Management of
Vertical Problems
(Open Bites and
Deep Bites)
This chapter discusses common vertical problems that initiate and develop during the primary or early mixed dentition: (1) open bites associated with persistent oral habits and other dysfunctions and (2) deep bites (dental deep bite and skeletal deep bite). These anomalies are not self-corrected and in some situations worsen in later stages of the dentition; therefore, early detection and intervention are important.
Open Bite
Treatment of skeletal open bite, or hyperdivergent phenotype malocclusion, and anterior open bite is one of the common difficulties facing orthodontists. They are especially problematic during the permanent dentition and are one of the most challenging malocclusions to treat.
The intent of this book is to emphasize the advantages of early-age intervention for all malocclusions, including open bites that initiate and develop during the primary and mixed dentitions. Open bite is a multifactorial phenomenon; recognition of the etiology plays an important role in diagnosis and treatment of this anomaly. The problem can be diagnosed clinically and cephalometrically; however, diagnosis should be viewed in the context of both skeletal and dental structures.
Hereditary factors influence the direction, form, and rate of skeletal growth; they can produce abnormal growth patterns and incorrect jaw posture, resulting in skeletal open bite. Environmental factors during the primary and mixed dentitions can also play an important role in developing open bites. Therefore, different kinds of open bite with different morphologic and etiologic characteristics must be accurately classified for precise treatment planning. This requires experience and training.
Early recognition of the cause and proper intervention can prevent the development of abnormalities or at least reduce the severity of the problem later. At the present time, it is not possible to eliminate or prevent the influence of genetic factors on dentoskeletal structure; however, with accurate examination and recognition of the effect, practitioners might be able to prevent, modify, or at least reduce the severity of the problem. Because environmental factors are mostly recognizable, recognition of and intervention in such influences at an early stage of formation can prevent development of open bite or at least guide the abnormality toward normality. The following are the major common local or environmental factors that play a role in development of open bite at early age:
• Digit sucking
• Abnormal tongue size, posture, and function
• Abnormal neuromuscular function
• Enlarged lymphatic tissue causing mouth breathing and postural alteration that induces dental and skeletal modifications
The etiology and mechanism of the factors causing open bite are discussed in detail in chapter 6. The current chapter presents the differential diagnosis, treatment strategies, and techniques for early correction of open bite during the primary and mixed dentitions.
Pediatric dentists and general practitioners who see children at an early age have greater responsibility for the detection of and intervention in these developing anomalies. Differential diagnosis and treatment of open bite malocclusion are sometimes challenging. However, successful identification of the etiology through careful clinical and cephalometric evaluation as well as some general history of the problem, improve the chances of treatment success. A brief review of the problem and its etiologic factors will be provided here, for the purpose of recognition and proper intervention.
Depending on the etiologic factors and the complexity of the abnormality, treatment for open bite ranges from observation to simple habit control to complex surgical procedures.
Etiology
Components of vertical problems must be diagnosed and classified under two contexts: skeletal structures and dental structures. Skeletal open bite usually has a genetic background and interacts with environmental causes. It can develop to a more complex dentoskeletal open bite and in some cases, especially if not resolved by the end of the mixed dentition years, will require complicated orthodontic and orthopedic treatment, with or without surgical intervention.
The first step toward early treatment is recognition of the problem, and the best way to recognize the problem is to understand and differentiate between the characteristics of different types of open bite. No single factor can be considered the cause of open bite. The most common local causes of this anomaly are thumb and finger sucking, tongue problems (such as abnormal function, size, position, and posture), mouth breathing as a result of enlarged lymphatic tissue or other airway obstruction, and lip dysfunction.
Finger sucking
Depending on the type of sucking and the position of the fingers, sucking can affect the occlusion by different mechanisms. Finger force directed to the anterior teeth and the incisive bone can cause dental and dentoalveolar protrusion and open bite, prevent eruption of anterior teeth, and lead to underdevelopment of the alveolar process; it can also cause posterior crossbite. A prolonged habit and absence of contact in the posterior teeth can also cause overeruption of the posterior teeth and even clockwise rotation of the mandible (Fig 13-1).

Fig 13-1 Dentoskeletal open bite and posterior crossbite caused by thumb sucking.
Abnormal tongue force
The tongue can cause anterior open bite through different mechanisms, such as tongue size, tongue position, tongue posture, and abnormal tongue function. Depending on the size of the tongue, macroglossia can have different destructive effects on the occlusion, such as interdental spacing, Class III malocclusion, and open bite. Severe enlargement of the tongue can also cause functional difficulties in speaking, eating, swallowing, and sleeping. This condition can be seen in individuals with certain inherited or congenital disorders, such as neonatal hypothyroidism, Down syndrome, and acromegaly.
Abnormal position of the tongue is another condition that can cause dentoskeletal deformity. This situation is not the result of the size of the tongue; rather the tongue is positioned more anteriorly as a subconscious reaction to large tonsils or because of mouth breathing in response to nasal obstruction or enlarged adenoid tissue (Fig 13-2).

Fig 13-2 (a to c) Dentoskeletal open bite caused by abnormal size, position, or function of the tongue.
Oral respiration
During mouth breathing, no matter what the cause, the mouth is open, the mandible is postured inferiorly, and the tongue is protruded between the anterior teeth and resting against the oral floor. This situation causes postural alteration and induces dental and skeletal modifications similar to those caused by thumb sucking.
Mouth breathing can also cause excessive eruption of the posterior teeth and maxillary constriction, change head posture, cause an increase in the vertical dimension of the face, and result in development of anterior dentoskeletal open bite.
Genetic factors
Genetic factors, either alone or in combination with local factors, can disrupt the normal skeletal growth pattern through different mechanisms, such as disturbance of the normal size, shape, and proportion of different parts of skeletal structures. Development of skeletal abnormalities causes several skeletal malocclusions, including open bite, which mostly require orthosurgical management.1
Tongue thrust is an abnormal tongue function that usually develops secondary to thumb sucking and then maintains or increases the open bite that was produced by the finger, even after the finger-sucking habit has stopped. During correction of open bite and application of different treatment mechanics, abnormal tongue function must be controlled.
Morphologic characteristics
For practical purposes and simplification of differential diagnosis, the open bite syndrome can be classified into two types: dental open bite and skeletal open bite.
Dental open bite
Simple dental open bite is considered an open bite without skeletal abnormalities, with the following characteristics:
• Normal craniofacial pattern
• Normal skeletal jaw relationships
• Previous history of finger sucking
• Proclined incisors
• Anterior tongue thrust
• Undererupted incisors
• Normal or slightly excessive molar height
• Normal inclination of posterior dentition
• Divergent occlusal plane
• No gummy smile
• No vertical excess or posterior tipping of the maxilla
Prolonged continuation of environmental factors and failure to initiate early treatment of simple dental open bite can produce more complicated effects, such as molar overeruption, mandibular clockwise rotation, and subsequently skeletal defects.
Skeletal open bite
True skeletal open bite abnormalities are usually caused by genetics, prolonged environmental factors, or a combination of both. They consist of many unfavorable growth patterns and skeletal disharmonies that must be distinguished by careful clinical and cephalometric evaluation before treatment planning.
The following are the important structural defects that can be detected by careful clinical and paraclinical evaluation of patients with skeletal open bite or vertical divergent face:
• Steep mandibular plane
• Retrognathic mandible
• Obtuse gonial angle
• Short ramal height
• Short anterior cranial base
• Short posterior cranial base
• Obtuse y-axis angle
• Obtuse saddle angle
• Obtuse articular angle
• Obtuse occlusal plane–mandibular plane angle
• Obtuse mandibular plane to palatal plane angle
• Counterclockwise rotation of the palate
• Increased lower facial height
• Decreased upper facial height
• Decreased posterior facial height
• Steep anterior cranial base
Differential diagnosis
Simple dental open bite is a common abnormality that occurs during the primary or early mixed dentition, caused by environmental problems such as abnormal habits, the type of nutrition, or enlargement of lymphatic tissues. Untreated open bite not only increases in severity over time but also can cause other dentoskeletal damage that can be more complicated to manage at a later age. These consequences are not confined to undereruption of anterior teeth; open bite can cause overeruption of the maxillary or mandibular molars or both, and in severe cases it can cause skeletal deformities such as clockwise rotation of the mandible or counterclockwise rotation of the maxilla.
For early intervention in simple anterior dental open bite, the first step before mechanotherapy is recognition of the type of open bite and the structure involved. Therefore, besides the clinical and paraclinical evaluations that always must be performed for assessment of all malocclusions, special attention to cephalometric analysis of the vertical dimension is important in diagnosis of open bite malocclusions. For differentiation of dental open bite and to verify whether the open bite is due to anterior undereruption or posterior overeruption, the author recommends a simple cephalometric evaluation of the occlusal plane relative to mandibular plane–palatal plane angle. In normal occlusion, the mandibular plane–palatal plane angle is about 30 degrees, and the occlusal plane bisects this angle almost equally. In patients with open bite, variations in this configuration indicate the cause of the open bite (Fig 13-3).
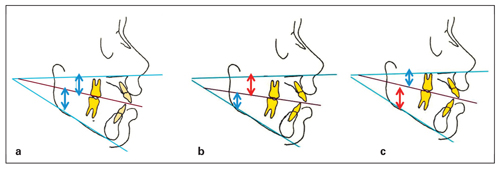
Fig 13-3 Cephalometric evaluation of mandibular plane– palatal plane angle to determine the cause of open bite. In normal occlusion, this measurement is about 30 degrees, and the occlusal plane bisects this angle almost equally. (a) Normal molar position with undereruption of the incisors. (b) Overeruption of the maxillary molars. (c) Overeruption of the mandibular molars.
Treatment strategies during the permanent dentition
As already discussed, early detection and interception of the developing anomaly at its early stage of development (primary or mixed dentition) is easier and provides more stable results. However, for the purposes of comparison, the following is a brief review of open bite correction in adolescents and adults.
Sustained open bite malocclusion during the late mixed dentition or permanent dentition is not self-correcting, and orthodontic treatment is almost always challenging; this is one of the most difficult malocclusions to treat orthodontically. Treatment approaches in this period depend on the age of the patient and the severity of the problem.
Habit control and lip seal
Habit control, lip seal, and swallowing exercises can have a positive effect in camouflage treatment, even during the permanent dentition. These methods facilitate orthodontic tooth movement against the tongue force, which can be achieved by a device such as a tongue guard.
Control of vertical growth
Control of vertical dental eruption and posterior dentoalveolar development during camouflage treatment can also be helpful in correction of the permanent dentition. This is achieved by use of a lower holding arch and a transpalatal arch.
Orthodontic camouflage
Orthodontic camouflage consists of only orthodontic procedures, with special tactics depending on the morphologic and anatomical structures involved in this malocclusion. These approaches include posterior intrusion, anterior extrusion, or a combination of both. This type of treatment can be combined with tooth extraction if appropriate.
Many appliances for correction of anterior open bite in the permanent dentition have been proposed, including a bite block; an extrusion or intrusion arch; a multiloop edgewise archwire2; functional appliances3; and extraoral forces such as high-pull headgear, vertical chin cup (which can have some positive effect in the early permanent dentition), titanium screw anchorage,4 titanium miniplates fixed bilaterally to the zygomatic buttress area,5 and a magnetic active vertical corrector device.6
Orthognathic surgery
True skeletal open bites cannot be treated by orthodontic camouflage alone and require a combination of orthodontics and surgical treatment,1 such as surgical impaction of the maxillary posterior segment, which is considered to be the most effective treatment option for correction of skeletal open bites in adult patients.
Early Treatment Strategies for Open Bite
Vertical growth of the face, as shown by Enlow,7 is the last dimension of the dentofacial structure to be completed during early postnatal growth and the transitional dentition. As Carlson8 pointed out, only 50% of growth in the midface and the mandible is complete by the age of 8 to 10 years. Therefore, early treatment and control of vertical growth during this period is more efficient.
Harris and Johnson,9 in a longitudinal sibling analysis, concluded that most occlusal variability is acquired, not inherited.
As mentioned earlier, the most common local causes of anterior open bites are thumb and finger sucking, mouth breathing in response to enlarged lymphatic tissue or other airway obstruction, lip dysfunction, and tongue problems (such as abnormal function, size, position, and posture). Anterior open bites caused by local factors are often accompanied by a downward rotation of the mandible, excessive eruption of the posterior teeth, or undereruption of the anterior teeth. The main strategy of early intervention is to overcome these abnormalities by eliminating or preventing the cause, as well as to correct or guide the affected sites, through the following tactics:
• Elimination or control of the etiologic factors that are disturbing incisor eruption and alveolar growth (such as finger sucking, tongue thrust, and lip dysfunction)
• Prevention or correction of maxillary and mandibular molar overeruption
• Prevention, control, or guidance of clockwise rotation of the mandible
• Incisor retraction to “close the drawbridge” between separated maxillary and mandibular incisors
• Achievement of an increase in the posterior facial height–anterior facial height ratio
Different fixed and removable appliances have been used to prevent and control the force of finger sucking and abnormal tongue thrusting in children (see chapter 6). The purpose of this discussion is to clarify the mechanotherapy and tactics that can be efficient in early treatment of anterior open bite.
Thumb or finger sucking is perhaps the most common type of non-nutritive oral habit present in children. Depending on the severity of the problem and type of finger sucking, this habit can cause severe dentoskeletal defects, including open bite (ranging from a simple dental open bite to a severe skeletal open bite), posterior crossbite, overeruption of molars, and mandibular rotation. Thus, treatment would be more efficient if started at an earlier age.
Placement of the tongue between the incisors has been sought as a causative factor for anterior open bite for some years. Subtelny10 stated that abnormal tongue function between incisors is a type of adaptation of the tongue to the open bite area formed by previous finger sucking. Proffit11 showed that individuals who place the tongue tip forward when they swallow usually do not have more tongue force against the teeth than do those who keep the tongue tip back; in fact, tongue pressure may be lower.
Swallowing is not a learned behavior. Forward tongue placement is a physiologic, subconscious function to fill the gap present between incisors during swallowing. The lips are brought together, and the tongue is placed between the separated anterior teeth to form an anterior seal to prevent food or liquids from escaping. Correction of anterior open bite is more complicated and disturbing when persistent tongue activity is present. Resolving the problem is easier if it is corrected at an earlier age; correction of open bite with persistent tongue thrust is much more difficult in the permanent dentition.
Depending on the etiologic factors and the complexity of the abnormality, early orthodontic treatment for open bite ranges from observation to simple habit control to complex surgical procedures.
Classification of open bite
To simplify the treatment planning process for anterior open bite correction during the primary or early mixed dentition, the author classifies open bite into three types of abnormality: type I, type II, and type III.
Type I simple dental open bite
Simple dental open bite is an anterior open bite in which some environmental factor has affected anterior tooth eruption and/or vertical growth of the alveolar process; as a result, a gap has developed between the anterior teeth. The size of the gap depends on the severity of the cause. In response to the open bite, abnormal tongue function has developed subconsciously to close the gap during swallowing, and therefore continuous tongue force maintains or worsens the gap. In type I open bite, no skeletal discrepancy or molar overeruption is involved; only the incisors or the dentoalveolar process is underdeveloped.
Type II combined dental open bite
In type II anterior open bite, an abnormality was initially caused by some environmental factor plus some minor skeletal disharmony or molar overeruption. In these situations, sustained local factors or hereditary background can cause further deformity to the dentition or basal bone, such as molar overeruption or slight mandibular rotation; therefore, signs of vertical problems are also present.
Type III dentoskeletal open bite
Type III open bite is an anterior open bite in which hereditary or congenital defects with or without local factors have changed the growth pattern of the child and therefore have changed the morphology and foundation of the dentoskeletal occlusion. This type of open bite is usually combined with some type of divergence of dentoskeletal structures and can be clearly recognized by cephalometric evaluation. Early detection and proper intervention can solve the problem or at least reduce the severity of the anomaly. Treatment during the permanent dentition is much more complicated and occasionally requires orthognathic surgery.
Treatment considerations
Early intervention in open bite differs depending on the stage of dentition and the type of open bite. Early treatment strategy for open bite malocclusion can be divided into three periods of dental development: primary dentition, mixed dentition, and permanent dentition. The tactics for treatment of the permanent dentition were discussed briefly earlier in the chapter. The following sections focus on early orthodontic intervention during the primary and mixed dentition periods.
Management during the primary dentition
Generally, active orthodontic treatment of open bite during the primary dentition is not recommended, because most cases at this stage of the dentition involve local factors such as pacifier or finger sucking or mouth breathing, which can be self-corrected after etiologic factors are eliminated. However, periodic observation by the dentist or the awareness of the parents can be helpful.
If abnormal habits are persistent and severe enough to affect normal jaw growth, for example by preventing anterior dentoalveolar growth or causing mandibular rotation, the patient and the parents should be advised that these severe habits can be controlled with a simple appliance such as a fixed tongue guard.
Management during the mixed dentition
After careful clinical and paraclinical evaluations of the problem are completed, treatment during the mixed dentition stage can be designed in one or two phases with or without orthognathic surgery. The pretreatment assessments should carefully verify the following:
• Type of open bite (skeletal, dental, or combination)
• Etiologic factors (whether the cause is still active)
• Morphology of the malocclusion and affected structures
• Skeletal age of the patient
• Cooperation of the patient and parents
The best age for early intervention is during the early mixed dentition.
Tactics of Early Intervention During the Mixed Dentition
The main strategy of early intervention is to eliminate or prevent the cause of the abnormality behind the open bite by controlling or guiding the affected sites.
Depending on the stage of the dentition, etiologic factors, characteristics, and the morphology of the open bite, the following six tactics may be applied.
1. Habit control
Control of finger or tongue force as an early intervention is the first and most important tactic in treatment of this anomaly. This tactic will facilitate anterior tooth eruption, alveolar growth, and open bite correction. Several kinds of fixed or removable appliances are available for this purpose. This tactic is very helpful in treatment of type I open bite, and if applied at the proper time such appliances can correct the problem without the need for further mechanotherapy (see cases 13-1 to 13-3).
As Rakosi3 and Huang et al12 have shown, the tongue crib has been used widely and successfully to stop thumb sucking and the abnormal tongue forces that produce and maintain anterior open bite.
2. Lip seal and swallowing exercises
To establish normal neuromuscular function and maintain stability of the result, lip seal and tongue exercises have been recommended.3,13 The patient is instructed to keep the lips together at all times and swallow without thrusting the tip of the tongue toward the maxillary or mandibular incisors. These exercises can be performed before appliance therapy and during treatment and then continued during retention.
3. Growth modification
The third tactic for open bite correction during the mixed dentition involves correction or guidance of the affected sites by controlling vertical growth, overeruption of the posterior teeth, and dentoalveolar development. This goal can be achieved by controlling the eruption or intrusion of the posterior segments. Overeruption of molars can occur in patients with prolonged finger sucking while the posterior teeth are not in contact.
Different devices have been proposed for this purpose: simple bite block, spring-loaded bite block, functional appliances, titanium screw anchorage, magnetic active vertical corrector, anterior extrusion arch. Two appliances that the author has designed and applied with excellent results— the tongue crib–transpalatal arch (TC-TPA) and the step-up or step-down anterior arch— are introduced here.
Tongue crib–transpalatal arch
The TC-TPA is a combination of a modified transpalatal arch and tongue crib (Fig 13-4). This appliance is made with 0.036- or 0.040-inch stainless steel wire and consists of two parts (the transpalatal arch and the tongue crib) in a one-unit appliance (see case 9). The transpalatal bar should be separated from the palate by at least 1 mm. The omega loop is located distally to help molar intrusion during swallowing. The tongue crib or tongue guard is designed as a vertical loop (see Fig 13-4a) or as a bow with vertical pieces of wire soldered to the arch (see Fig 13-4b).
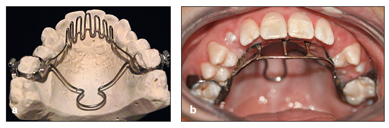
Fig 13-4 (a and b) TC-TPA appliance. This appliance can control tongue force, prevent molar eruption, and intrude the molars.
When the treatment plan for anterior open bite calls for intrusion of the maxillary molars, it is necessary to prevent overeruption of the mandibular molars at the same time; the results of intrusion of maxillary molars alone may not be effective. The best tactic for this purpose is insertion of a mandibular lingual arch at the same time.
Step-type anterior arch
In patients with a vertical growth pattern, early intervention can be followed with treatment of the permanent dentition by application of special archwires that the author has designed, the step-up and step-down anterior arches. Figure 13-5 shows a step-down anterior arch for the maxillary arch (see case 13-9).
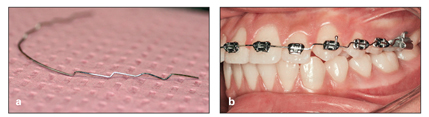
Fig 13-5 (a and b) Step-down anterior arch to intrude the posterior teeth and extrude the anterior teeth.
In severe open bites involving the maxilla, the mandible, and the dentition, two step-type arches can be applied at the same time: one step-down arch in the maxillary dentition and one step-up arch in the mandibular dentition. When skeletal open bite is combined with underdeveloped anterior dentoalveolar structure, vertical elastics can be added to step-down arches if vertical loops are incorporated in the maxillary and mandibular anterior segments.
The step-down and step-up arches can also be used in the treatment of deep bite problems by changing the direction of the steps opposite to what is used in open bite cases (see Deep Bite section later in chapter).
4. Closing the drawbridge
Another tactic suitable for elimination of some anterior open bites is retraction of proclined incisors. This method can be applied in patients with incisor spacing or after premolar extraction (Fig 13-6). This approach has been termed closing the drawbridge by Subtelny and Sakuda.14
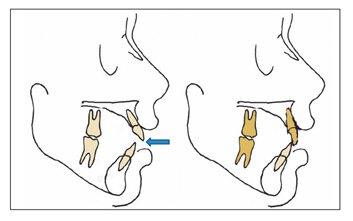
Fig 13-6 Retraction of incisors followed by gap closure (closing the drawbridge).
5. Increase of posterior facial height– anterior facial height ratio
Increasing the ratio of the posterior facial height to the anterior facial height is another tactic for correction of skeletal anterior open bite. Combinations of bite block and anterior vertical elastics or combinations of bite block with vertical chin cap or high-pull headgear have been used for this purpose by many investigators.15,16
6. Combined mechanotherapy with selective extraction
For some morphologic situations, selective extraction can be used along with mechanotherapy. These approaches include extraction of premolars to close the drawbridge in cases of anterior protrusion (see case 13-8) and extraction of permanent molars to close the bite by inducing counterclockwise rotation of the mandible (see case 13-10).
Case Reports
The following case reports show the different types of open bite: type I simple dental open bite (cases 13-1 to 13-3), type II combined dental open bite (case 13-4), and type III dentoskeletal open bite (cases 13-5 to 13-10).
Case 13-1: Type I open bite
A 14-year-old boy presented with an anterior open bite. He had a history of thumb sucking that was stopped by age 9 years, but a severe tongue thrust habit continued (Figs 13-7a to 13-7d).
Clinical, cast, and cephalometric evaluations indicated that he had a simple dentoalveolar open bite caused by persistent tongue thrust. No skeletal discrepancy or molar overeruption was evident.
Treatment:
The treatment plan called only for the application of a fixed tongue guard and tongue exercises (Fig 13-7e). This treatment was very effective and terminated after 9 months. The corrected occlusion was maintained with a Hawley retainer. Figures 13-7f to 13-7h show the posttreatment results.

Fig 13-7 Management of simple anterior open bite in a 14-year-old boy with a history of thumb sucking and severe tongue thrusting. (a to c) Pretreatment occlusion. (d) Activity of the tongue during deglutition. (e) Fixed tongue guard, the only appliance used. (f to h) Posttreatment occlusion.
Case 13-2: Type I open bite
A 12-year, 4-month-old girl in the late mixed dentition presented with a severe anterior dental open bite (3 to 5 mm) extending from the left primary second molar to the right primary second molar (Figs 13-8a and 13-8b). She had a Class I dentoskeletal pattern and no skeletal abnormality or divergence. According to the parents, no finger sucking was involved, but the patient had a prolonged history of pacifier use.
Treatment:
The problem was diagnosed as a dentoalveolar anterior open bite, and the treatment plan was simply to control tongue forces and instruct the patient in tongue exercises. Because the patient showed good compliance, the only appliance used was a removable tongue guard (Figs 13-8c and 13-8d). Figures 13-8e to 13-8g show the patient’s posttreatment occlusion.
Significant dentoskeletal changes that were achieved were anterior tooth eruption, slight retroclination of the incisors, change from open bite of –3.5 mm to overbite of 1.9 mm, reduction in overjet from 4.0 to 2.3 mm, and change in point A–nasion–point B (ANB) angle from 4.5 to 2.6 degrees (Figs 13-8h to 13-8j).
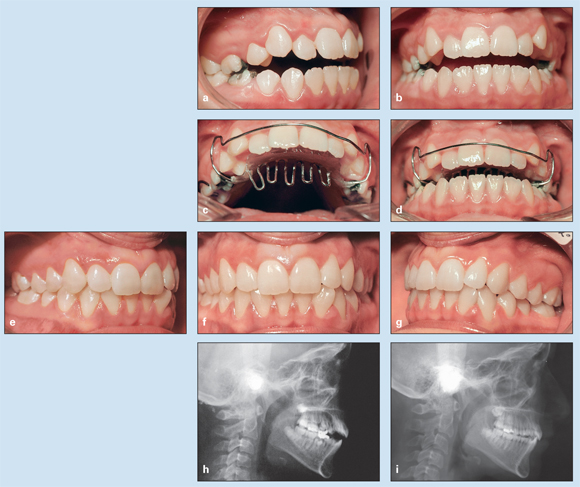
Fig 13-8 Management of severe anterior dental open bite extending from the maxillary left to maxillary right primary second molars in a 12-year, 4-month-old girl in the late mixed dentition. There is no skeletal abnormality. (a and b) Pretreatment occlusion. (c and d) Removable tongue guard, the only appliance used. (e to g) Posttreatment occlusion. (h) Pretreatment cephalometric radiograph. (i) Posttreatment cephalometric radiograph.
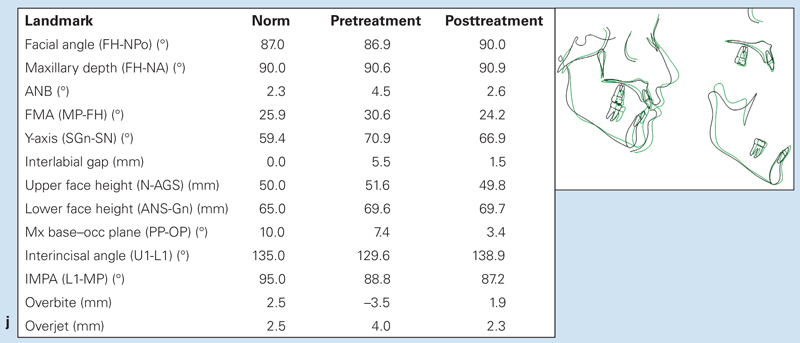
Fig 13-8 (cont) (j) Changes in cephalometric measurements and superimposition of pretreatment (black) and posttreatment (green) tracings.
Case 13-3: Type I open bite
A 9-year-old boy with thumb-sucking and tongue-thrusting habits presented with an anterior dental open bite, slight maxillary constriction, and a mandibular shift (Figs 13-9a to 13-9d). Clinical and paraclinical evaluations indicated that he had a type I simple dental open bite that originally was caused by thumb sucking and later was combined with tongue thrusting.
Treatment:
Because the slight maxillary constriction on the right side was causing mandibular shift, treatment was designed as a slight unilateral maxillary arch expansion with simultaneous control of tongue force. The appliance used was a quad helix unilateral expander with a tongue guard soldered to the anterior bow (Fig 13-9e). Figures 13-9f to 13-9h show the results after phase 1 treatment and correction of anterior open bite and posterior crossbite.
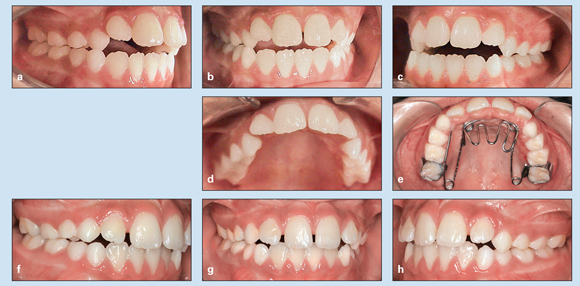
Fig 13-9 Management of anterior dental open bite, slight maxillary constriction, and mandibular shift in a 9-year-old boy with thumb-sucking and tongue-thrusting habits. (a to d) Pretreatment occlusion. (e) Unilateral quad helix expander with a tongue guard. (f to h) Occlusion after completion of phase 1 treatment and correction of anterior open bite and posterior crossbite.
Case 13-4: Type II open bite
A 9-year, 10-month-old girl presented with Class I occlusion, an anterior dentoalveolar open bite (type II combined open bite), and maxillomandibular dental protrusion (Figs 13-10a to 13-10c). She exhibited a tongue thrust habit and had a history of previous thumb sucking. Cephalometric analyses indicated that she had a slight vertical growth pattern (Frankfort plane–mandibular incisor angle [FMA], 30.6 degrees; y-axis, 73.4 degrees; lower facial height, 68.7 mm.
Treatment:
Based on the morphologic conditions, the treatment strategy was to control tongue force and to alleviate the vertical growth tendency by intrusion of the maxillary molars and prevention of extrusion of the mandibular molars, which would in turn correct the open bite and induce counterclockwise rotation of the mandible. This patient was given a maxillary TC-TPA to control the tongue force and simultaneously intrude the maxillary molars. A lower holding arch was used to prevent mandibular molar extrusion. Figures 13-10d to 13-10h show the results of treatment.
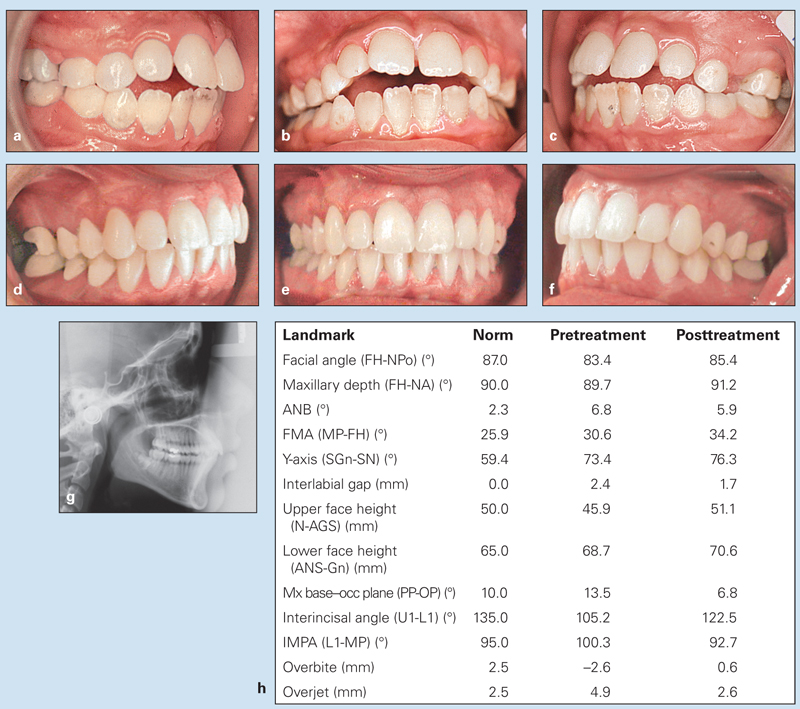
Fig 13-10 Management of Class I anterior dentoalveolar open bite with maxillomandibular dental protrusion and tongue thrusting in a 9-year, 10-month-old girl. (a to c) Pretreatment occlusion. (d to f) Posttreatment occlusion. (g) Posttreatment cephalometric radiograph. (h) Changes in cephalometric measurements.
Case 13-5: Type III open bite
An 11-year-old girl presented with Class I occlusion, a 3.5-mm anterior open bite, a tongue thrust, and a vertical growth pattern (Figs 13-11a to 13-11c). She had no history of finger sucking.
Treatment:
Treatment was designed to have two phases. Phase 1 was control of tongue forces and interceptive treatment (growth modification) to control the vertical growth pattern. Mechanotherapy at this stage was limited to a TC-TPA for maxillary molar intrusion and tongue control (Fig 13-11d) and a lower holding arch to control mandibular molar eruption (Fig 13-11e). Figures 13-11f and 13-11g show the change in occlusion after 8 months of interceptive treatment, which clearly resulted in molar intrusion (no contact in the molar area) and significant improvement of the anterior open bite. Significant cephalometric dentoskeletal changes were achieved in this phase of treatment (Figs 13-11h to 13-11j). These changes can be summarized as intrusion of maxillary molars, prevention of mandibular molar eruption, mandibular counterclockwise rotation, control of the increased lower facial height, and correction of anterior dentoskeletal open bite. Phase 2 will be carried out after complete eruption of the permanent dentition (excluding third molars).
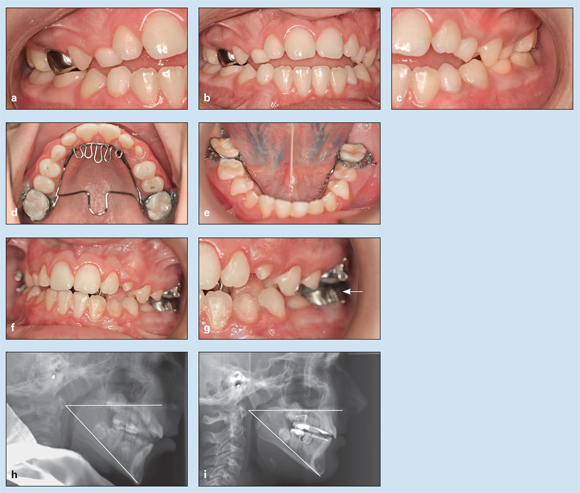
Fig 13-11 Management of Class I malocclusion and type III anterior open bite and tongue thrust in an 11-year-old girl. She has a vertical growth pattern and no history of finger sucking. (a to c) Pretreatment occlusion. (d) Combined TC-TPA for maxillary molar intrusion and tongue control. (e) Lower holding arch to control mandibular molar eruption. (f and g) Posttreatment occlusion with only 8 months of interceptive treatment. (arrow) Molar separation achieved by intrusion. (h)
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


