Management of Incisor Crowding
Incisor crowding is one of the most frequently observed dental phenomena in young children during the early and middle mixed dentition periods. Incisor crowding has been a subject of increasing concern for children and their parents, and it is among the most common reasons patients seek orthodontic treatment.
Because of the discrepancy between primary and permanent incisors, some degree of incisor crowding is very common during the early mixed dentition. Some of this crowding can be transitional and needs no intervention, some can be corrected with occlusal guidance and space supervision, and some can be critical and develop to a severe malocclusion and therefore must be managed with tooth extraction at the proper time.
Overall space availability for all dentition varies, depending on the growth of the jaws and relative variation in the mesiodistal crown diameters of the permanent teeth and their predecessors. Children who have little or no developmental spacing between the primary incisors and occasionally some crowding in the primary dentition develop severe crowding in the permanent incisors. As Baume1 showed, children with no spacing during the primary dentition (Baume class II) have a 40% chance of developing crowding in their permanent incisors.
Mandibular anterior crowding is initially identified as a discrepancy between the mesiodistal tooth widths of the four permanent incisors and the available space in the anterior part of basal bone. However, many other variables must be considered prior to early intervention and treatment, such as the direction of mandibular growth, early loss of primary molars, incisor and molar inclinations, and oral and perioral musculature balance. All of these factors can play a role in and be associated with incisor crowding.
Because not all incisor crowding during the mixed dentition is alike, the treatment procedure must vary depending on the etiology and morphology of the crowding. However, this common problem sometimes is a cause of great concern for parents and patients, so practitioners must be prepared to address this issue with parents. The most appropriate answer to their questions is not, “This is not a problem,” or “Wait until all permanent teeth erupt.” Rather, the wise and proper answer is, “This might be a sign of other problems, so the situation should be evaluated now.”
The next question for practitioners is how to identify and differentiate different situations of incisor crowding to enable optimal management of each case. This chapter will answer this question by examining different aspects of incisor crowding:
• Is there any way to predict this problem?
• What is the common cause of this problem?
• How can different types of crowding be classified and differentiated?
• What kind of intervention can prevent the problem?
• How can the problem be treated?
Prediction
Predicting permanent incisor crowding at an earlier stage has been a goal in several longitudinal studies during the primary, mixed, and permanent dentitions. However, there are conflicting results in the literature evaluating the correlation between crowding and other dentofacial structures. Baume1 reported that children with no spacing during the primary dentition (Baume class II) have a 40% chance of crowding in their permanent incisors.
Hunter,2 after analysis of crowding and spacing of the teeth, concluded that estimates of the size of unerupted teeth in the mixed dentition are more accurate than estimates of future spacing or crowding; this is because arch perimeter does not decrease by the same amount in all cases but is rather associated with the amount of crowding in the mixed dentition. The amount of crowding or spacing must always be determined after considering molar, canine, and incisor relationships as well as the condition of lip posture on the dentition.
Sampson and Richards3 tested the hypothesis that pre-eruptive tooth positions and dental arch parameters might forecast crowding changes in Class I untreated dentition unaffected by caries or attrition. Crowding scores, radiographic relationships, and dental arch dimensions were evaluated for the mixed dentition. The sample was divided into two groups, depending on whether there was an increase or decrease in incisor and canine crowding between the mixed and the permanent dentitions. Dental arch form and tooth size were important factors in measuring the amount of incisor or canine crowding at stage 1 and stage 2. The researchers found that neither the radiographic nor the dental arch predictors proved useful in forecasting crowding changes.
Howe et al4 examined the extent to which tooth size and jaw size each contribute to dental crowding. Two groups of dental casts were selected on the basis of dental crowding. In one group, 50 pairs of dental casts exhibited gross dental crowding. The second group consisted of 54 pairs of dental casts that exhibited little or no crowding. Howe et al4 observed significant differences between the dental arch dimensions of the two groups. The crowded group was found to have smaller dental arch dimensions than the noncrowded group. The researchers suggested that practitioners should consider treatments that increase dental arch length rather than those that reduce tooth mass.
Bishara et al5 attempted to determine the changes in the maxillary and mandibular tooth size–arch length discrepancy between the primary dentition (mean age of 4.0 years) and second molar eruption (mean age of 13.3 years) to establish whether a tooth size–arch length discrepancy in the permanent dentition can be predicted in the primary dentition. They evaluated the records of 35 boys and 27 girls. The mesiodistal diameters of all primary teeth and their permanent successors, as well as various parameters of dental arch width and length, were measured in the primary and permanent dentitions.
The researchers concluded that additional factors are involved in tooth size–arch size discrepancy and should be considered in explaining this phenomenon. These factors are present in most persons, whether or not they have a malocclusion or have undergone orthodontic treatment. Regression analysis indicated that these changes are related, in part, to tooth size as well as to changes in arch length and arch width. The correlations between the various primary and permanent tooth size–arch length discrepancies are of such a magnitude that they do not allow accurate prediction of discrepancies in the permanent dentition from the available dental measurements in the primary dentition.5
Sinclair and Little6 also found no clinically significant associations between various mandibular parameters and incisor crowding.
Melo et al7 searched for indicators during the primary dentition of future crowding of the mandibular incisors during the early mixed dentition. For this purpose, they examined the skeletal and dental morphologic characteristics of the primary dentition using dental casts and cephalograms of 23 subjects. They then assessed the degree of crowding in the same subjects at 9 years of age and found 12 normal and 11 crowded dentitions. The size of permanent incisors in the crowding group was significantly greater than that in the normal group. The maxillary and mandibular dental arch lengths and the posterior cranial base length (sella-basion) were also effective discriminators between the two groups.
Common Causes
Conducting an implant study in children, Björk8 clearly showed that the direction and rotational pattern of mandibular growth have different effects on occlusion, incisor position, and crowding. In fact, the same implant studies revealed that internal jaw rotation also changes the anteroposterior position of the incisor teeth, which in turn has a major influence on changes in arch length. They showed that the rotational pattern of jaw growth obviously influences the magnitude of tooth eruption. When the mandible rotates downward and backward, anterior facial height increases, there is a tendency toward anterior open bite, and the incisors are thrust forward relative to the mandible. When excessive counterclockwise rotation occurs, short facial height develops, and lingual displacement of the incisors relative to the maxilla and mandible increases the tendency toward crowding.
Leighton and Hunter9 also reported that the angles between the sella-nasion line and the mandibular and occlusal planes were significantly larger in patients with crowding during both the mixed and permanent dentition stages. They also associated downward and deficient growth of the mandible with upright or retroclined mandibular incisors and with crowding.
Sayin and Türkkahraman10 tried to find factors that can contribute to mandibular anterior crowding. They evaluated 60 dental casts of patients during the early mixed dentition, divided into two groups according to the severity of mandibular anterior crowding. In the mandible, the primary intercanine widths, intermolar widths, permanent intermolar widths, interalveolar widths, space available for the mandibular permanent incisors, and total arch length were all significantly larger in patients with crowding than they were in patients without crowding. No significant correlation was found between crowding and total arch length.
Türkkahraman and Sayin11 evaluated the association between dentofacial structures and mandibular crowding during the early mixed dentition by analyzing cephalometric radiographs and casts of 60 children. They found that children with crowding had smaller mandibular incisor–nasion–point B angles and shorter maxillary and mandibular skeletal length. They also found greater interincisal angles, overjet, overbite, and Wits appraisal measurements. They concluded that crowding of the mandibular incisors is not merely the result of a tooth size–arch size discrepancy; dentofacial characteristics also contribute to this misalignment.
Intervention and Prevention
Despite much research and many longitudinal investigations to find special characteristics and criteria for early detection and prevention of permanent incisor crowding during the primary dentition, there is still much controversy on the subject. Practitioners still see young children with incisor crowding that was not prevented and highly concerned parents seeking some kind of early intervention. Nevertheless, incisor crowding during the mixed dentition can be managed differently depending on the amount of crowding and other variables involved in this process, and all factors must be considered in treatment planning.
There is no reliable criterion during the primary dentition to predict permanent incisor crowding, but even if it were possible prevention is not possible until all incisors are erupted. However, the author’s clinical experience in some early treatment during the primary dentition indicates that some type of early intervention, even before eruption of permanent incisors, can be useful in providing space for the permanent incisors. For example, during rapid palatal expansion in the primary or early mixed dentition for correction of posterior crossbite, some space can develop for incisors and canines, facilitating normal eruption of the anterior segment (Fig 5-1; see the discussion on early correction of posterior crossbite in chapter 12).
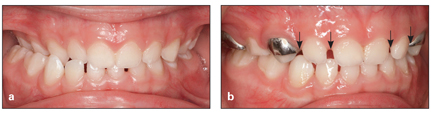
Fig 5-1 (a and b) Space opening (arrows) after rapid expansion and posterior crossbite correction.
Moreover, clinical observation indicates that an abnormal sequence of eruption between mandibular canines and first premolars has a tendency to precede some kinds of mandibular incisor crowding, and in such cases early detection and proper intervention can reduce or correct incisor crowding. Other examples of prevention and early intervention for mandibular incisor crowding are control of some types of thumb sucking to retrude the mandibular incisors and control of lower lip dysfunction that can cause mandibular incisor crowding.
Longitudinal monitoring of panoramic radiographs and the three phases of transitional dentition is a prudent measure that can be considered the first step in prevention and early intervention.
Characteristics and Classification
Mandibular anterior crowding is identified as a discrepancy between the mesiodistal tooth widths of the four permanent incisors and the space available between the mesial surfaces of the primary canines. Because crowding can result from different morphologic and etiologic factors, the first step for the purpose of proper treatment planning is to identify the kind of crowding, that is, to determine the amount of permanent incisor crowding during an early stage of the mixed dentition. This can be achieved by careful measurement and analysis of tooth size–arch size discrepancy (see chapter 4).
However, incisor crowding is not merely a tooth size–arch size discrepancy. Many variables, such as direction of mandibular growth, early loss of primary molars, the oral and perioral musculature, and incisor and molar inclinations, can be associated with crowding. Thus, the second issue for proper treatment planning is to search for dentofacial factors that might be associated with mandibular crowding, using all necessary diagnostic tools during the early mixed dentition.
After careful assessment of the aforementioned variables, incisor crowding can be arbitrarily classified into three types of crowding:
1. Minor crowding up to 3 mm of space deficiency
2. Moderate crowding with 3 to 5 mm of space deficiency
3. Severe crowding with more than 6 mm of space deficiency
However, the amount of crowding in millimeters is not the only decisive criterion for treatment decisions; many other factors must be evaluated and considered in treatment planning. The purpose of this classification is to provide the first practical step of discriminating between different amounts of crowding.
Generally incisor crowding has been classified into two general types, acquired crowding and hereditary crowding, which are discussed in detail later in this chapter.
Treatment
Although incisor crowding is not merely a function of tooth size–arch size discrepancy and many other local and general variables might be involved and must be evaluated, for practical purposes the treatment options have been classified according to the amount of incisor crowding (minor, moderate, and severe crowding).
Minor Crowding
Because of the size difference between primary and permanent incisors (incisor liability), a minor amount of permanent incisor crowding (less than 3 mm) at an early stage of the mixed dentition is considered transient crowding; up to 3 mm of incisor crowding may resolve spontaneously during the transitional dentition without the need for early intervention.
Studies of children with normal occlusion also indicate that transitional changes from the primary to the mixed dentition resolve up to 3 mm of incisor crowding spontaneously without treatment. As was discussed in chapter 2, there are natural mechanisms that can self-correct minor crowding of incisors during the transitional dentition, such as interdental spacing, more proclination of permanent incisors, and intercanine width increase.
Moorrees and Reed12 studied a series of 184 casts at 3 years and 16 to 18 years of age. They found that, in the mandible, an average of 1.6 mm of crowding in boys and 1.8 mm of crowding in girls will recover to 0.0 mm by the age of 8 years. They attributed this recovery to a phenomenon termed secondary spacing, which facilitates lateral incisor eruption. This process occurs when the mandibular lateral incisors emerge and push the mandibular primary canines laterally. This also causes the maxillary primary canines to move laterally by occlusal force, creating spaces for the maxillary lateral incisors.
Extraction of the mandibular primary canines during this natural phenomenon will prevent secondary spacing and the increase in intercanine width. Prevention of this phenomenon may even convert a nonextraction case to an extraction case. Therefore, no greater relief of spacing in the incisor segment can be expected after complete eruption of the lateral incisors. They also added that the level of dental maturation, that is, tooth formation and emergence, gives decisive clues for diagnosis and treatment planning because it defines the timetable of individual development.12
It is also important to remember that physiologic self-correction of minor crowding can occur, provided that the following factors are present:
• Normal growth and development of the jaws
• Normal interdental spacing, especially primate spaces
• Normal labial inclination of the maxillary and mandibular incisors
• Normal increase in intercanine width
• On the other hand, the presence of any of the following disturbances can disrupt self-correction of minor crowding and change the treatment plan:
• Premature loss of primary teeth
• Problems of tooth number, size, or form
• Abnormal habits
• Soft tissue problems, such as lip dysfunction
• Hereditary or congenital disturbances
Therefore, for patients with minor incisor crowding, practitioners must carefully monitor the transitional dentition and maintain arch length integrity against any abnormal factors such as interproximal caries, accidental tooth loss, or abnormal habits.
Moderate Crowding
Moderate mixed dentition crowding is the presence of 3 to 5 mm of crowding during the transitional stage of dentition. Depending on the variable conditions of occlusion, moderate crowding can be treated differently at different stages of transition. Treatment can take place from the time of eruption of the mandibular permanent central incisors (around 6 years) to the late mixed dentition stage (around 11 to 12 years).
Permanent incisor buds are located lingual to the root of primary incisors and, especially in mandibular dentition, they often erupt lingually. Therefore, monitoring is very important at this stage of transition. For example, delayed exfoliation of primary incisors might be problematic; sometimes permanent central incisors erupt lingually while primary central incisors are still present and immobile. In this situation, immediate radiographic evaluation and extraction of the over-retained primary teeth must be performed (Fig 5-2).
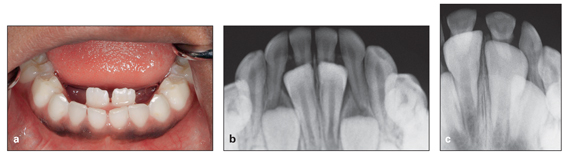
Fig 5-2 (a to c) Delayed resorption of the primary central incisor roots, causing lingual eruption of the permanent incisors.
If the primary canine has already exfoliated or been extracted without supervision and some space has been lost, a space regainer such as a lip bumper should be used to regain the lost space. Afterward, use of a lingual holding arch or fixed appliance is recommended (for more detail on space regaining, see chapter 4).
If, on the other hand, space analysis and evaluation of all other perioral factors indicate that the space available in the arch and basal bone can accommodate all incisors, canines, and premolars and there is no evidence of space loss resulting from early loss of the primary dentition or caries, moderately crowded incisors can be guided to better positions by careful space management in the posterior segment of the arch, in a procedure called space supervision. In other words, when space analyses indicate that there is “just enough” space, the situation is a borderline case for extraction, and an attempt should be made to correct moderate crowding through supervision of the transitional dentition to prevent loss of leeway space. Moyers13 described space supervision cases as those that will make it through the mixed dentition better with clinical guidance than without it.
Proper selection of cases and a thorough case evaluation are always necessary for this tactic. In patients with moderate anterior crowding, space supervision can be applied through four different tactics:
1. Sequential stripping of primary teeth
2. Preservation of E space
3. Space creation
4. Combination approach, using more than one of the aforementioned methods
Sequential stripping of primary teeth
Sequential stripping of primary lateral incisors, canines, or molars can allow spontaneous alignment of incisors and distal eruption of the canines and premolars without any mechanotherapy. Minor amounts of stripping do not cause patient discomfort. Greater amounts of slicing may require administration of local anesthesia and produce some postoperative sensitivity; fluoride therapy helps alleviate the sensitivity. It is possible to gain as much as 4 mm (maximum) of anterior space through this procedure. This procedure can be done by stripping metal tape or a fine flexible diamond disk.
Space supervision and slicing of primary teeth can be applied during eruption of the mandibular permanent lateral incisors, which usually have more difficulty in erupting than central incisors because of their size. Disking of the mesial surface of the primary canine can resolve the problem. In some cases of severe space deficiency, it may be necessary to extract the primary canines, but immediate insertion of a lower holding arch with spurs is indicated to prevent any space loss that can result from lingual movement of mandibular incisors (Fig 5-3).

Fig 5-3 Lower holding arch with spurs.
When disking or extraction of the mandibular primary canine is planned, the normal transitional process of secondary spacing must be considered. The disking or extraction must be timed so as not to disrupt the development of secondary spacing.
Another example of sequential stripping is disking of the mesial surface of the primary first molar to provide space for the mandibular permanent canine and guide distal eruption of the canine helping spontaneous correction of moderate incisor crowding. Likewise, the mesial surface of the primary second molar can be stripped to facilitate and guide first premolar eruption. With this technique, the moderate incisor crowding is actually transferred to the posterior segment, taking advantage of leeway space, without use of any appliances.
Another example of selective grinding is disking of the distal surface of the mandibular primary second molar. This procedure is indicated when the maxillary permanent first molar has erupted before the mandibular molar. Distal stripping of the primary second molar accelerates mesial migration of the mandibular molar to achieve a Class I molar relationship.
Preservation of E space
Preservation of E space, or guidance of eruption in moderate incisor crowding, is another kind of space supervision that can be applied after careful evaluation of dentofacial structures and muscles, space analysis, and confirmation of a moderate space deficiency.
Gianelly14 stated that the late mixed dentition stage of dentition, after the eruption of the first premolars, is a favorable time to start treatment to resolve incisor crowding. Moyers13 and Gianelly15 suggested that in the majority of individuals with moderate crowding in the early mixed dentition, this technique provides adequate space to resolve the moderate incisor crowding.
The author suggests that the optimum time to apply this procedure is before exfoliation of both primary first and second molars. Insertion of a proper lingual holding arch connected to the permanent first molars before exfoliation of the primary first and second molars will prevent any mesial shift of the first permanent molar to leeway space. This tactic will preserve 2 to 4 mm of space for crowded incisors.
After insertion of a good lower holding arch to prevent any mesial shift of the permanent molars, extraction of the primary first molar will actually guide the first premolar eruption more distally. Subsequently, the canine can move distally to facilitate spontaneous correction of incisor crowding.
Preservation of E space and guidance of eruption of premolars can be applied in patients with primary molar ankylosis and tilted eruption of premolars.
The best appliances to preserve E space or prevent mesial movement of permanent molars are the lower holding arch in the mandible and the transpalatal arch in the maxilla (Fig 5-4).
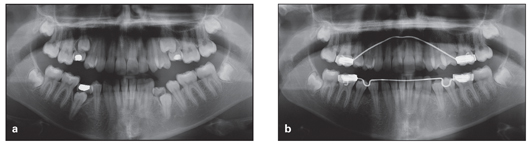
Fig 5-4 (a and b) Preservation of E space to allow normal eruption of premolars.
Space creation
Space creation is another means of correcting moderate incisor crowding (3 to 5 mm of crowding) during the mixed dentition. The procedure of space creation is different from space regaining, which is the procedure to apply when existing space has been lost due to early loss of primary teeth. Rather, space creation is a procedure to create needed space. Space creation is a more complex procedure and needs much more evaluation and analysis before any treatment planning. This procedure can be performed in the following ways:
• Transverse expansion
• Sagittal expansion (anteroposterior arch length increase)
• Selective stripping
• Combination of the aforementioned methods
For more details about space creation, see chapter 4.
Combination approach
Incisor crowding during the transitional dentition is a common problem that worries patients and parents. In many patients, the problem can be treated with nonextraction procedures at an early age, while tooth extraction will be required if the treatment is postponed to the permanent dentition.
Clinical experience indicates that this kind of crowding usually develops during incisor transition as a result of a combination of etiologic factors such as early primary tooth loss, trauma, supernumerary teeth, missing teeth, Bolton discrepancy, abnormal habits, abnormal muscle function, abnormal basal bone relationships such as deep bite, or anterior crossbite. Thus, the practitioner must take advantage of all the examinations and diagnostic tools available to search for dentofacial factors in the early mixed dentition that might be associated with mandibular crowding.
As discussed earlier, Björk and Skieller16 reported that the mandibular growth pattern and mandibular rotation affect incisor position and crowding. When the mandible rotates downward and backward, anterior facial height increases, there is a tendency toward anterior open bite, and the incisors are thrust forward relative to the mandible. When excessive counterclockwise rotation occurs, a short facial height results, and lingual displacement of the incisors relative to the maxilla and mandible increases the tendency toward crowding. Therefore, these types of crowding with multifactorial causes cannot be managed by space supervision or space creation alone. However, elimination or prevention of the causes, especially through early detection and proper intervention, can result in a stable and balanced occlusion. The following cases are examples of this type of crowding that can be managed at an early age.
Case 5-1
A 10-year, 8-month-old boy presented with a Class I malocclusion, locked anterior crossbite (without mandibular shift), maxillary incisor crowding, displacement, and a diastema (Figs 5-5a to 5-5e).
A panoramic radiograph taken about 1 year after an accident (Fig 5-5f) revealed the effect of trauma to the permanent incisors (early resorption of the left primary central and lateral incisors and delayed resorption of the right primary lateral and central incisors), causing delayed eruption of the right permanent central and lateral incisors, tilting to crossbite, and mandibular crowding (Fig 5-5g to 5-5j).
Treatment:
Treatment was started with 2 × 4 maxillary bonding and placement of composite resin on the occlusal surfaces of the mandibular molars to disocclude the anterior segment. A nickel-titanium archwire was also placed for leveling, followed by a stainless steel archwire with open loop for correction of incisor crossbite.
After crossbite correction was completed, mandibular bonding was performed for correction of incisor crowding. Figures 5-5k and 5-5l show the dentition during treatment. Figure 5-5m reveals the change of canine inclination. This patient was then treated only with 2 × 6 maxillary and mandibular bonding. Figures 5-5n to 5-5r show the final posttreatment occlusion.
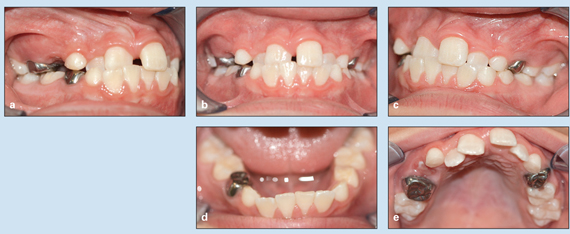
Fig 5-5 Treatment of a 10-year, 8-month-old boy with a Class I malocclusion, locked anterior crossbite, maxillary incisor crowding, displacement, and a diastema. (a to e) Pretreatment occlusion.

Fig 5-5 (cont) (f) Magnified panoramic radiograph, taken about 1 year after trauma, reveals displacement of the maxillary permanent right lateral incisor. (g to j) Consecutive pretreatment panoramic radiographs. (k and l) Dentition during treatment. (m) Panoramic radiograph during treatment, revealing the change in canine inclination. (n to r) Posttreatment occlusion.
Case 5-2
A 10-year-old girl presented with an anterior locked occlusion that caused severe crowding and displacement of the mandibular incisors (Figs 5-6a to 5-6f).
Treatment:
A nonextraction treatment procedure was planned. Treatment was started with mandibular 2 × 6 bonding and application of composite resin on the occlusal surfaces of the mandibular first molars to disocclude the anterior segment. After correction of crossbite and proclination of all of the maxillary incisors, mandibular 2 × 3 bonding was used first to align three incisors and create space for the mandibular right lateral incisor. The final step was traction of the severely displaced right lateral incisor into the arch and alignment (Figs 5-6g to 5-6l).

Fig 5-6 Treatment of a 10-year-old girl with severe anterior crowding. (a to e) Pretreatment occlusion. (f) Pretreatment panoramic radiograph. (g to k) Posttreatment occlusion. (l) Posttreatment panoramic radiograph.
Case 5-3
A 10-year-old boy presented with a Class I very deep bite (impinging) and retroclined maxillary and mandibular incisors. He had severe mandibular incisor crowding, and the mandibular right lateral incisor was completely displaced lingually. Early loss of the mandibular primary incisors and deep bite resulted in mandibular anterior collapse and some retrusion of the maxillary incisors (Fig 5-7a to 5-7f).
Treatment:
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


