolle et al. 1979; McCarthy 1982; Chapman 1984).
Today, paper bag rebreathing should never recommended unless myocardial ischemia can be ruled out and the patient’s oxygenation has been directly measured by arterial blood gases or pulse oximetry: since these conditions are impossible to achieve outside the hospital this method is not recommended (Callaham 1989).
- Medication. If the previous measure fails because the patient is very nervous, then this last alternative must be applied. This situation is very unusual because the previous measures are usually successful. In this case, intramuscular midazolam 5 ml (5 mg) is injected, and in 5–15 minutes the patient relaxes and recovers. Midazolam can also be given orally, although its effect takes more than 30 minutes.
A classic alternative is to inject diazepam (Valium®) 2 ml (10 mg) intramuscularly, although as it is not water‐soluble, this is more painful (Chapman 1984).
- Medication. If the previous measure fails because the patient is very nervous, then this last alternative must be applied. This situation is very unusual because the previous measures are usually successful. In this case, intramuscular midazolam 5 ml (5 mg) is injected, and in 5–15 minutes the patient relaxes and recovers. Midazolam can also be given orally, although its effect takes more than 30 minutes.
Patients who experience hyperventilation syndrome generally recover very well, do not lose consciousness, and can continue with their dental treatment.
Allergic‐like Reactions
These are also known as anaphylactoid reactions (Baldo et al. 2008) or allergic‐like reactions because they are nonimmune reactions caused by emotional tension that can lead to release of compounds such as histamine (Ring 1985) and reactions such as the following:
- Urticaria associated with anxiety (Milan et al. 1983; Tauberg et al. 1983).
- Angioedema associated with anxiety (Barclay and Edwards 1971; Chue 1976).
Note: The clinical description of these conditions is provided in this chapter (see below) in the section on allergy, where such conditions are typical.
Fortunately, this type of reaction is very rare and, logically, is confused with allergic reactions, since it is characterized by similar manifestations, but can be distinguished from allergic reactions by the negative result in allergy tests. Patients who experience reactions can be treated at the dentist’s office with anxiolytics and sedation (Milan et al. 1983; Tauberg et al. 1983).
Toxicity Induced by Sympathomimetic Vasoconstrictors
Approximately 3% of the general adverse reactions that occur during administration of local anesthetic are to epinephrine (Fast et al. 1986; Matsuura 1989). Interestingly, these reactions are usually confused with vasovagal syncope.
Pathophysiology
Initially, it was thought that the signs and symptoms were caused by the action of catecholamines (epinephrine and norepinephrine) in the brain. However, it has been shown that this is not the case because the low lipid solubility of these substances makes it difficult for the drugs to penetrate the CNS and intraventricular or intracisternal injections (direct administration to the brain) lead to sedation (Marley and Stephenson 1972).
The real cause of these actions is via the cardiovascular system, metabolic action, and neuromuscular transmission caused by these same adrenergic amines (Jastak et al. 1995). The reactions appear immediately as a result of an inadvertent intravascular injection, overdose, or severe interactions with other drugs (Pogrel et al. 2014). In any case, the effect is usually short, since catecholamines are inactivated after a few minutes (less than 5) (Lund 1951).
Symptoms of Reaction to Epinephrine
As we have seen, onset is rapid, occurring shortly after injection or even during injection. The reaction lasts only a few minutes and is characterized by the symptoms set out below (Dick 1953; Holroyd et al. 1960; Jastak et al. 1995; Malamed 2004):
- Patient‐reported symptoms:
- Sensation of anxiety, nervousness, fear, and apprehension.
- Palpitations (tachycardia) resulting from the force and speed at which the heart contracts. This is the main symptom.
- Dizziness, vertigo, and weakness.
- Occasionally, nausea, which rarely progresses to vomiting, difficulty breathing (dyspnea) caused by anxiety and, more rarely, headache, which is sometimes throbbing owing to the force with which the heart pumps blood, thus increasing pressure in the head.
- The signs are as follows:
- Pale and cold skin, mainly on the face, and sweating (diaphoresis).
- Occasionally, trembling in the lips and hands.
- The cardiovascular examination reveals increased heart rate, with frequent premature ventricular contraction, increased systolic arterial pressure and increased blood pressure.
Symptoms of Reaction to Norepinephrine
As seen above, onset of the reaction is rapid, shortly after the injection or even during the injection, generally at high concentrations, such as 1:25 000 (40 μg/ml) or 1:30 000 (33 μg/ml) (Boakes et al. 1972; New Zealand Committee on Adverse Drug Reactions 1974), and the reaction lasts a few minutes. The symptoms are set out below (Boakes et al. 1972; Meyer 1986; Van der Bijl and Victor 1992):
- Patient‐reported symptoms:
- Headache is the main symptom and the most frequent. Onset is immediate or within a few minutes. It is usually severe (often so intense that patients press their hands to their head). It generally affects the temporal or occipital area (nape of the neck), although there have been reports of frontal headache. The headache may be throbbing, although not always, and rarely may persist for hours or days, albeit with less intensity. This is due to involvement of the CNS.
- Other symptoms include anxiety, nervousness, apprehension, nausea (although rarely vomiting), and difficulty breathing (dyspnea) caused by anxiety.
- The signs are as follows:
- Pale and cold skin, mainly on the face, and sweating (diaphoresis).
- In contrast, the skin of the face is sometimes flushed.
- The cardiovascular examination reveals reduced heart rate (bradycardia), which is a very characteristic sign, and increased arterial pressure (both systolic and diastolic).
The general cause of reaction to norepinephrine is the encephalopathy caused by the hypertensive crisis.
Management by the Dentist
- The usual approach is as follows:
- Interrupt the dental procedure in progress.
- Wait and see if the reaction resolves itself, given that it is usually mild or moderate and disappears after a few minutes (less than 5), and continue with treatment.
- If the reaction does not resolve within a few minutes:
- Place the patient in a comfortable position, generally erect or seated/semiseated (never lying down). This position minimizes the effect of hypertension on brain tissue.
- Monitor the patient every 5 minutes, recording heart rate and blood pressure.
- If the situation persists:
- Administer oxygen through a mask. However, it is important not to confuse this situation with hyperventilation, in which case oxygen worsens the situation.
- Administer a sedative (diazepam or midazolam) parenterally (intramuscular); however, when these drugs take effect, the reaction has generally resolved.
- Wait until the patient has completely recovered, seated in the dental chair, from the fatigue resulting from the adrenergic excitation and only allow him/her to leave when fully recovered. When in doubt of any resolution of symptoms, activate emergency medical response services.
- Exceptionally, in predisposed patients, these situations (owing to the increased heart rate and/or increased blood pressure) can cause a heart attack (angina pectoris or myocardial infarction) or cerebrovascular accident. In these cases, and although beyond the scope of this book, the support measures set out at the beginning of this chapter should be followed and the emergency services called (911 in the United States, 112 in the European Union, and 999 in the UK).
Systemic Toxicity Induced by Local Anesthetics
Approximately 1.5% of all general complications occurring during administration of local anesthetics are caused by toxicity (Malamed 1993). It is important to remember that many such complications are mistaken for allergy and vasovagal syncope, when allergic reactions are usually very different from local anesthetic‐induced toxicity (see below).
Pathophysiology
Local anesthetics block sodium channels indiscriminately in excitable membranes (Covino 1987; Lai et al. 2004), the main targets being the nervous system and the muscles, especially the heart and cardiovascular system. In the case of toxicity, it is important to take into account the plasma level of the local anesthetic: venous concentrations are 20–50% lower than arterial levels (Eriksson et al. 1966; Moore et al. 1977; Knudsen et al. 1997), but physicians use the venous plasma values (expressed as micrograms per milliliter, μg/ml) (Annex 13).
Despite marked individual variability, toxic manifestations begin to appear when the local anesthetic exceeds a specific concentration (Annex 13). In addition, toxicity increases with the greater relative potency of the anesthetic and therefore is observed at lower plasma levels (Covino 1987; Garfield and Gugino 1987).
Local anesthetics first attack the CNS, which is more vulnerable, therefore lower plasma concentrations should be sought. Thus, as local anesthetic concentrations in blood increase, the drug can easily cross the blood–brain barrier owing to its high lipid solubility (Garfield and Gugino 1987) and low molecular weight (Covino 1987), affecting the CNS and leading to seizures. Subsequently, as plasma levels gradually increase, the cardiovascular system, which is more resistant, becomes involved, thus initiating the collapse that leads to death (Covino 1987; Garfield and Gugino 1987). The areas affected are as follows:
- CNS. In the delicate balance between inhibition and excitation, initial excitation is the predominant initial characteristic. The inhibitory neurons are blocked and the patient may have shaking, tremors, diplopia, tinnitus, and seizures. As toxicity advances, both inhibition and excitation are depressed, resulting in loss of consciousness (Garfield and Gugino 1987).
- Heart. Contractility is reduced, as is heart rate (bradycardia) (Covino 1987).
- Vessels. The direct action of the anesthetic leads to vasodilation as a result of relaxation of the vascular muscle tissue, and blood pressure falls (hypotension). In addition, as the sympathetic preganglionic nerve fibers are anesthetized, thus blocking the vasoconstrictor effect, both the vasodilator effect and hypotension become more pronounced.
During the convulsion phase, breathlessness is accompanied by a marked increase in oxygen consumption owing to the effort of muscular contractions. We therefore observe the following:
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


