Introduction
Many authors have examined the surgical bone treatment of cleft palate patients, but no study has emphasized the role of orthodontic therapy. The aims of this study were to evaluate the long-term stability of bone grafts when using an orthodontic-surgical protocol, to determine the success of bone grafts in minor vs severe clefts, and to develop a qualitative method for assessing the success of bone grafting.
Methods
Forty-nine patients were included in this study. Occlusal x-rays were taken before (T0), immediately after (T1), and at least 1 year after bone grafting (T2). Two radiographic parameters were analyzed adjacent to the cleft side: the vertical bone level (Bergland scale) and the horizontal bone level (Witherow-derived scale).
Results
The bone graft success at T2 was 91.84% (95% confidence interval, 84.55-96.41). The severity of the cleft before grafting was not statistically correlated with success at T2 ( P <0.05). The concordance rate between Bergland and Witherow values was 87.07% (95% confidence interval, 82.69-90.69). The variables analyzed (sex, age, type of cleft, lateral incisor agenesis) were not statistically correlated ( P <0.05) with the stability of bone graft. Based on the results, the only factor involved in the stability of the graft seems to be dental age at the time of bone grafting and the orthodontic therapy before and after grafting.
Conclusions
It seems appropriate to recommend early application of a surgical-orthodontic protocol to treat cleft lip and palate patients, prevent postoperative bone resorption, and guarantee correct positioning of the teeth.
Many studies have examined the surgical bone treatment of cleft palate patients; however, only a small number of these have addressed the long-term stability of the alveolar grafts.
There is a consensus among academic oral surgeons regarding the necessity of postponing bone grafting until the mixed dentition and then using a technique called “secondary bone grafting.” Boyne and Sands distinguished an “early” secondary bone grafting, usually performed between the ages of 2 and 5, and a “late” secondary bone grafting, usually after 5 years of age. This surgical technique has many advantages, including unified maxillary reconstruction and continuous alveolar formation, physiologic eruption of the teeth adjacent to the cleft, stabilization of cleft fragments, opportunity for a rapid expansion of the midline suture, elimination of oronasal fistulas, and overall facial esthetic improvements. However, all surgical and grafting procedures can cause growth alterations with bone dysplasias that are more severe when the procedure is performed early. For this reason, Kuijpers-Jagtman and Long concluded that a critical and customized case assessment is necessary to determine the risks and benefits of the procedure.
Despite the many studies on the outcomes after secondary bone grafting, they have significant limitations, including reported success rates of less than 100%, small sample sizes, inconsistent inclusion and exclusion criteria, incomplete and heterogeneous clinical records, limited follow-ups, and subjective methods for assessing the success of bone grafts.
Many factors are involved in the success of alveolar bone grafting. The first important factor is the canine position and its eruption stage at the time of bone grafting. Several studies have demonstrated that the success of bone grafts decreases if the procedure is performed after canine eruption on the cleft side. The second fundamental factor is the role of the therapy protocol and the orthodontic role, which have not been explored in the literature.
The aims of this study were to evaluate the long-term stability of bone grafts with an orthodontic-surgical protocol, to determine the success rate of bone grafts in minor vs severe clefts, and to develop a qualitative method for assessing the success of bone grafting.
Material and methods
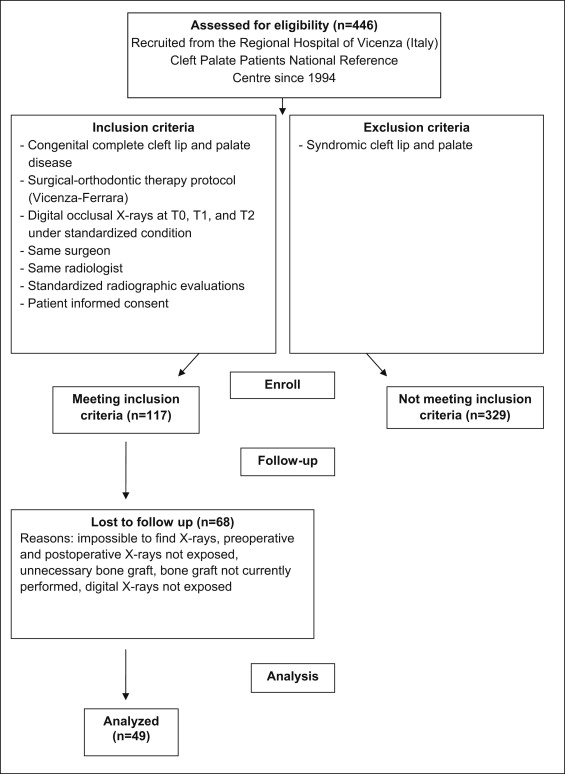
In this retrospective clinical trial, we analyzed the records of 446 complete cleft lip and palate patients, recruited from the Regional Hospital of Vicenza (Italy), Cleft Palate Patients National Reference Centre, between 1994 and 2011. There was only 1 data manager (D.T.), and all records were digitized. The study population consisted of white patients matched for sex and age.
