27 Malignant Salivary Gland Neoplasms—Classification
Histogenesis of Malignant Salivary Gland Neoplasms
Polymorphous Low-Grade Adenocarcinoma
Carcinoma Ex Pleomorphic Adenoma
Other Rare Salivary Gland Malignancies
Epithelial–Myoepithelial Carcinoma
Clear Cell Carcinoma, Not Otherwise Specified
Low-Grade Cribriform Cystadenocarcinoma
Adenocarcinoma, Not Otherwise Specified
Metastasizing Pleomorphic Adenoma
Introduction
The 2005 revised World Health Organization (WHO) histological classification1 of salivary gland tumors includes 24 carcinomas (Table 27.1). The main changes from the 1991 classification involved the introduction of new entities—clear cell carcinoma, not otherwise specified; sialoblastoma; low-grade cribriform cystadenocarcinoma (low-grade salivary duct carcinoma); and cribriform adenocarcinoma of the tongue, a variant of polymorphous low-grade adenocarcinoma. Several of the subtypes have been accorded separate categories of their own—carcinoma ex pleomorphic adenoma, carcinosarcoma, metastasizing pleomorphic adenoma, sebaceous neoplasms, sebaceous lymphadenoma/carcinoma, lymphoepithelial carcinoma, and small cell and large cell undifferentiated carcinomas. Clinicians consider all of these new categories and new entities to be clinically rare and seldom encountered, but they have to be identified when patients present with them.
The majority of salivary gland malignancies, whether in the major or minor salivary glands, are covered by: acinic cell carcinoma, mucoepidermoid carcinoma, adenoid cystic carcinoma, and polymorphous low-grade adenocarcinoma. Other malignant tumors that are of interest to surgeons include: salivary duct carcinoma, oncocytic carcinoma, carcinoma ex pleomorphic adenoma, metastasizing pleomorphic adenoma, and undifferentiated carcinoma.
The surgical pathologist’ s view is that any classification is dynamic rather than static and at best represents no more than a consensus of those individuals involved at the time of its formulation. Any tendency to regard a classification as immutable should be firmly resisted. The primary function of the pathologist is to produce as precise a diagnosis as possible. It is only by evaluation and subsequent clinical experience of the behavior of lesions and their responses to a variety of treatment protocols that the relative importance of the individual diagnosis can be established. It is in this area of precise diagnosis that the value of an extended classification of salivary gland tumors becomes most evident. Broad prognostic groupings and tumor grades are of no help if the initial diagnostic category has been incorrect.2
Histogenesis of Malignant Salivary Gland Neoplasms
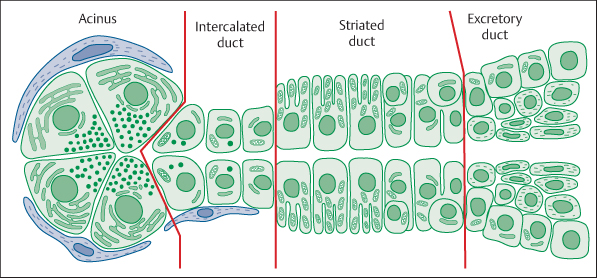
To understand the histogenesis of salivary gland neoplasms, it is necessary to understand the composition of the salivary gland unit. Each unit is made up of serous or mucous acini that lead to an intercalated duct, which in turn is connected to a striated duct that finally empties into an extralobular excretory duct. Myoepithelial cells are located around the periphery of the acini and intercalated duct (Fig. 27.1). It is generally accepted that the basal cells of the excretory duct and intercalated duct cells act as reserve cells for the more differentiated cells of the salivary gland unit. The basal cells of the excretory duct give rise to the acinar cells, intercalated duct cells, striated duct cells, and probably the myoepithelial cells. As reserve or progenitor cells, the basal cells and intercalated duct cells thus play a pivotal role in the development of the salivary glands, as well as tumor formation. They are referred to as excretory duct reserve cells and intercalated duct reserve cells.3,4
|
Entity |
Specific features |
|
Acinic cell carcinoma |
All ages affected; staging better predictor than grading |
|
Mucoepidermoid carcinoma |
Most common salivary malignancy in adults and children; outcome mostly favorable |
|
Adenoid cystic carcinoma |
Outcome usually fatal; typically slowly growing mass followed by pain (perineural spread), lymph-node involvement uncommon, radiotherapy may improve local control |
|
Polymorphous low-grade adenocarcinoma |
Low metastatic potential, palate involved in 60% of the cases; excellent prognosis |
|
Epithelial–myoepithelial carcinoma |
Female preponderance, peak incidence in the sixth and seventh decades of life, mainly major glands, may ulcerate when located in minor glands; frequently recurs and/or metastasizes |
|
Clear cell carcinoma, not otherwise specified |
More frequent in minor glands (palate); ulceration may be present; excellent prognosis |
|
Basal cell adenocarcinoma |
> 90% occur in the parotid, mostly asymptomatic except for swelling, metastasize only occasionally |
|
Sebaceous carcinoma |
Arise mainly in the parotid, bimodal age distribution (third and seventh to eighth decades of life) |
|
Sebaceous lymphadenocarcinoma |
Extremely rare, only three cases have been reported |
|
Cystadenocarcinoma |
Rare, often a slowly growing compressible asymptomatic tumor; good prognosis |
|
Low-grade cribriform cystadenocarcinoma |
Resembles breast lesions, located in the parotid, usually present in the elderly female (originally low-grade salivary duct carcinoma) |
|
Mucinous adenocarcinoma |
Rare, palate and sublingual glands affected, insensitive to irradiation |
|
Oncocytic carcinoma |
Usually preexisting oncocytoma, frequent recurrence and regional and/or distant metastases |
|
Salivary duct carcinoma |
9% of all salivary malignancies; typically a rapidly growing parotid mass that may fluctuate in size, male preponderance, very aggressive |
|
Adenocarcinoma, not otherwise specified |
No pathognomonic histopathological features; inconsistent reporting, since many cases reported should be classified as more specific types; limited data on prognosis |
|
Myoepithelial carcinoma |
< 2% of all salivary malignancies; 75% arise in the parotid, half of the cases develop in preexisting pleomorphic adenoma, histomorphology correlates with diverse clinical outcomes |
|
Carcinoma ex pleomorphic adenoma |
12% of all salivary malignancies; subclassification mandatory into invasive (extremely aggressive) or noninvasive/minimally invasive (excellent prognosis, no need for neck dissection or irradiation) |
|
Carcinosarcoma |
Extremely rare; some patients have a history of recurrent pleomorphic adenoma |
|
Metastasizing pleomorphic adenoma |
Extremely rare; only 40 cases described to date |
|
Squamous cell carcinoma |
Restricted to the major glands; < 1% of all salivary malignancies, prior irradiation frequent, very aggressive, locoregional recurrence in > 50% |
|
Small cell carcinoma |
2% of all salivary malignancies, recurrence and distant metastasis develop in > 50% |
|
Large cell carcinoma |
Extremely rare, very aggressive, tumor size > 4 cm indicates poor prognosis |
|
Lymphoepithelial carcinoma |
Rare, predilection for Inuit in the Arctic regions, associated with Epstein–Barr virus |
|
Sialoblastoma |
Extremely rare, usually present at birth; mostly cured by surgical resection, preoperative biopsy needed |
Fig. 27.1 The cellular organization of the acinus and ducts of a normal salivary gland unit.
The current classifications of neoplasms are based on the ability of the neoplastic cell to mimic its cells of origin morphologically and functionally. In salivary gland neoplasms, two hypothetical possibilities have been suggested. Both theories strive to account for the vast heterogeneity shown by these neoplasms. The first theory, the multicellular theory, is that neoplasms are developed from adult differentiated counterparts of the salivary unit. Thus, acinic cell carcinomas would originate from acinar cells, oncocytic tumors from striated duct cells, squamous cell carcinomas and mucoepidermoid carcinomas from intercalated duct cells.
The second hypothesis is that neoplasms originate from the two undifferentiated types of reserve cell, the excretory duct reserve cell and the intercalated duct reserve cell. This is known as the “bicellular theory of origin.” Thus, adenoid cystic carcinoma morphologically resembles intercalated duct cells, and the bicellular theory of origin would account for the appearance of both ductal and myoepithelial cells through neoplastic transformation of the intercalated duct reserve cell. Squamous cell carcinoma and mucoepidermoid carcinoma arise from cells of the excretory duct reserve cell, as the cells of origin of salivary duct units carry the potential to keratinize because of their origin from surface epithelium. Warthin tumor and oncocytic neoplasms would arise from oncocytes, anywhere along the salivary unit or from the mature striated duct cells that they most closely mimic. Acinar (acinic) cell carcinoma arises from serous acinar cells and intercalated duct cells.
While these theories are comprehensible, it has been suggested that is no evidence to support the hypothesis of a semi-pluripotential bicellular reserve. It is currently proposed that all cell types are capable of replication and of being involved in tumorigenetic processes.5–9
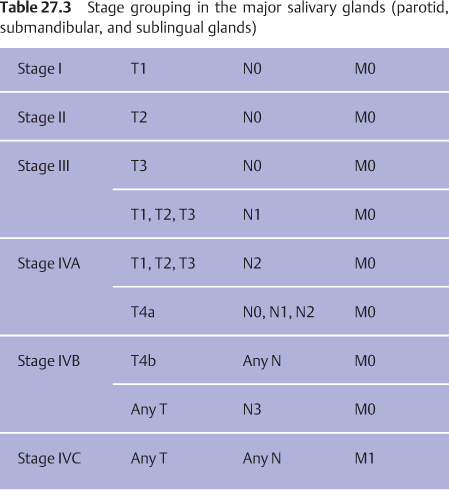
TNM and Stage Groupings
Recommendations have been made by the American Joint Committee on Cancer (AJCC) and the International Union on Cancer (UICC), and a primary tumor, regional nodes, and metastasis (TNM) classification and stage groupings have been published for salivary gland cancers. The classification only applies to carcinomas of the major salivary glands—the parotid, submandibular (submaxillary), and sublingual glands (Tables 27.2 and 27.3). Malignant tumors arising in minor salivary glands are staged according to the classification corresponding to the anatomic sites in which the tumor is located or diagnosed, with the TNM and stage groupings used for mucosal squamous cell carcinoma.10,11
Acinic Cell Carcinoma
Definition
Acinic cell carcinoma is a malignant epithelial neoplasm of the salivary glands in which at least some of the neoplastic cells show serous acinar cell differentiation, which is characterized by cytoplasmic zymogen secretory granules. Salivary ductal cells are also a component of this neoplasm. Synonyms: acinic cell adenocarcinoma, acinous cell carcinoma.
Epidemiology
More women than men are affected. All ages are affected, but there is an even distribution from the third to eighth decades of life. Eighty percent of the lesions occur in the parotid gland, 17% interorally in the minor salivary glands, and 4% in the submandibular gland.
|
T—primary site |
|
|
T1 |
Tumor 2 cm or less in largest dimension, without extraparenchymal extensiona |
|
T2 |
Tumor more than 2 cm but no more than 4 cm in largest dimension, without extraparenchymal extensiona |
|
T3 |
Tumor more than 4 cm and/or tumor with extraparenchymal extensiona |
|
T4a |
Tumor invades skin, mandible, ear canal, or facial nerve |
|
T4b |
Tumor invades base of skull, pterygoid plates, or encases carotid artery |
|
N—regional lymph nodes |
|
|
N0 |
No regional lymph-node metastasis |
|
N1 |
Metastasis in a single ipsilateral lymph node, 3 cm or less in largest diameter |
|
N2 |
Metastasis in a single ipsilateral lymph node, more than 3 cm but not more than 6 cm in largest dimension, or in multiple ipsilateral lymph nodes, none more than 6 cm in largest dimension, or in bilateral or contralateral lymph nodes, none more than 6 cm in largest dimension |
|
|
N2a Metastasis in a single ipsilateral lymph node, more than 3 cm but no more than 6 cm in largest dimension |
|
|
N2b Metastases in multiple ipsilateral lymph nodes, none more than 6 cm in largest dimension |
|
|
N2c Metastases in bilateral or contralateral lymph nodes, none more than 6 cm in largest dimension |
|
N3 |
Metastasis in a lymph node more than 6 cm in largest dimension |
|
M—distant metastasis |
|
|
MX |
Distant metastases cannot be assessed |
|
M0 |
No distant metastasis |
|
M1 |
Distant metastasis |
Clinical Features
The lesion presents as a slow-growing, solitary, unfixed mass in the parotid region. It may unusually present with pain or discomfort, and occasionally the patient may have a facial nerve weakness. The duration of symptoms and signs is commonly less than 12 months, although some may have been present for years. There is a predilection to metastasize to the cervical lymph nodes, and subsequently more distant sites, most frequently the lungs. Tumors in the submandibular gland are more aggressive than those in the parotid and minor salivary glands.
Staging is a better predictor of outcome than histomorphological grading. Most tumors are considered to be low-grade, but some behave aggressively and have a fatal course; the histological grading is therefore not considered to be useful as a prognostic indicator. Tumors that are large, involve the deep lobe of the parotid, and have nodal metastases, incomplete excision, and multiple recurrences are all associated with a poor prognosis.12,13
Prognosis and Predictive Factors
The average recurrence rate reported is 35%, and the incidence of metastasis and disease-associated death is about 16%.
Mucoepidermoid Carcinoma
Definition
Mucoepidermoid carcinoma is a malignant glandular epithelial neoplasm characterized by mucous, intermediate, and epidermoid cells, with columnar, clear cell, and oncocytoid features. Synonyms: mixed epidermoid and mucus-secreting carcinoma.
Epidemiology
Mucoepidermoid carcinoma is the most common primary salivary gland malignancy in both adults and children. It has a wide, nearly uniform age distribution, with lower rates in pediatric patients and the elderly. The mean age of the patients is about 45 years. There is a female predominance, and the lesion can arise in the major and minor salivary glands.
