Fig. 1.1
The three major salivary glands (a) parotid gland, (b) submandibular gland, and (c) sublingual gland with their nerve innervation are highlighted (Reprinted with permission from Holsinger and Bui [2])
Whole saliva is mostly made of water (99.5 %) and other functional components such proteins, enzymes, electrolytes, and smaller organic molecules as described in Table 1.1 [4]. At least 40 proteins have been identified in salivary secretions, and most of these are identified in helping maintain the integrity of teeth against a constant barrage of physical, chemical, and microbial trauma. In addition to these proteins and lipids, salivary electrolytes and organic molecules like urea and glucose are also important elements of the oral defense system. The interaction among these components is essential in maintaining a balanced and healthy oral environment [5].
Table 1.1
The composition of saliva
|
Composition of saliva
|
|
|---|---|
|
Proteins:
|
Albumin; amylase; β(beta)-glucuronidase, carbohydrates; cystatins; epidermal growth factor; esterases; fibronectin; gustin; histatins; immunoglobulin A, G, and M; kallikrein; lactate dehydrogenase; lactoferrin; lipase; lysozyme; mucins; nerve growth factor; parotid aggregins; peptidases; phosphatases, proline-rich proteins; ribonucleases; salivary peroxidases; secretory component; secretory IgA; serum proteins; tyrosine-rich proteins; vitamin-binding proteins
|
|
Enzymes
|
|
|
Glycoprotein
|
|
|
Peptides
|
|
|
Small organic molecules
|
Creatinine, glucose, lipids, nitrogen, sialic acid, urea, uric acid
|
|
Electrolytes
|
Ammonia, bicarbonate, calcium, chloride, fluoride, iodide, magnesium, phosphates, potassium, nonspecific buffers, sodium, sulfates, thiocyanate
|
The protein-rich secretions of the salivary glands contain a milieu of antibacterial enzymes, immunoglobulins, lubricants, inorganic elements, and incredibly high numbers of bacteria (108–109 bacteria per ml of saliva). That being said, saliva continues to be the tooth’s first defense against cariogenic pathogens [5]. Salivary function can be divided mainly into three major areas: (1) protective, (2) food related, and (3) communication/speech. The salivary components involved in the “protective” function of saliva are described in Table 1.2 [4].
Table 1.2
The salivary components involved in the “protective” function of saliva
|
Function: protective
|
Salivary components involved
|
|---|---|
|
Lubrication
|
Water, mucins, proline-rich glycoproteins coat surfaces of oral mucosa, throat, and food
|
|
Antibacterial, antifungal, antiviral
|
Salivary proteins (e.g., lysozyme, lactoferrin, lactoperoxidase, mucins): histatins, cystatins, secretory IgA, proline-rich glycoproteins
|
|
Mucosal integrity
|
Mucins, electrolytes, water
|
|
Lavage, cleansing
|
Water
|
|
Buffering capacity
|
Bicarbonate and phosphate, proteins
|
|
Remineralization
|
Calcium, phosphate, proline-rich glycoproteins
|
Protective
Saliva protects and lubricates oral cavity. Mucins, produced mainly by the submandibular and sublingual secretory cells, are the lubricant component of saliva [6, 7]. Mucins control the permeability of mucosal surfaces, by creating a salivary film that is able to limit the penetration of various potential irritants and toxins in foods and beverages, as well as hazardous agents such as tobacco smoke. Furthermore, mucins, in combination with electrolytes and water, act as a natural “water proofing” agent that helps maintain the oral tissues in a hydrated state thus preserving its mucosal integrity. Saliva also contains antifungal and antiviral systems, such as secreting antibodies (secretory IgA), directly involved in neutralizing viruses [8]. Consequently, water, IgA, and proline provide a constant oral “cleansing” or “lavage” function. This physical flow of saliva continuously removes potentially harmful bacteria. Next, bicarbonate and phosphate ions and proteins assist in the achievement of oral homeostasis and the maintenance of a specific pH by buffering extreme oral acids and bases. Teeth are remineralized through the deposition of calcium, phosphorus, and statherin (a calcium-binding protein) [9].
Food-Related and Communication
Another important function of saliva is its contribution to the initial phase of digestion (Table 1.3) [4]. The salivary glands provide lubricatory molecules that coat food and the soft and hard tissues of the oral cavity. Lubrication allows food to travel easily through the digestive system and provides smooth tissue surfaces with minimal friction. Without lubrication, food becomes impacted around teeth, making eating difficult and unpleasant, and it also contributes to plaque formation. Saliva enhances taste and swallowing as well. The presence of saliva is critical in stimulating chemical sensations on taste buds [10]. During mastication, the salivary flow intensifies, which in turn stimulates taste receptors and augments the diffusion and chemical interaction between food particles and the associated taste buds. Saliva, as a result, is a fundamental factor in maintaining optimal nutritional status. Moreover, the lubrication from water and mucins assists in the ability to speak and makes verbal communicate possible [11].
Table 1.3
The salivary components involved in the “food-related and communication” functions of saliva
|
Salivary components involved
|
|
|---|---|
|
Function: food related
|
|
|
Preparation for digestion
|
Water, mucins, proline-rich glycoproteins
|
|
Digestion
|
Amylase, ribonuclease, lipase
|
|
Mucosal integrity
|
Mucins, electrolytes, water
|
|
Taste
|
Water, gustin (zinc-binding salivary protein)
|
|
Function: communication
|
|
|
Speech
|
Water, mucins
|
Gross Anatomy of the Salivary Glands
The Parotid Gland
The parotid gland, the largest of the salivary glands, weighs approximately 15–30 g and is 6 × 4 cm in dimensions. The parotid gland is located bilaterally on each side of the face in front of the ears and extends to the lower borders of the mandible. Each gland is covered by fibrous connective tissue capsule that secretes serous fluid, a watery and protein-rich solution. The parotid gland is shaped like an inverted pyramid. It is positioned inferior to the zygomatic arch, anteroinferior to the external acoustic meatus, anterior to the mastoid process, and posterior to the ramus of the mandible (Fig. 1.2). The gland is divided into a base, an apex, and lateral, anterior, and posterior surfaces. Its laterosurface is situated right below the skin and superficial fascia of the head. The anterior surface of the gland is grooved by the ramus of the mandible and masseter muscle (from this depression the maxillary artery leaves the gland). The posterior surface is grooved by the mastoid process, the sternocleidomastoid muscle, and styloid process. From this site, the external carotid and the facial nerve enter the gland. The apex of the gland is located between the angle of the mandible and the sternocleidomastoid muscle. From this area, the retromandibular vein and the facial nerve leave the gland [12] (Fig. 1.2).
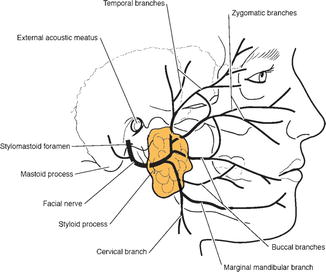
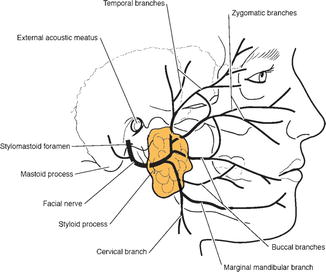
Fig. 1.2
Lateral view of the parotid gland and its nerve supply (Adapted with permission from Holsinger and Bui [2])
The parotid gland has a large duct (Stensen’s duct) that crosses the masseter muscle and opens near the upper second molar in the oral cavity (Fig. 1.3). Blood supply is provided by the terminal branches of external carotid artery (ECA). The facial nerve and its branches form an important landmark, dividing the parotid into superficial and deep lobes. The main sensory nerve within this gland is the auriculotemporal nerve (Fig. 1.2). Secretomotor supply to the parotid is derived from the glossopharyngeal nerve (IX), via the tympanic branch, tympanic plexus, lesser petrosal nerve, and the pterygopalatine ganglion. The parotid contains superficial lymph nodes in its superior lobe. These nodes drain deeply to the deep cervical nodes or superficially to the superficial cervical nodes [6].
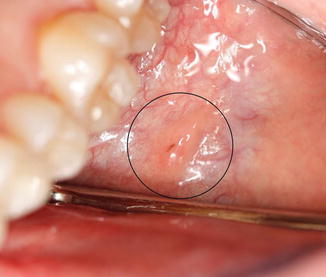
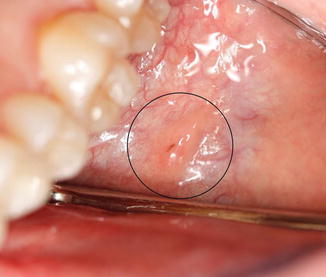
Fig. 1.3
The orifice of the Stensen’s duct of the parotid gland located near the second maxillary molar
The Submandibular Gland
The submandibular gland is approximately half of the weight (7–10 g) and size (4–5 cm) of the parotid gland. This gland is also encapsulated, but there is no fibrous connective tissue. The submandibular gland is located in the submandibular triangle formed by the anterior and posterior bellies of the digastric muscle and the inferior margin of the mandible (Fig. 1.1b). The gland present three surfaces: lateral (connected to medial surface of the mandible), medial (connected to the mylohyoid, hyoglossus, and digastric muscles), and inferior (shielded by the skin and platysma muscle). The gland is divided into superficial and deep lobes, the latter being the majority part of the gland. The deep lobe projects from the mylohyoid and hyoglossus muscles. The submandibular duct, also referred to as Wharton’s duct, exits from the deep part of the gland adjacent to the mandibular second molar and ascends anteriorly to the floor of the mouth (Fig. 1.4). As the duct exits the gland, it lies inferior to the lingual nerve. The blood supply originates from the facial and lingual artery and submental and facial veins. The innervation of this gland relies on submandibular ganglion and lingual nerve located superiorly to the deep process of the gland (Fig. 1.1) [2, 6, 12].
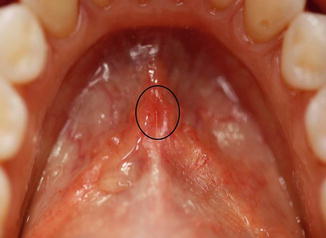
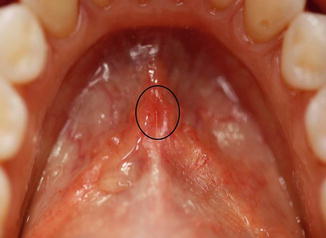
Fig. 1.4
The orifices of the Wharton’s ducts are located on anterior part of the floor of the mouth
The Sublingual Gland
The sublingual gland is the smallest of the major salivary glands. It is almond shaped and is located underneath the mucous membrane of the floor of the mouth between the mandible and genioglossus muscle (Fig. 1.1c). The sublingual gland is not covered by a fascial capsule. This gland has approximately 8–20 small ducts (the ducts of Rivinus), which exit the superior aspect of the gland and open along the sublingual fold on the floor of the mouth. Occasionally, several of these ducts may join to form a common duct (the duct of Bartholin), which typically empties into the Wharton’s duct. The secretions from sublingual and submandibular glands flow through this duct and excrete into the floor of the mouth below the tongue. The sublingual and submental arteries are the main source of circulation in this salivary gland. The lingual, the chorda tympani, and the sympathetic nerves are responsible for its innervation (Fig. 1.1) [2, 6, 12].
Minor Salivary Glands
The minor salivary glands are widely distributed throughout the oral mucosa, palate, uvula, floor of the mouth, posterior tongue, retromolar and peritonsillar area, pharynx, larynx, and paranasal sinuses. There are hundreds (600–1,000) of these small glands ranging in size from 1 to 5 mm (Fig. 1.5). Unlike the major glands, the minor glands present a single duct that secretes directly into the oral cavity. These glands can secrete serous, mucous, or mixed saliva. Additionally, minor salivary glands may be found at the superior pole of the tonsils (Weber’s glands) and at the base of the tongue (von Ebner’s glands). Parasympathetic innervation is derived from the lingual nerve, except for the minor glands of the palate, which receive their parasympathetic fibers from the palatine nerves, fed by the sphenopalatine ganglion.


Fig. 1.5
The minor salivary glands within the circle
Histology of the Salivary Glands
The major salivary glands consist of a main excretory duct, which drains into the oral cavity on one side, and on the reverse side it branches into series of smaller ducts (progressively lesser in diameter) referred to as striated, intercalated, and finally into even tinier ones termed intercellular canaliculi [2, 6, 13]. These highly divided branches terminate into globular secretory end pieces known as acini (Fig. 1.6).
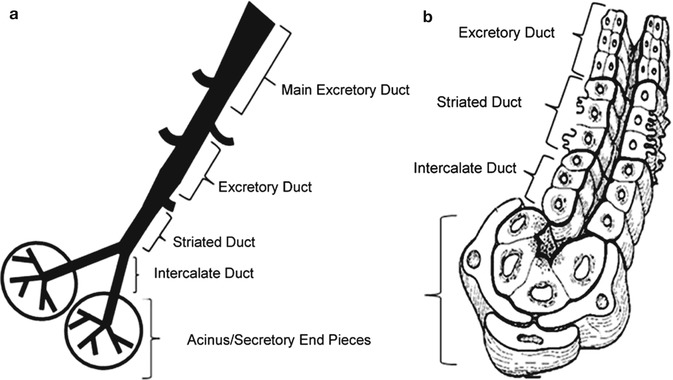
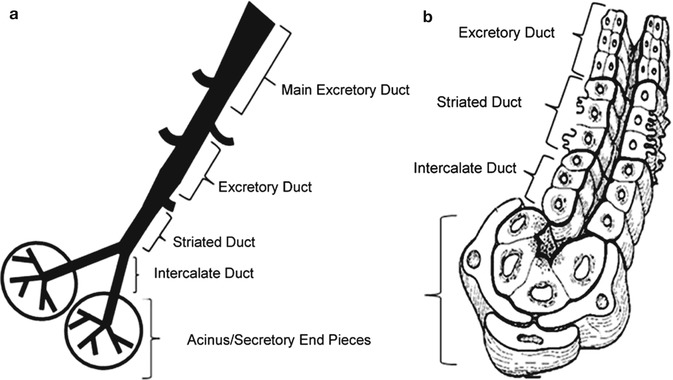
Fig. 1.6
(a) Ductal system of the salivary gland, (b) A cross-sectional view of different cells which make up the ductal system. The rough caricature illustrates the emergence of smaller ducts to larger ones and eventually to the main excretory duct which opens into the oral cavity (Adapted with permission from Holsinger and Bui [2])
The end pieces may contain the two leading types of secretory cells: serous and mucous. Serous cells produce water and protein-rich content, whereas mucous cells produce mucin. This subcomponent of mucus is viscous; thus, it coats and protects mucosal surfaces. Salivary glands are supported by connective tissue, which house the nerve, vascular, and lymphatic supplies (Fig. 1.7). Parotid glands are mostly composed of serous cells, while the submandibular and sublingual glands are mixed glands of both serous and mucous cells (Figs. 1.7 and 1.8) [2, 6, 13].
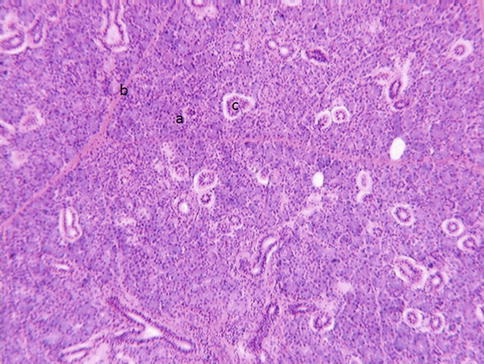
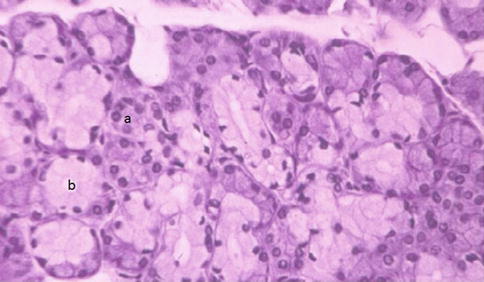
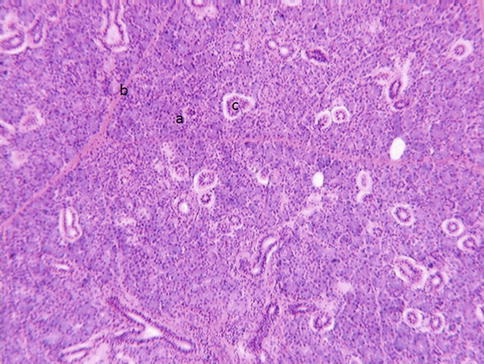
Fig. 1.7
Parotid gland contains serous producing cells (a). Connective tissue septum separates each lobule (b). Intralobular ducts (c) transport primary saliva from secretory end pieces to the main excretory ducts and eventually to the oral cavity
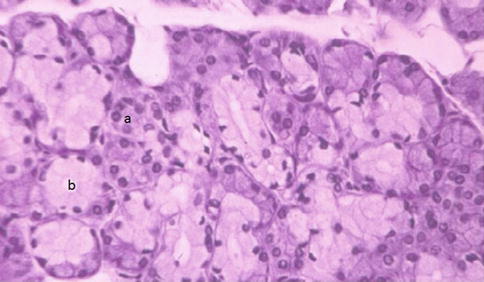
Fig. 1.8
Submandibular gland contains both serous- (a) and mucous (b)-secreting cells
Salivary Secretory End Pieces
In parotid glands, secretory end pieces present themselves as an encapsulated spherical structure with 8–12 of only serous cells (Fig. 1.9). Each of these cells is pyramidal in shape: the broad base is adjacent to the connective tissue called stroma, while its narrow apex faces the central lumen (Fig. 1.9). The submandibular gland has similar secretory end pieces; however, it contains both mucous- and serous-secreting cells (Fig. 1.10). Mucous cells form the main lining of these submandibular gland secretory acini, while a group of serous-secreting cells lie on the periphery and are referred to as serous demilune (Fig. 1.11) [5, 6].
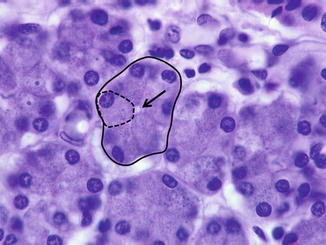

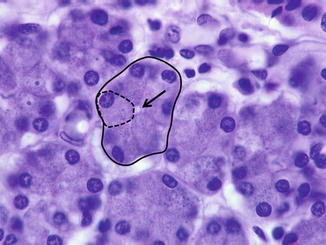
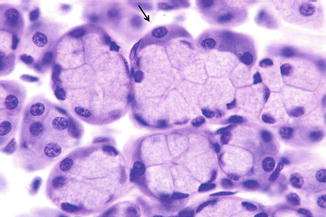
Fig. 1.9
Parotid secretory end pieces (solid circle) are globular structures with 8–12 serous cells and an associated lumen (arrow). The dashed lines highlight one serous cell

Fig. 1.10
Submandibular and sublingual glands’ secretory end pieces are made of few mucous cells arranged in a spherical unit, called acinus (dotted line)
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses