The treatment of children with cleft lip and palate requires three-dimensional thinking and the ability to carefully manipulate soft and hard tissues. The manner in which the initial phases of lip and palate reconstruction is accomplished directly affects secondary repair of the skeletal defect. All surgery creates scarring, and scarring may adversely affect growth. Patients with unrepaired clefts are less likely to have abnormal maxillary growth; therefore maxillary growth restriction may be the result of surgical intervention before the cessation of growth. With that in mind, the objectives of repairing the cleft maxilla are to close the alveolar fistula; provide adequate bone for the eruption of teeth; lift the slumped alar base and recreate the nasal floor; prevent periodontal defects to the adjacent teeth; unify the maxilla; reapproximate the oral soft tissues with alveolar mucosa and attached gingival tissues in the appropriate positions; reestablish the vestibule; provide a hygienic oral environment; and minimize the iatrogenic maxillary growth restriction.
HISTORY AND TIMING OF ALVEOLAR CLEFT REPAIR
There are many reports in the literature regarding timing and technique of cleft alveolar defect repair. Some advocate primary bone grafting in infancy, often at the time of lip repair. Others prefer secondary bone grafting, which is accomplished after the eruption of teeth but before eruption of the permanent canine or lateral incisor (if present). And still others try to avoid bone grafting altogether by doing a gingivoperiosteoplasty (GPP) at the time of lip repair in hopes that the osteogenic potential of the periosteum in infants will allow a bony bridge to form, rendering a later bone graft unnecessary. Review of the literature reveals that the first wave of interest was in primary bone grafting. This was stimulated in part by Axhausen in 1952, who became frustrated with the techniques of his time, which involved mucosal incisions and freshening of the underlying bone to try and promote bone healing.
Primary bone grafting became popular through the 1960s, and the literature is filled with reports of the technique and purported advantages. Although many reports emerged, so did a movement to review outcomes of early surgery and monitor facial growth. With the introduction of the cephalometric facial analysis, orthodontists became interested in facial growth and they became pivotal in the comprehensive management of patients with clefts. Most notably, Pruzansky emphatically lectured and published on the importance of record keeping, and although surgeons were “successfully” bone grafting cleft defects, he critically analyzed cases and was less than enthusiastic with the outcomes of primary grafting. Pruzansky and others demonstrated the severe growth restriction, dental crossbites, speech problems, and many surgical complications that patients experienced as a consequence of their surgical rehabilitation. The early 1970s marked the end of primary bone grafting in most centers. For a period of time after this, there was a backlash toward any procedure performed in this area before the cessation of growth.
However, during this time period Boyne and Sands adopted the philosophy that the development of the maxilla and dental eruption should guide the surgeon with regard to timing of surgery. Their philosophy changed the way bone grafting was performed, and their concepts have been the gold standard ever since they were introduced. Roughly 85% of midfacial growth is complete after the eruption of the first permanent molars. If the bone grafting procedure is performed at this time, there is much less iatrogenic growth restriction of the maxilla when compared with procedures performed earlier. Boyne and Sands advocated interceptive orthodontics for arch expansion, meticulous three-layer surgical closure, use of autologous bone, and soft-tissue coverage with keratinized tissue over the alveolar crest. Bergland and colleagues eloquently described the procedure and their results using iliac cancellous bone graft, documenting a 2.7% failure rate. Subsequent experience and published outcomes have supported these findings. There have been variations over the years with regard to timing and techniques, but this technique remains the preferred approach.
GRAFTING MATERIALS
Many grafting materials have been described, mostly via case reports, but the vast majority of the outcome data reveals that iliac crest autogenous graft is the material of choice. Alloplasts and allografts have been studied but do not demonstrate the same success rates or benefits as autogenous grafts. Many autogenous sources have been described—rib, calvarium, iliac crest, tibia, mandible—with outcome studies demonstrating highest success rates using iliac crest, followed by anterior mandible. There is significantly less bone available in the mandible for harvest, and it should probably be reserved for small bone grafting cases. Rib harvest is usually reserved for primary bone grafting in infancy, as it is easier to procure adequate bone in this age group. Cranium offers little cancellous bone, longer operating room time, and a potentially higher complication rate when compared with iliac crest bone. Procuring tibial bone carries a risk of growth disturbance in the pediatric patient, and the tibia also offers limited bone supply. This is particularly true for bilateral clefts. Early studies using bone morphogenetic proteins (rhBMP-2) are promising, but further research is required before their widespread use can be advocated.
GRAFTING MATERIALS
Many grafting materials have been described, mostly via case reports, but the vast majority of the outcome data reveals that iliac crest autogenous graft is the material of choice. Alloplasts and allografts have been studied but do not demonstrate the same success rates or benefits as autogenous grafts. Many autogenous sources have been described—rib, calvarium, iliac crest, tibia, mandible—with outcome studies demonstrating highest success rates using iliac crest, followed by anterior mandible. There is significantly less bone available in the mandible for harvest, and it should probably be reserved for small bone grafting cases. Rib harvest is usually reserved for primary bone grafting in infancy, as it is easier to procure adequate bone in this age group. Cranium offers little cancellous bone, longer operating room time, and a potentially higher complication rate when compared with iliac crest bone. Procuring tibial bone carries a risk of growth disturbance in the pediatric patient, and the tibia also offers limited bone supply. This is particularly true for bilateral clefts. Early studies using bone morphogenetic proteins (rhBMP-2) are promising, but further research is required before their widespread use can be advocated.
ORTHODONTICS
The orthodontist is an integral cleft team member and has a number of roles. His or her recommendations regarding timing of treatment, based on growth, should be considered carefully when surgical interventions are planned. By age 4 or 5 the effects of surgical scarring on growth may become apparent. Although techniques have improved, surgically treated patients with clefts have a tendency toward both anterior and posterior crossbites, which are less frequently seen in patients with untreated clefts. A number of acceptable treatment strategies may be used, but of paramount concern is to maximize outcomes while minimizing the time in orthodontic treatment. Treatment timing can be categorized into three main opportunities, discussed in the following sections.
PRESURGICAL MOLDING IN INFANCY
Some practitioners prefer using alveolar or nasoalveolar molding appliances before surgically correcting the cleft lip. These molding devices have been used for several decades, and considerable controversy exists regarding their risks and benefits. For most practitioners who favor this approach, the appliance is used to approximate the alveolar segments to allow GPP to be performed during the primary lip repair. This approach attempts to reconstruct the cleft maxilla during the primary repair in the hopes of avoiding the need for primary bone grafting. Proponents of this technique believe that closure of the alveolar ridge tissue may allow for enough bone to be present for subsequent tooth eruption and therefore avoid the need for a donor site. Data regarding the outcome of the teeth, dental arch form, and other outcome factors have yet to be published in a convincing fashion. Given the experience of the 1960s with primary bone grafting, many surgeons and orthodontists believe that significant growth restriction may occur with this type of early intervention. It is hoped that additional data will be forthcoming regarding the utility and outcomes of this technique.
PHASE I ORTHODONTICS (AGES 6 TO 10)
The goals of phase I orthodontic therapy include optimizing the position of the dentoalveolar structures and encouraging growth in appropriate dimensions if discrepancies are noted early. A portion of this phase may be omitted if jaw growth is progressing well. Some practitioners use reverse-pull headgear when maxillary hypoplasia is present. Historically this phase commences in time to ensure bone grafting when the root of the permanent cuspid is two-thirds formed. For many contemporary practitioners, this may occur once the eruption of the centrals and sometimes the laterals has commenced.
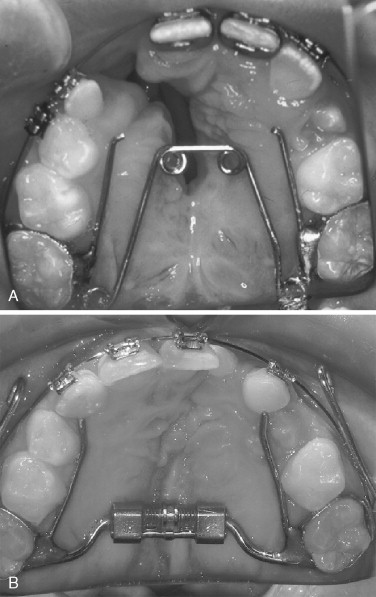
There are generally two scenarios that require phase I orthodontics; the goal of both is to prepare the patient for bone grafting. The first scenario occurs when there is normal intermolar width but the intercanine dimension is narrow owing to collapse of the lesser segment. This requires the use of an appliance with the ability to hold the transverse width in the posterior maxilla and create expansion anteriorly with a quad helix ( Figure 40-1, A ). The second scenario typically requires the placement of a hyrax rapid palatal expander. In this scenario a posterior crossbite exists in the molar and/or premolar region. Patients with posterior crossbites frequently have large anterior collapse of the lesser segment, necessitating modification of the expander ( Figure 40-1, B ).
Differential expansion in a patient with a cleft is challenging for many reasons. There is scar rather than bone across the palate, which allows quick but less predictable movements. This leads to less control of the segments and dental midlines. If incisors are present, brackets may also be placed to assist with midline control, as well as to treat rotations and anterior crossbites. The orthodontist must avoid tooth movement (especially roots) toward the cleft site, and on occasion orthodontic treatment with brackets and wire must be delayed until after bone grafting. When the maxillary arch form and crossbites are corrected, the cleft defect will be widened and the alveolar fistula made larger. This will typically create more air escape and fluid regurgitation and may worsen speech temporarily. Speech improves after grafting is complete, and the appliance can be removed. It is important to discuss these issues carefully with the parents before initiating treatment.
COMPREHENSIVE PHASE II ORTHODONTICS
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