Clinical Features
Approximately 50% present in the major salivary glands—parotid 45% and submandibular 5%. The most frequent intraoral sites are the palate and buccal mucosa. Most tumors present as firm, fixed and painless swellings, some of which may have a cystic component. The tumor has an early likelihood of metastasizing to the cervical lymph nodes, locally initially and then more widespread.
Several systems of tumor grading have been proposed. Using five histopathological features—cystic component < 20%; neural invasion; necrosis; four or more mitoses per 10 high-powered fields; and anaplasia—may allow grading into low, intermediate, and high-grade lesions. In the submandibular gland, low-grade tumors tend to behave more aggressively.14,15
Prognosis and Predictive Factors
Most patients have a favorable outcome, as the majority of the lesions are low-grade or intermediate-grade tumors. High-grade tumors have an unfavorable outcome after surgery and radiotherapy.
Adenoid Cystic Carcinoma
Definition
Adenoid cystic carcinoma is a basaloid tumor consisting of epithelial cells in variable morphological configurations, including tubular, cribriform, and solid patterns.
Epidemiology
Adenoid cystic carcinoma represents approximately 10% of all epithelial salivary neoplasms and most frequently involves the parotid, submandibular, and minor salivary glands. These make up 30% of epithelial minor salivary gland tumors, with the highest frequency in the palate, followed by the tongue, buccal mucosa, lip, and floor of the mouth. The tumor occurs in all age groups, with a high frequency in middle-aged and older patients. There is no sex predilection, except for a high incidence in women of submandibular tumors.
Clinical Features
The most common symptom is a slow-growing mass, followed by pain due to the tumor’s propensity for perineural invasion. Facial nerve paralysis may also occur. The mass is solid and well-circumscribed but unencapsulated. The tumor consists of two main cell types: ductal and modified myoepithelial cells, which typically have hyper-chromatic, angular nuclei and frequently clear cytoplasm.
Tumor Patterns
There are three defined patterns: tubular, cribriform, and solid. Each of these forms can be observed as the dominant component, or more commonly as part of a composite tumor. Perineural invasion and to a lesser extent intraneural invasion are common and frequently conspicuous features of adenoid cystic carcinoma. Tumors can extend along nerves for a considerable distance beyond the clinically apparent boundaries of the tumor. Tumors may invade bone extensively before radiological evidence of osseous destruction appears. Adenoid cystic carcinoma occasionally occurs along with other, different neoplasms (hybrid tumors). Pleomorphic carcinomas and sarcomatoid transformation of adenoid cystic carcinoma have been reported, mostly in recurrent and metastatic disease.
Differential Diagnosis
Pleomorphic adenoma, polymorphous low-grade adenocarcinoma, basal cell adenoma, and adenocarcinoma and basaloid squamous carcinomas are the major entities to be differentiated.
Prognosis and Predictive Factors
Factors influencing survival include the histological patterns, tumor site, clinical stage, bone invasion, and status of the surgical margins. Generally, tumors composed of tubular and cribriform patterns follow a less aggressive course than those in which more than 30% of the lesion consists of solid components. Along with the histological pattern, the clinical staging substantially affects the prognosis. The 5-year survival is approximately 35%, but the long-term survival is poorer, and 80%–90% of patients die of the disease within 10–15 years. The local recurrence rate is in the range of 15%–85%. Recurrence is usually a sign of incurability.
Lymph-node involvement is uncommon but has been reported, typically with tumors of the submandibular gland and often due to contiguous spread rather than metastases. The incidence of distant metastases is estimated to be in the range of 25%–55%. The lungs, followed by bone, brain, and liver are the common sites. Wide local and radical surgical excision, with or without postoperative radiotherapy, is the treatment of choice. Radiation, alone or with chemotherapy, has shown limited success in the treatment of recurrent or metastatic disease. The value of chemotherapy in these tumors is limited and requires more investigation.16–20
Polymorphous Low-Grade Adenocarcinoma
Definition
The lesion is a malignant epithelial tumor characterized by cytologic uniformity, morphologic diversity, an infiltrative growth pattern, and low metastatic potential. Synonyms: terminal duct carcinoma, lobular carcinoma.
Epidemiology
Polymorphous low-grade adenocarcinoma is the second most common malignant intraoral tumor of the salivary glands, accounting for 26% of all carcinomas. There is a female preponderance of 2: 1. All ages are affected, but more than 70% of the patients are between the ages of 50 and 70 years.
Clinical Features
A painless mass in the palate is the most common presentation. Macroscopically, polymorphous low-grade adenocarcinomas usually appear as firm, circumscribed, but unencapsulated lesions, up to 2 cm in size. Intraoral lesions are the most common, but cases have also been reported in the parotid gland.
Tumor Patterns
Microscopically, the lesions demonstrate a variety of morphological configurations, differing both between tumors and within an individual tumor. The main microscopic patterns are: 1, lobular; 2, papillary or papillary–cystic; 3, cribriform areas, sometimes resembling those in adenoid cystic carcinoma; and 4, trabecular or small, ductlike structures lined with a single layer of cuboidal cells. This tumor is highly aggressive locally and is unencapsulated.21
Differential Diagnosis
Confusion between pleomorphic adenoma and adenoid cystic carcinoma may occur, especially when small biopsy specimens are presented. Most difficulties arise with minor salivary gland tumors. Use of special cytological tests helps confirm the diagnosis of polymorphous low-grade adenocarcinoma.
Prognosis and Predictive Factors
The overall prognosis is excellent. A recurrence rate of 10%–15% and a cervical metastasis rate of 10%–15% have been recorded; distant metastases have rarely been reported.21,22
Oncocytic Carcinoma
Definition
Oncocytic carcinoma is a proliferation of cytomorphologically malignant oncocytes and phenotypes with an adenocarcinomatous architecture, including infiltrative qualities. They may arise de novo, but are usually seen in association with a preexisting oncocytoma. A patient with an oncocytoma that has previously been classified as benign may subsequently present with cervical node metastases, and the lesion may then be retrospectively reclassified as originally malignant.
Clinical Features
Oncocytoma is uncommon and usually affects men, with mean age of 65 years. Eighty percent of the lesions affect the parotid gland and 8% the submandibular gland, with the rest being located the minor salivary glands. These tumors are considered to be high-grade and are characterized by multiple local recurrences and regional and distant metastasis.23,24
Salivary Duct Carcinoma
Definition
Salivary duct carcinoma is an aggressive adenocarcinoma that resembles high-grade ductal carcinoma in the breast. Synonyms: cribriform salivary carcinoma of the excretory ducts, high-grade salivary duct carcinoma.
Clinical Features
Salivary duct carcinoma is thought to be an uncommon salivary cancer. It has a male–female ratio of 4: 1, and the majority of lesions present in patients over the age of 50 years. The parotid gland is most commonly affected. The usual presentation is with rapid onset of a growing swelling, associated with pain and facial palsy. The tumor has a propensity to perineural spread, with intravascular tumor emboli. At presentation, the majority of patients are in an advanced stage of disease.
Differential Diagnosis
Malignancies to consider in the differential diagnosis include metastatic breast and squamous cell carcinomas, oncocytic carcinoma, and mucoepidermoid carcinoma.
Prognosis and Predictive Factors
Salivary duct carcinoma is one of the most aggressive salivary malignancies. More than a third of the patients develop local recurrences and just under 50% develop distant metastases. The sites of distant metastasis include the lungs, bones, liver, brain, and skin.25,26
Carcinoma Ex Pleomorphic Adenoma
Definition
Carcinoma ex pleomorphic adenoma is defined as a pleomorphic adenoma from which an epithelial malignancy is derived. Synonyms: carcinoma arising in a benign mixed tumor, carcinoma ex benign mixed tumor, carcinoma arising in a pleomorphic adenoma, malignant mixed tumor.
Clinical Features
Carcinoma ex pleomorphic adenoma represents about 3.6% of all salivary tumors, 12% of all salivary malignancies (range 2.8%–42.4%), and usually presents in the sixth to seventh decades of life. Many carcinomas ex pleomorphic adenoma probably result from the accumulation of genetic instabilities in a long-standing pleomorphic adenoma. They most frequently arise in the parotid gland, but all other salivary sites have been reportedly involved. The usual presentation is of a long-standing mass that has recently started to increase rapidly; the patient may or may not report pain and have facial palsy. The malignant component is most frequently a poorly differentiated adenocarcinoma or an undifferentiated carcinoma.
Tumor Patterns
Carcinoma ex pleomorphic adenoma can be subclassified into noninvasive, minimally invasive (< 1.5 mm penetration of the malignant component into extracapsular tissue) and invasive (> 1.5 mm of invasion from the tumor capsule into adjacent tissues). The first two groups usually have an excellent prognosis, while the latter has a more guarded prognosis. There is also a noninvasive carcinoma ex pleomorphic adenoma, also known as carcinoma in situ, intracapsular carcinoma ex pleomorphic adenoma, or pleomorphic adenoma with severe dysplastic changes.
Prognosis and Predictive Factors
Treatment is generally with wide local excision, including a neck dissection, followed by postoperative radiotherapy. As a group, invasive carcinomas ex pleomorphic adenoma are extremely aggressive, with 25%–50% of patients developing one or more recurrences. Some develop distant metastases, especially in the lung, bones (especially the spine), abdomen, and central nervous system. The size, grade, and clinical and pathological stage of the tumor are significant prognostic indicators. The overall survival at 3 years is about 40% and at 5 years 30%.27–30
Squamous Cell Carcinoma
Definition
Squamous cell carcinoma is a primary malignant epithelial tumor composed of epidermoid cells, which produce keratin and/or demonstrate intercellular bridges on light microscopy. It is essential to exclude the possibility of metastatic disease. Because of the unreliability of distinguishing minor salivary squamous carcinomas from other tumors of mucosal origin, the diagnosis is restricted to the major salivary glands.
Clinical Features
Primary squamous cell carcinoma probably represents less than 1% of salivary gland tumors. The majority present in the sixth to eighth decades of life, at a mean age of 60–65 years. Eighty percent arise in the parotid gland and 20% in the submandibular gland. Patients commonly present with a rapidly increasing, painful, firm, and fixed mass, not infrequently associated with a facial nerve weakness.31
Lymphoepithelial Carcinoma
Definition
Lymphoepithelial carcinoma is an undifferentiated carcinoma accompanied by a prominent nonneoplastic lymphoplasmacytic infiltrate. Synonyms: lymphoepithelioma-like carcinoma, malignant lymphoepithelial lesion, undifferentiated carcinoma with lymphoid stroma, undifferentiated carcinoma, carcinoma ex lymphoepithelial lesion.
Epidemiology
This is a rare salivary gland cancer, accounting for less than 1% of all salivary tumors. There is a strikingly high incidence among the Inuit in the Arctic regions (Greenland, Canada and Alaska), as well as among south-eastern Chinese and Japanese. There is a slight female preponderance, the parotid is more frequently involved, and the disease is at higher stages and apparently has a more aggressive clinical course in Inuits. There is a wide age range, from children to the elderly.32
Etiology
Almost 100% of salivary gland lymphoepithelial carcinomas in endemic areas are associated with Epstein–Barr virus (EBV).33
Clinical Features
The parotid is affected in 80% of the patients, followed by the submandibular gland, and rarely the minor salivary glands. Patients present with a change in size in a longstanding parotid or submandibular mass, with or without pain, and the tumor becomes fixed. Twenty percent of the patients have a facial palsy at presentation. Lymphoepithelial carcinoma has a propensity to spread to regional lymph nodes, with 20% of patients having distant metastases at the time of diagnosis.
Differential Diagnosis
The differential diagnosis includes metastatic undifferentiated carcinoma, malignant lymphoma, lymphoepithelial sialadenitis, lymphadenoma, and large cell undifferentiated carcinoma.
Prognosis and Predictive Factors
Five-year survival rates of 75%–85% have been reported in patients treated with surgery and radiotherapy. Local recurrences are possible. The prognosis depends on the tumor stage.
Other Rare Salivary Gland Malignancies
 Epithelial–Myoepithelial Carcinoma
Epithelial–Myoepithelial Carcinoma
Epithelial–myoepithelial carcinoma represents about 1% of salivary gland tumors. It occurs mostly in the parotid glands and minor oral salivary glands.34
 Clear Cell Carcinoma, Not Otherwise Specified
Clear Cell Carcinoma, Not Otherwise Specified
This is most frequently seen in the intraoral minor salivary glands. Middle-aged and older patients are affected. The prognosis is excellent.35
 Basal Cell Adenocarcinoma
Basal Cell Adenocarcinoma
Definition
Dominated by basaloid epithelial cells, basal cell adenocarcinoma is cytologically and histomorphologically similar to basal cell adenoma, but is an infiltrative epithelial neoplasm with a potential for metastasis. Synonyms: basaloid salivary carcinoma ex monomorphic adenoma, malignant basal cell adenoma, malignant basal cell tumor, and basal cell carcinoma.
Clinical Features
There is no sex predilection. The average age of patients is 60 years, and only adults are affected. More than 90% of the lesions are located in the parotid gland. They are locally destructive and often recur and metastasize locally.36
 Malignant Sebaceous Tumors
Malignant Sebaceous Tumors
Sebaceous Carcinoma
Sebaceous carcinoma is a malignant tumor composed of sebaceous cells of varying maturity that are arranged in sheets and/or nests, with different degrees of pleomorphism, nuclear atypia, and invasiveness. There is a bimodal age distribution, with peak incidences in the third decade and in the seventh to eighth decades of life. There is no sex predilection. Ninety percent of the lesions arise in the parotid gland, and patients present with a painful mass and varying degrees of facial paralysis. The treatment of choice is wide surgical excision for lesions in low stages and adjuvant radiotherapy for those in advanced stages. The 5-year survival is ≈ 60%.37
Sebaceous Lymphadenocarcinoma
Sebaceous lymphadenocarcinoma is the malignant counterpart of sebaceous lymphadenoma. Fewer than 10 cases have been reported to date.38
 Cystadenocarcinoma
Cystadenocarcinoma
This is characterized by predominantly cystic growth that often shows intraluminal papillary growth. The patients’ average age is 50 years, and the majority of lesions present in the parotid gland. The sublingual gland is proportionally more often involved than with other benign or malignant tumors. The buccal mucosa, lips, and palate are the most frequently involved minor gland sites. Surgery is the preferred treatment, with wide margins to minimize local recurrence. Nodal metastases have been reported.39
 Low-Grade Cribriform Cystadenocarcinoma
Low-Grade Cribriform Cystadenocarcinoma
This is a rare, cystic, proliferative carcinoma that resembles the range of breast lesions, from atypical ductal hyperplasia to micropapillary and cribriform low-grade ductal carcinoma in situ. The majority present in the parotid gland as cystic lesions, and they are seldom reported in the palate. They usually present in the elderly.40
 Mucinous Adenocarcinoma
Mucinous Adenocarcinoma
Mucinous adenocarcinoma is rare and usually presents in patients over the age of 50 years. It is usually seen in the palate, floor of mouth, submandibular gland, and lips, and has a propensity to recur locally and metastasize to lymph nodes.41
 Adenocarcinoma, Not Otherwise Specified
Adenocarcinoma, Not Otherwise Specified
This is an uncommon salivary cancer; the term should only be used when the tumor shows ductal differentiation but lacks any of the histomorphological features that characterize the other defined types of salivary carcinoma.
 Myoepithelial Carcinoma
Myoepithelial Carcinoma
Definition
Myoepithelial carcinoma of the salivary glands is a neoplasm composed almost exclusively of tumor cells with myoepithelial differentiation, characterized by infiltrative growth and with a potential for metastasis. These tumors represent the malignant counterpart of the benign myoepithelioma. Synonym: malignant myoepithelioma.
Clinical Features
The mean age at presentation is 55 years, but there is a wide range of age distribution. There is no sex predilection. The lesions represent less than 2% of all salivary gland carcinomas. More than 75% arise in the parotid gland, and they usually present as a painless mass, without local or distant metastasis at the time of presentation. These lesions may develop de novo, but many are reported to develop in preexisting pleomorphic adenomas or benign myoepitheliomas, particularly in recurrences.42,43
Prognosis and Predictive Factors
These are considered to be locally aggressive neoplasms. Approximately 33% of the patients die of the disease, a further third have recurrences, mostly multiple, and the remaining third of patients remain disease-free.
 Carcinosarcoma
Carcinosarcoma
This is a malignant tumor composed of a mixture of both carcinomatous and sarcomatous elements. It is extremely rare, with fewer than 50 cases reported. Sixty-six percent of the lesions arise in the parotid gland. Almost 60% of the patients die of local recurrence and/or distant metastasis, usually within 30 months.44
 Metastasizing Pleomorphic Adenoma
Metastasizing Pleomorphic Adenoma
Definition
Metastasizing pleomorphic adenoma is a histologically benign lesion that unexpectedly develops local and distant metastases. Synonyms: metastasizing benign mixed tumor, malignant mixed tumor.
Clinical Features
It is considered that multiple recurrences and surgical procedures allow some tumor to gain access to the venous circulation and metastasize. More than 75% of the lesions are in the parotid, some are in the submandibular gland, and there are also intraoral tumors. Forty percent of the patients die with the disease, 47% recover without disease, and 13% survive with disease.45,46
 Small Cell Carcinoma
Small Cell Carcinoma
This accounts for less than 1% of all salivary gland tumors and 2% of all salivary gland malignancies. Most patients are over the age of 50 years. Local recurrences are common. There is a very poor prognosis, with most patients dying with local or metastatic disease.47
 Large Cell Carcinoma
Large Cell Carcinoma
Large cell carcinoma is considered to be rare. Patients are aged over 60 years, and most present with a parotid mass, fixed, with metastatic nodes and facial palsy. The size of the tumors has been found to be a prognostic indicator. Synonyms: lymphoepithelioma-like carcinoma, malignant lymphoepithelial lesion, undifferentiated carcinoma with lymphoid stroma, undifferentiated carcinoma, carcinoma ex lymphoepithelial lesion.48
 Sialoblastoma
Sialoblastoma
Definition
This is a rare, potentially aggressive parotid or submandibular tumor that is usually present at birth. Synonyms: congenital basal cell adenoma, basal cell adenoma, basaloid adenocarcinoma, congenital hybrid basal cell adenoma–adenoid cystic carcinoma, embryoma.
Epidemiology
The condition is diagnosed at birth in most cases. Only 24 cases have been reported, with a male preponderance of 2: 1. The parotid is usually involved, but occasionally the submandibular gland.49
Prognosis and Predictive Factors
The tumor is usually cured by surgery, but it can potentially recur in 22% of cases and regional metastases are seen in 9%.
 A total of 24 malignant salivary gland neoplasms are currently described in the latest WHO classification.
A total of 24 malignant salivary gland neoplasms are currently described in the latest WHO classification.
 This diversity of neoplasms and other tumorlike lesions is unparalleled in any other organ system—making the surgical pathology of salivary gland neoplasms one of the more intimidating areas in diagnostic pathology. However, pathological analysis is considered essential for predicting the natural history of the various lesions and the likely prognosis.
This diversity of neoplasms and other tumorlike lesions is unparalleled in any other organ system—making the surgical pathology of salivary gland neoplasms one of the more intimidating areas in diagnostic pathology. However, pathological analysis is considered essential for predicting the natural history of the various lesions and the likely prognosis.
 While morphology continues to be the mainstay in the diagnosis of salivary tumors, immunohistochemistry is valuable for discerning the nature of poorly differentiated tumors involving the salivary glands (distinguishing between epithelial, lymphoid, and mesenchymal) and their origin (primary carcinoma or metastatic disease). It may also help differentiate the different types of clear cell tumor from one another.
While morphology continues to be the mainstay in the diagnosis of salivary tumors, immunohistochemistry is valuable for discerning the nature of poorly differentiated tumors involving the salivary glands (distinguishing between epithelial, lymphoid, and mesenchymal) and their origin (primary carcinoma or metastatic disease). It may also help differentiate the different types of clear cell tumor from one another.
 The majority of patients (60%–70%) will have one of four histological types: acinic cell carcinoma, adenoid cystic carcinoma, mucoepidermoid carcinoma, or polymorphous low-grade adenocarcinoma.
The majority of patients (60%–70%) will have one of four histological types: acinic cell carcinoma, adenoid cystic carcinoma, mucoepidermoid carcinoma, or polymorphous low-grade adenocarcinoma.
 Several tumors can be clinically classified as low-grade by their nature: acinic cell carcinoma, polymorphous low-grade carcinoma, and basal cell adenocarcinoma.
Several tumors can be clinically classified as low-grade by their nature: acinic cell carcinoma, polymorphous low-grade carcinoma, and basal cell adenocarcinoma.
 In contrast, several tumors are clinically high-grade: undifferentiated carcinoma; small cell, large cell, and lymphoepithelial carcinomas; oncocytic carcinoma; salivary duct carcinoma; carcinosarcoma; myoepithelial carcinoma; carcinoma ex pleomorphic adenoma; adenocarcinoma, not otherwise specified; and primary squamous cell carcinoma.
In contrast, several tumors are clinically high-grade: undifferentiated carcinoma; small cell, large cell, and lymphoepithelial carcinomas; oncocytic carcinoma; salivary duct carcinoma; carcinosarcoma; myoepithelial carcinoma; carcinoma ex pleomorphic adenoma; adenocarcinoma, not otherwise specified; and primary squamous cell carcinoma.
 Some malignant tumors vary in their aggressiveness, and methods have been suggested for distinguishing between high-grade and low-grade mucoepidermoid carcinomas and adenoid cystic carcinomas.
Some malignant tumors vary in their aggressiveness, and methods have been suggested for distinguishing between high-grade and low-grade mucoepidermoid carcinomas and adenoid cystic carcinomas.
 Some malignant salivary neoplasms have site predilections, such as the minor salivary gland (polymorphous low-grade adenocarcinoma, clear cell carcinoma, mucinous adenocarcinoma), whereas others have a predilection for specific age groups (sialoblastoma, usually diagnosed by age of 2; and basal cell adenocarcinoma, cystadenocarcinoma, myoepithelioma, and large cell carcinoma, affecting those over 50–60 years of age).
Some malignant salivary neoplasms have site predilections, such as the minor salivary gland (polymorphous low-grade adenocarcinoma, clear cell carcinoma, mucinous adenocarcinoma), whereas others have a predilection for specific age groups (sialoblastoma, usually diagnosed by age of 2; and basal cell adenocarcinoma, cystadenocarcinoma, myoepithelioma, and large cell carcinoma, affecting those over 50–60 years of age).
 The major points that should be included in all pathology reports are: (a) histological type; (b) anatomic site of origin; (c) documentation of the extent of the disease, to allow full TNM staging; and (d) documentation of the completeness of the surgical excision and margin status.
The major points that should be included in all pathology reports are: (a) histological type; (b) anatomic site of origin; (c) documentation of the extent of the disease, to allow full TNM staging; and (d) documentation of the completeness of the surgical excision and margin status.
< div class='tao-gold-member'>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses