This article describes the concepts of treating a complex aesthetic interdisciplinary case in a traditional approach.
Key points
- •
Communication is important to achieve the ultimate perio-restorative interface.
- •
Facial aesthetic design was used to aid in the development of an aesthetic blueprint, so that soft and hard tissue discrepancies could be eliminated to improve the restorative aesthetic outcome and minimize patients’ facial asymmetry.
- •
The team approach is essential in achieving ideal aesthetics for an interdisciplinary treatment plan.
- •
When communication occurs properly, the aesthetic surgery can be considered a surgical component of the restorative therapy.
Background
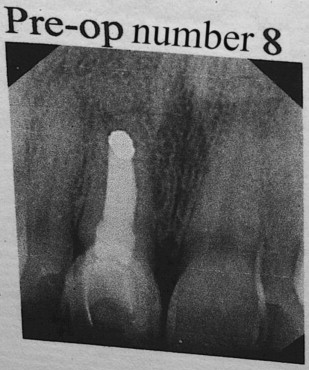
A 40-year-old female patient presented to our office with a chief complaint of pain above the upper right central incisor. Her medical history was noncontributory. On radiographic examination it was determined than an endodontic failure existed including periapical pathology and a buccal fistula ( Fig. 1 ). Full mouth charting revealed a stable periodontal status with a localized 8-mm midfacial probing approximating the apex of tooth number 8. Dental examination revealed porcelain laminate veneers on teeth numbers 4 to 13, which had been placed approximately 14 years prior.
Background
A 40-year-old female patient presented to our office with a chief complaint of pain above the upper right central incisor. Her medical history was noncontributory. On radiographic examination it was determined than an endodontic failure existed including periapical pathology and a buccal fistula ( Fig. 1 ). Full mouth charting revealed a stable periodontal status with a localized 8-mm midfacial probing approximating the apex of tooth number 8. Dental examination revealed porcelain laminate veneers on teeth numbers 4 to 13, which had been placed approximately 14 years prior.
Aesthetic evaluation
Traditionally we evaluate patients from the facial perspective, then the smile perspective. Finally, we evaluate individual tooth anatomy for proper aesthetics. Before comprehensive evaluation and esthetic treatment planning, we took digital photographs per the American Academy of Cosmetic Dentistry’s guidelines, and we also took a full mouth series of x-rays, made study models, and performed intraoral charting.
Facial
The patient’s facial form is dolichocephalic on visual examination ( Fig. 2 ). Both the bridge of the nose and the chin favor the patient’s left side. The lower third of the face is the dominant third.

Smile
The patient has existing maxillary veneers from the second premolar to the second premolar ( Fig. 3 ). At a full smile the patient shows excessive gingival display with a canting from right to left of the midline ( Fig. 4 ). More gingival tissue is shown on the patient’s right side than on the left as well as a canting of the existing veneers 4 to 8 to the patient’s left. Asymmetrical tissue heights exist both from right of midline to left. Additionally, an asymmetry in tissue height is present between the maxillary centrals. The gingival margin on 8 is approximately 1.5 mm apical to the margin on tooth 9. Convexities appear to be present in the buccal corridor apical to the gingival margins of teeth 3 to 5 and 12 to 14.


Tooth
The narrowness of the patient’s facial features dictated that the teeth, especially the central incisors, not be made any longer ( Fig. 5 ). However, the angularity of the patient’s facial features made it desirable to keep the angular anatomy in the teeth.

Periodontal considerations
The patient had a chronic endodontic failure of tooth 8, with an existing buccal fistula. From a periodontal perspective, there was minimal overall probing depth except for a localized deep midfacial probing depth on tooth 8 indicating no midfacial bone was present. Although the interproximal bone appeared intact radiographically, there was an existing gingival discrepancy between teeth 8 and 9, with the gingival margin of 8 approximately 1.5 mm apical to 9 ( Fig. 6 ). A high smile line existed with associated excessive gingival display from tooth 3 to tooth 8 and tooth 10 to tooth 14. The gingival position of 9 was determined to be ideal in relation to facial aesthetic design and the patient’s interpupillary line.

Treatment plan
The treatment planning for this case required close coordination between restorative and periodontal specialists. Scheduling was critical as the patient would be traveling between two offices during some of the procedures.
The initial treatment plan called for an extraction of the upper right central incisor and an attempt at immediate placement of the implant along with any tissue augmentation that would be required for site development. At the same visit a 2-unit bis-acryl temporary bridge, retained by the left central incisor, would be fabricated. Any additional site development could then be done by removing and adding or subtracting from the provisional. The patient would ultimately require hard and soft tissue crown lengthening, restoration of the upper 10 anteriors (4-7 and 10-13) with porcelain veneers, an implant crown on 8, and a porcelain jacket on 9.
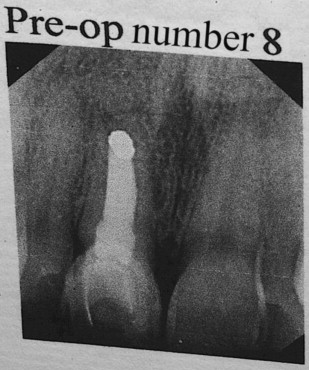
Surgical Treatment
Extraction of 8, implant placement, and temporary bridge
A facial and palatal sulcular incision was performed, and tooth 8 was extracted. A severe facial dehiscence was present approximating the apex of the socket ( Fig. 7 ). An immediate implant (Biomet 3i, NanoTite, 5 × 13 mm; Palm Beach Gardens, FL) was stabilized in the residual socket, and demineralized freeze-dried bone allograft (DFDBA; LifeNet Tissue Bank, Virginia Beach, Virginia) was used to fill the gap and augment the facial dehiscence. A thick subepithelial connective tissue graft was used instead of a membrane to augment the soft tissue, improve primary closure, and attempt vertical augmentation that would decrease the existing gingival discrepancy ( Fig. 8 ).
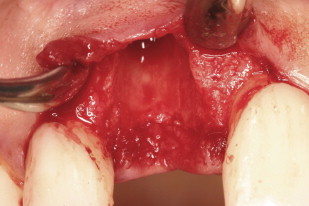
The patient then went to the restorative dentist’s office for provisionalization. A two-unit cantilever bridge was used with tooth 9 as the abutment. The patient was anesthetized again with 1 carpule of articaine hydrochloride and epinephrine (Septocaine). The existing veneer on tooth 9 was removed carefully so as not to disturb the surgical site. The preparation was continued for a porcelain jacket, with removal of 1.5 mm circumferentially and 1.5 incisally, and scooping out of the lingual surface for prosthetic clearance in the bite ( Fig. 9 ).

Glycerin was then applied lightly to the area; Luxatemp (DMG America, Englewood, NJ) was injected into the initial mold of the patient’s teeth, seated in the mouth for 2 minutes, and gently pulled out. Any excess material was cleaned from the area. The material was allowed a full 4 minutes to set, then removed and shaped outside the mouth ( Fig. 10 ). Care was taken not to put pressure on the pontic site. The mesial aspect of teeth 7 and 9 was sounded to find the crest of bone. Contact points were created roughly 4.5 to 5.0 mm long to ensure papillary regeneration. The bridge was then polished and cemented with TempBond Clear (Kerr Corporation, Orange, CA); excess cement was removed, and the bite was checked ( Fig. 11 ).





