Chapter 38 Lateral pharyngoplasty
1 INTRODUCTION
We call lateral pharyngoplasty (LP) the surgical splint of the lateral pharyngeal walls, achieved by turning the superior pharyngeal constrictor muscles (SPC) into dilating flaps. The lateral pharyngeal muscular walls are thickened and exceedingly collapsible during respiration in patients with obstructive sleep apnea/hypopnea syndrome, causing narrowing of the pharynx. The SPC muscles envelop all the collapsible segment of the pharynx and form the outer pharyngeal muscular layer.
3 SURGICAL TECHNIQUE
The procedure is performed with the patient under general anesthesia, using a mouth gag with a long tongue blade to give adequate exposure (Fig. 38.1). We use 4.0 Vicryl for all sutures. LP is performed as a stand-alone treatment for snoring and sleep apnea. When the patient needs nasal surgery to improve nasal breathing, this can be done in combination with LP. Fourteen per cent of our cases were treated with both LP and nasal surgery together.
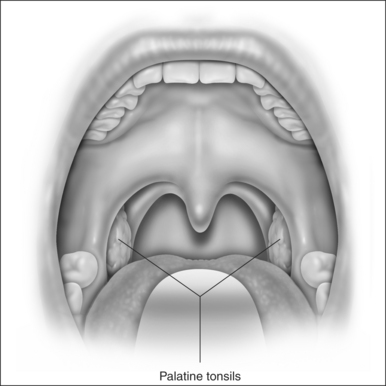
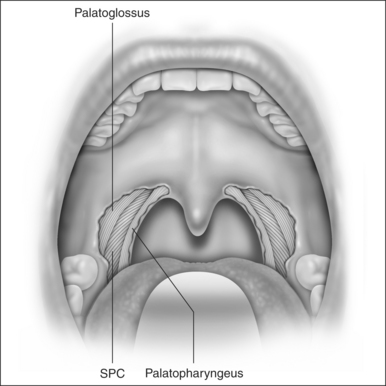
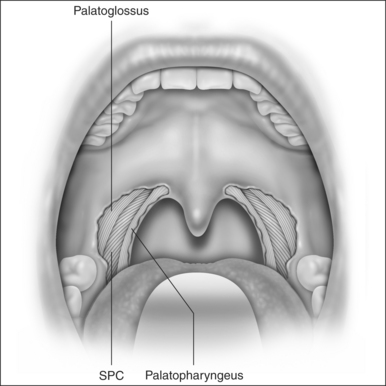
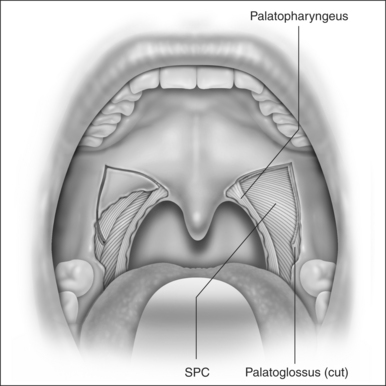
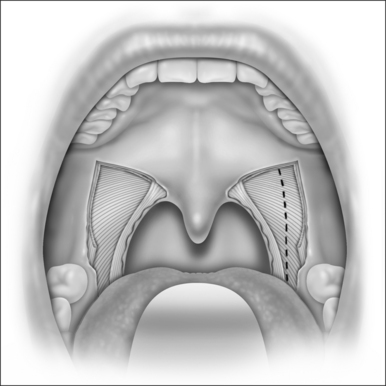
LP starts with a bilateral tonsillectomy (Fig. 38.2). If that has already been done, we undermine and remove the tonsillar fossa lining until we can identify the palatoglossus and palatopharyngeus muscles. Next, with an upside down ‘V-shape’ incision (Fig. 38.3), we remove a triangle of mucosa and muscle (palatoglossus) from the lateral oral free margin of the soft palate and anterior pillar.That provides a wide exposure of the SPC muscle, including its pterygopharyngeal (partially), buccopharyngeal and mylopharyngeal parts (Figs 38.4 and 38.5). The height of this incision corresponds to that reached by the lateral superior traction (see Fig. 38.10) of the upper part of the palatopharyngeus muscle, which will be used to close this wound.
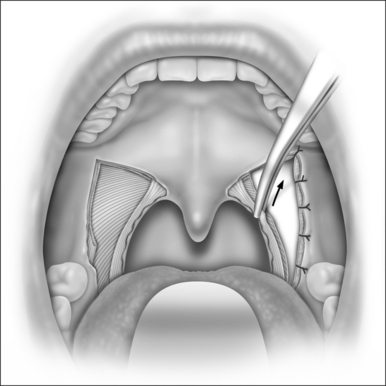
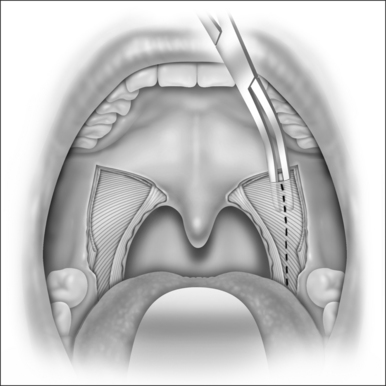
Once fully exposed, we undermine and elevate the SPC muscle from the peripharyngeal space (Fig. 38.6), starting from its most cranial visible part, and separate it from its fascia (buccopharyngeal fascia). It is very important to preserve this fascia, avoiding injury to cranial nerves IX and X and to other pharyngeal muscles, which could delay swallowing recovery. The SPC muscle is elevated from the pharyngeal wall in its posterior but not lateral aspect, near the palatopharyngeus muscle, since this region has fewer blood vessels, and once you reach the right plane of dissection there, the muscle can be easily detached from its fascia. Usually, the vertical fibers of the palatopharyngeus muscle have to be pulled medially at the start of the dissection, to expose better the horizontal fibers of the SPC. Once detached, we cauterize the SPC with a bipolar and section its fibers in a cranial to caudal direction (Fig. 38.7). We keep this dissection near the palatopharyngeus, using this muscle as a guide to avoid injuring vessels and nerves at the lateropharyngeal space. This dissection extends as far as the caudal end of the SPC muscle (glossopharyngeal part, where it originates from the side of the tongue). To accomplish this, we have to create a submucosal tunnel inferiorly to the tonsillar fossa to preserve and separate the mucosa from the SPC muscle that is being sectioned. This usually extends from 1 to 1.6 cm beyond the tonsillar fossa, depending on the anatomy, and relates to the retroglossal area.
< div class='tao-gold-member'>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses