Fig. 8.1
Patient with a tooth extraction performed 1 year earlier. The focused panoramic view well demonstrates a persistent alveolar socket related to delayed socket healing (*). Note also the increased thickening of the alveolar lamina dura (arrowheads) and alveolar crest (arrow), as an early finding of osteonecrosis of the jaw (ONJ)
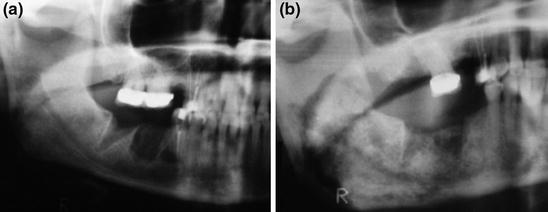
Fig. 8.2
Follow-up panoramic radiograph in a patient who underwent a tooth extraction. a Panoramic radiograph 1 month after extraction. b Panoramic radiograph 1 year after extraction. Delayed healing of the socket is readily visible in a comparison of the two images. Note also the thickened and disorganized medullary trabeculation, with cortical thickening and a typical “cotton-wool’’ appearance
Several authors have described bone sclerosis as the most common finding: its appearance can range between subtle thickening of the lamina dura and alveolar crest (Fig. 8.1) to attenuated osteopetrosis-like sclerosis [4, 9, 10]. In advanced stages, osteonecrosis is seen as an irregular area of osteosclerosis with “a cotton wool-like’’ appearance (Fig. 8.2b). Osteolyses often show a central sequestrum; lytic areas may also indicate foci of bacterial infection (Fig. 8.3) [4, 5, 9].


Fig. 8.3
Panoramic radiograph in a patient with ONJ showing a very large osteolytic area with central bone sequestrum (arrow)
Periosteal reaction and bone sequestrum may be predominant in advanced stages of the disease (Fig. 8.4) [7, 9]. Pathologic fractures are a common finding, with one study showing fractures in 16 of 32 patients with ONJ [4, 5, 7, 9]. Narrowing of the marrow space and involvement of the inferior alveolar canal are also common findings at CT (Fig. 8.5) [4, 5, 9]. However, it was recently demonstrated that even if adjacent alveolar bone is altered by lytic or sclerotic changes, sparing of the mandibular canal may represent the diagnostic clue for malignancies [11, 12]. CT is a useful imaging modality to demonstrate both the size and the type of alveolar involvement, to precisely assess the dimensions and locations of the lesions, and to define lesion margins during management (Fig. 8.6) [11, 12]. If the maxilla is involved, there may be associated abnormalities in the adjacent maxillary sinus, from muco-periosteal thickening to air-fluid levels and purulent drainage (Fig. 8.7) [9, 11, 12].
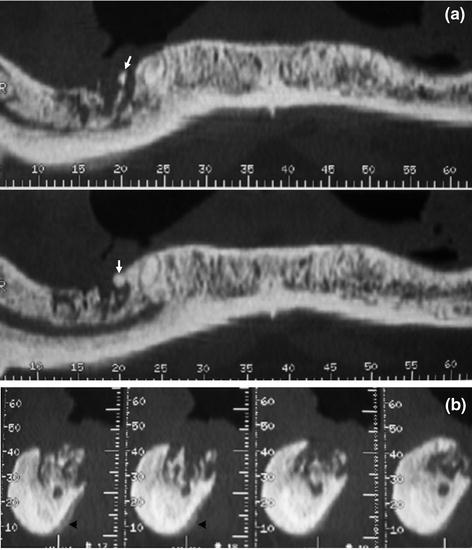

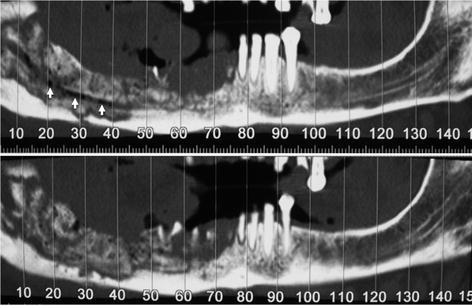
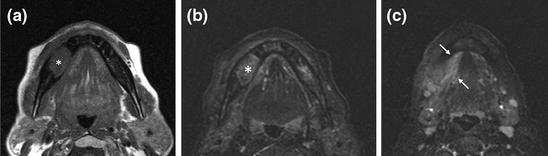
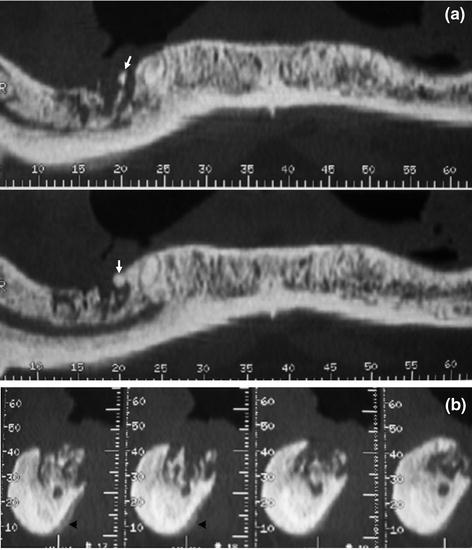
Fig. 8.4
CT Denta-scan. a Panoramic view shows lytic lesion in the right mandible with small sclerotic bone sequestra (arrows). b A thick and regular periosteal reaction (arrowheads) is well demonstrated on a cross-sectional image series

Fig. 8.5
Panoramic radiograph shows a wide osteolytic area involving the mandibular canal (arrows)
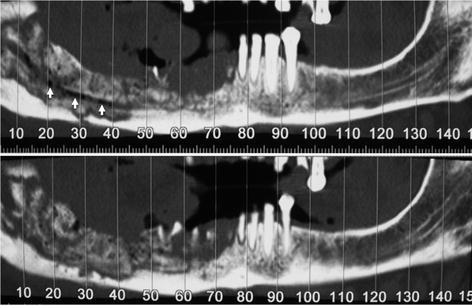
Fig. 8.6
CT Denta-scan. Two different panoramic views show the extensive involvement of the right mandible and the presence of both osteolytic and sclerotic foci, determining a mottled or “cotton-wool’’ appearance. Note also the involvement of the mandibular canal, evidenced by several small air bubbles in its content (arrows)
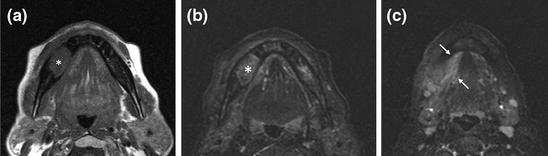
Fig. 8.7
MRI in a patient with ONJ-related osteonecrosis. a T1-weighted axial MRI shows a large hypointense lesion (*) involving the right mandible. b On axial STIR, the osteonecrotic focus is mildly hyperintense. c More caudal STIR MRI shows extensive involvement of the periosseous soft tissues
8.3 Magnetic Resonance Imaging
In most cases, MRI is not used in the evaluation of a patient in whom ONJ is suspected, especially if the disease is in the early stage. However, as is the case with CT, disease extent is better demonstrated on MRI in the context of the clinical evaluation [9, 11–13]. The primary role of MRI is to assess the degree of bone and soft-tissue involvement, which may be helpful in planning surgical debridement in intractable cases not responding to conservative treatment [9, 14–16]. The signal-intensity changes on MRI encompass the bone and adjacent soft tissues, with variable signal-intensity abnormalities on T1- and T2-weighted images.
Typical ONJ findings on MRI are a decreased signal intensity on T1-weighted images and intermediate/high signal intensity on T2-weighted and/or short tau inversion-recovery (STIR) images, suggestive of edema and inflammation (Fig. 8.7a, b), with a variable degree of enhancement after the administration of contrast medium. Signal-intensity changes may be restricted to the cortex or extend to the bone marrow, adjacent soft tissues (Fig. 8.7c), maxillary sinus, and inferior alveolar canal [9, 13–16]. In cases of soft-tissue involvement, there is increased soft-tissue signal intensity on T2-weighted images (Fig. 8.7c) [9, 13–16]. However, signal-intensity changes on T2-weighted images and contrast enhancement findings may show enormous variability, due to fatty marrow replacement, bone sclerosis, or sequestrum [9, 13–18].
After gadolinium administration, the changes in signal intensity may be more extensive, suggesting greater disease extent than determined from the CT appearance of the involved bone (Fig. 8.8) [9, 13–16]. Bone marrow enhancement correlates with both the degree of fatty marrow replacement and a decrease in signal intensity on T1-weighted images [4] and typically spares the low T2 signal of the bone sequestrum [9, 13–18]. Soft-tissue enhancement is variable and may involve the mylohyoid ridge, buccinator muscle, orbicular muscle, maxillary sinus, and masticator space and muscles (Fig. 8.8) [9, 13–18]. There may be a focal mass-like thickening of these muscles, which clinically may mimic neoplastic involvement [19–21].
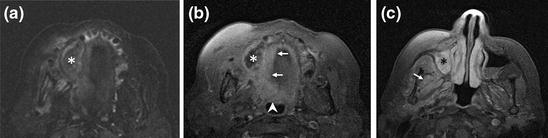
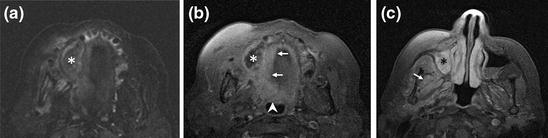
Fig. 8.8
MRI in a patient with maxillary osteonecrosis. a Axial STIR shows large osteonecrotic involvement (*) of the right maxillary bone. b Fat-suppressed T1-weighted axial MRI after gadolinium administration shows mild and diffuse enhancement around the osteonecrotic lesion (*) with involvement of the soft palate (arrows) and oropharyngeal wall (arrowhead). c More cranial fat-suppressed T1-weighted axial MRI after gadolinium administration shows thickening and enhancement of the maxillary sinus mucosa (*) as well as mild enhancement of the pterygoid muscles (arrow)
To date, only a few reports have described the MRI features of early-stage ONJ. According to Bisdas et al. [4], in early cases in which there are open wound areas and mild symptoms, decreased signal intensity on T1-weighted images is associated with intermediate or slightly increased signal intensity on T2-weighted images. At the periphery of wound lesions, there is usually a decrease in signal intensity on T2-weighted images [9].
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