Patients were included in the study based on the following criteria: (1) congenital complete cleft lip and palate; (2) treatment with the protocol of the Regional Hospital of Vicenza and the University of Ferrara; (3) digital occlusal radiographs before (T0), immediately after (T1), and at least 1 year after bone grafting (T2); (4) performance of the alveolar bone graft by the same surgeon; (5) digital occlusal x-rays exposed with a standardized radiologic technique (long-cone technique and root direction perpendicular to the palatine midline, compared with 2 other projections, to prevent radiologic superimpositions, image artefacts, and interpretation errors) by the same radiologist; (6) standardized radiographic evaluations; and (7) informed consent from each patient. Patients were excluded if they had syndromic cleft lip and palate. A total of 117 patients met all inclusion criteria. The study was double-blinded, and the statistical analysis was performed by an external statistician. Of the 117 patients who met the inclusion criteria, 68 were excluded for various reasons, leaving 49 patients in the study cohort ( Table I ). A flow chart of the study participants is shown in the Figure . Table II gives the sex distribution. There were 45 unilateral and 4 bilateral clefts. Among the 45 patients with unilateral clefts, 15 were right sided, and 30 were left sided. Thirty-two patients demonstrated lateral incisor agenesis, and 8 patients had agenesis of other teeth, contralateral to their clefts.
| Patients (n) | |
|---|---|
| Impossible to find radiographs | 5 |
| Preoperative radiographs not exposed | 10 |
| Postoperative radiographs not exposed | 22 |
| Bone graft unnecessary | 8 |
| Bone graft not currently performed | 5 |
| Digital radiographs not exposed | 18 |
| Patients excluded from study | 68 |
| Sex | n |
|---|---|
| Male | 33 |
| Female | 16 |
All patients had a surgical-orthodontic protocol in accordance with the Regional Hospital of Vicenza and the Postgraduate School of Orthodontics at the University of Ferrara in Italy. The chronologic order of the treatment, according to the protocol, is outlined below.
- 1.
At birth: placement of a passive palate plate, constructed of soft resin.
- 2.
At 3 months of age: soft-palate surgery and lip and nostril surgery with definitive lip repair.
- 3.
At 6 months of age: unilateral and bilateral rhinoplasty.
- 4.
At 8 to 12 months of age: initiation of speech therapy.
- 5.
At 18 to 20 months of age: hard palate surgery and continuation of speech therapy.
- 6.
At 5 years of age: placement of a hyrax-type rapid palatal expander bonded onto the deciduous teeth, with palatal and buccal arms reaching to the canines, activated at a quarter turn per day. The average activation period depended on the degree of maxillary constriction. A 2- to 3-mm overcorrection at the molars was recommended to counteract relapse. Immediately after the expansion, a maxillary traction device (Delaire mask) was applied with 450 g of force per side for 14 hours per day for 7 months. The rapid palatal expander was passively maintained in the mouth for 1 year after the expansion.
- 7.
At 6 to 9 years of age: placement of a passive transpalatal bar (0.036-in wire) bonded onto the first permanent molars (to prevent transverse relapse) and continuation of speech therapy.
- 8.
At 9 to 11 years of age: placement of an alveolar graft in the cleft side, using bone from the iliac crest, once canine root development was between one fourth and two thirds of its final root length as identified on the occlusal x-ray.
- 9.
At 9 to 15 years of age: orthodontic fixed therapy with preadjusted 0.022 × 0.028-in brackets to obtain alignment, leveling, malocclusion correction, and canine repositioning in the arch. Orthodontic therapy began when canine root development was between one fourth and two thirds of its final root length. Orthodontic appliances were kept in place through the transitional phase of the dentition until all teeth had erupted and definitive orthodontic treatment was completed, when all occlusal and functional goals of therapy were achieved.
- 10.
At 18 years of age: plastic (lip revision, nose revision, rhinoplasty, nasal septum surgery, adenoid surgery, sinus mucous membrane surgery, scar surgery) or maxillofacial surgery and implantation if necessary. In this study, no patient received jaw surgery, plastic surgery, or implantation.
Each patient had digital occlusal x-rays taken before the alveolar bone graft surgery (T0). The radiographs were taken using an AC Cefla dental machine with a CEI OXC 070G x-ray tube (Anthos, Imola, Italy). The machine was set at 65 kV and 7.5 mA. The focus-to-skin distance was 20 cm. Exposure time varied depending on the size of patient but was consistent for preoperative and postoperative x-rays and varied from 0.7, to 0.86, to 1.0 seconds. The film was oriented parallel to the occlusal plane, and the central beam was directed perpendicular to the cleft side for the first projection and at 70° to the film in the mesial and distal directions for the second and third projections. Then x-rays were processed with a dental vista scan machine (model 2130-51; Dürr Dental, Bietigheim-Bissingen, Germany) with DBSWIN software (Dürr Dental).
A numeric code was assigned to each patient before the evaluations to ensure blinding of the reviewers.
At T0, qualitative categorizations of cleft severity were made by using occlusal x-rays and based on the amount of bone support on each root adjacent to the cleft site. A standard for evaluation was adopted according to 2 scales: the Bergland vertical bone evaluation and the Witherow-derived horizontal bone evaluation. These scales are shown in Table III (types I, II, III, and IV and scores of 1, 0.5, and 0 were qualitative values used to indicate gradations in the presence or absence of bone). We compared each radiograph with its corresponding 2 other projections (the tube was directed at 70° to the film in the mesial and distal directions) to prevent image artefacts and interpretation errors. Two values were obtained for each cleft. The first value was related to the distal surface of the tooth on the mesial side of the cleft (site 1), and the second represented the mesial side of the tooth on the distal side of the cleft (site 2). In patients with bilateral clefts, both clefts were evaluated; however, only 1 value was recorded in the table because of identical results.
| Bergland scale | |
| Type I | Septal height approximately normal |
| Type II | Septal height at least three quarters of normal |
| Type III | Septal height less than three quarters of normal |
| Type IV | Absence of a continuous bony bridge |
| Witherow-derived scale | |
| Score 0 | No bone from the root surface to the midline of the cleft |
| Score 0.5 | Some bone but fails to reach the midline |
| Score 1 | Bone extends from the root surface to the midline |
All evaluations were performed by a blinded examiner (D.T.) and repeated 3 times on 3 different days, with a 30-day interval between evaluation sessions, to assess intraexaminer variability. Twelve randomly selected patients were assessed by 3 blinded and experienced examiners (U.B., A.G., G.S.) to evaluate interexaminer variability.
Based on the results, the patients were divided into the following groups ( Table IV ): (1) minor cleft: type I, score 1 or 0.5, on both teeth adjacent to the cleft; (2) moderate cleft: types II and III, score 0.5, on both teeth adjacent to the cleft; and (3) severe cleft: type IV, score 0, on both teeth adjacent to the cleft. Patients were also included in the gravest group if there was a different value on the roots adjacent to the cleft.
| Severity of cleft | n |
|---|---|
| Minor | 7 |
| Moderate | 30 |
| Severe | 12 |
| Total | 49 |
According to the protocol, an alveolar bone graft on the cleft side and an immediate postsurgical occlusal x-ray were performed on each patient. The patients were then examined monthly to monitor the orthodontic therapy. At T2, a long-term occlusal x-ray was obtained, and a qualitative evaluation of bone level was performed on the teeth adjacent to the cleft at T1 and T2. On 12 randomly selected patients, these evaluations were made by the first examiner and the 3 other examiners to evaluate interexaminer variability.
The first examiner obtained 294 values and repeated each measurement 3 times. The other 3 examiners obtained 216 values, resulting in a total of 1098 evaluations ( Tables V and VI ).
| I | II | III | IV | |
|---|---|---|---|---|
| T0 | 19 | 48 | 18 | 13 |
| T1 | 96 | 2 | 0 | 0 |
| T2 | 97 | 1 | 0 | 0 |
| 0 | 0.5 | 1 | |
|---|---|---|---|
| T0 | 13 | 85 | 0 |
| T1 | 0 | 12 | 86 |
| T2 | 0 | 8 | 90 |
By using this method, both of the following criteria had to be met for a successful outcome at T2: (1) vertical and horizontal bone values equal to or better than the bone values at T1; and (2) type I and score 1 (vertical and horizontal bone levels approximately normal), with bone support greater at T2 than at T0.
The patients’ records were reviewed for additional biometric data. Particular attention was paid to type of cleft (unilateral or bilateral); age at the 3 evaluation times; sex; any supernumerary teeth, diminutive lateral incisors, and peg-shaped lateral incisors in the cleft area; any supernumerary or diminutive teeth not in the cleft area; absence of any teeth adjacent to the cleft and the probable cause thereof; and the incidence of regrafting.
The average age at the time of bone grafting was 10.25 years, with a range of 8 to 14.7 years ( Table VII ). The average age at follow-up was 12.16 years, with a range of 10.1 to 15.6 years. The average time of follow-up after grafting was 1.87 years, with a range of 1 to 4.8 years ( Table VIII ).
| Average age (y) | SD | n | Minimum | Maximum | Median |
|---|---|---|---|---|---|
| 10.25 | 1.21 | 49 | 8.00 | 14.70 | 10.00 |
| Average (y) | SD | n | Minimum | Maximum | Median |
|---|---|---|---|---|---|
| 1.87 | 1.10 | 49 | 1.00 | 4.80 | 1.30 |
At T2, 38 patients (77.55%; 95% confidence interval [CI], 63.38-88.23) had not experienced canine eruption, and 11 patients (22.44%; 95% CI, 11.77-36.62) had canine impaction requiring a surgical flap and orthodontic recovery.
Statistical analysis
The percentage of bone graft success was calculated at T1 and T2. To evaluate whether the severity of the defect was correlated to the success of bone grafting at T2, the results were subjected to the nonparametric chi-square test. To evaluate whether the Bergland scale was comparable with the Witherow-derived scale, the Kendall coefficient of concordance was used (0 < Kendall W <1). The Kendall W expresses the level of agreement of multiple assessments from the same or different operators. This coefficient is a real number between 0 (no agreement) and 1 (full agreement). A Kendall W less than 0.7 indicates little agreement and that the measurement method can lead to inaccurate results, whereas a Kendall W greater than 0.9 indicates strong agreement and that the results are likely to be accurate.
We calculated the Kendall coefficient of concordance (0 < Kendall W < 1) to control for intraexaminer and interexaminer repeatability and reproducibility.
In addition, we evaluated several variables to determine whether they had statistically significant effects on the long-term stability of the bone grafts at T2. (1) The potential effects of sex and age (at bone grafting) were analyzed by using a linear regression analysis, which is an approach to modeling the relationship between a scalar variable Y and at least 1 variable called X. Proceeding to the statistical analysis, the patients were further divided into those who were 10 years or younger and those older than 10 years, in accordance with sample medians equal to 10 years old ( P <0.05). (2) The effects of type of cleft (unilateral or bilateral) were assessed by using a binomial test ( P <0.05). This determines the statistical significance of the deviations from the expected and the observed distributions into 2 categories. (3) Lateral incisor agenesis was also assessed by using a binomial test ( P <0.05). (4) Finally, we used the Wilcoxon signed rank test to determine the surgical success rates ( P <0.05). This is a nonparametric statistical hypothesis test used to assess whether population means differ when comparing 2 related samples or repeated measurements of 1 sample. It is useful in evaluations of ordinal-scale variables.
The chi-square test ( P <0.05) was used to verify the correlation between the severity of the cleft palate at T0 and any lost teeth adjacent to the cleft at T2, and whether site 1 had a different Bergland value than site 2 at any of the 3 measurement times. A binomial test ( P <0.05) was used to evaluate whether lateral incisor agenesis at T0 was correlated with the spontaneous eruption of the canines at T2, and whether there was an association between the type of cleft at T0 and any lost teeth adjacent to the cleft at T2.
The statistical analysis was performed with the R 2.12 × 64 software (copyright 1998-2012 by Kurt Hornik), and the statistical significance level was set at 95% ( P <0.05).
Results
Success rate and grading systems
The success rate at T1 was 70.41% (95% CI, 60.34-79.21). The success rate at T2 was 91.84% (95% CI, 84.55-96.41). The binomial intervals of confidence did not intersect; therefore, the T2 success rate was significantly greater than that at T1.
The correlation between cleft palate severity and success rate at T2 was not statistically significant ( P = 0.64).
The Kendall coefficient of concordance was 0.99 for both the Bergland and the Witherow-derived scales (0 < Kendall W < 1), indicating that these scales were comparable.
It was acceptable to use the Kendall W because the concordance rate between the Bergland and Witherow-derived values was 87.07% (95% CI, 82.69-90.69), and the error method was not relevant.
Table IX shows the cross-tabulation of the Bergland and Witherow-derived evaluations by first operator and first evaluation. It highlights the error point in which 37 type I Bergland values were classified as a Witherow-derived score of 0.5.
| Type | 0 | 0.5 | 1 |
|---|---|---|---|
| I | 0 | 37 | 175 |
| II | 0 | 50 | 1 |
| III | 0 | 18 | 0 |
| IV | 13 | 0 | 0 |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


