Fig. 12.1
Clinical features of stage I BIONJ in areas in the proximity of dental implants. This 64-year-old woman with osteoporosis had been treated with alendronate for 9 years

Fig. 12.2
Vaporization of necrotic bone using an Er:YAG laser (non-contact mode)
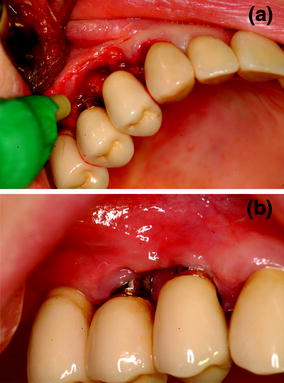
Fig. 12.3
a Biostimulation of the surgical area using low-level laser therapy (Nd:Yag laser). b At 3-weeks follow-up, there is complete clinical healing

Fig. 12.4
Stage I BIONJ of the lower jaw in an area of chronic trauma associated with complete denture wearing. This 67-year-old woman with breast cancer and bone metastases had been treated with zoledronate for 8 months

Fig. 12.5
Stage I BIONJ of the maxilla in the same patient as in Fig. 12.4
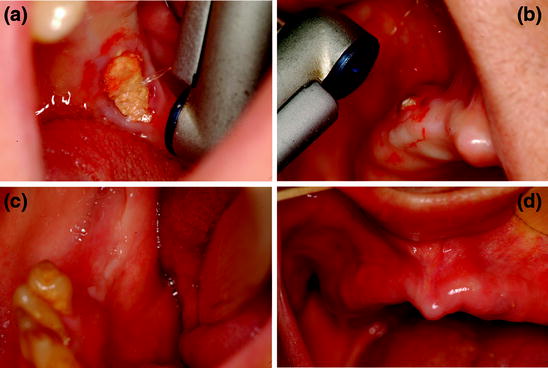
Fig. 12.6
a Vaporization of mandibular necrotic bone through Er:YAG laser (non-contact mode). b Vaporization of maxillary necrotic bone using Er:YAG laser. c At 1-month follow-up, there is complete mucosal healing of the mandibular treated site in shown in (a). d At 1-month follow-up, there is complete mucosal healing of the maxillary treated site shown in (b)
An evaluation of the peripheral bone damage induced by the different cutting systems demonstrated that all sections obtained with Er:YAG laser were better than those obtained by piezosurgery, high-speed drill, and low-speed drill. Er:YAG laser resulted in poor peripheral carbonization with a regular incision without a residual bone smear layer [34]. The erbium laser technique enables resection of the bones of the upper and lower jaw affected by BIONJ and can be performed using local anesthesia (Figs. 12.7, 12.8, 12.9, 12.10). Surgical debridement is also possible, with gradual evaporation of the necrotic bone at depths increasingly close to healthy bone. The minimally invasive technique of evaporation allows the sectioned bone surfaces to be made regular and the creation of micro-perforations at the base for renewed vascularization [35]. In our experience, BIONJ sites were treated with Er:YAG laser at very short pulses (VSP mode: pulse duration of 100 μs) and at a setting of 300 mJ, 30 Hz and 60 J/cm² of fluence; the laser device was used in non-contact or near-contact mode. Clinical success was obtained in cancer and non-cancer patients for 97% of BIONJ sites, with a complete mucosal healing in 90% of the cases for an average period of 13 months of follow up [36, 37]. Other authors reported similar results with laser surgery [38, 39].
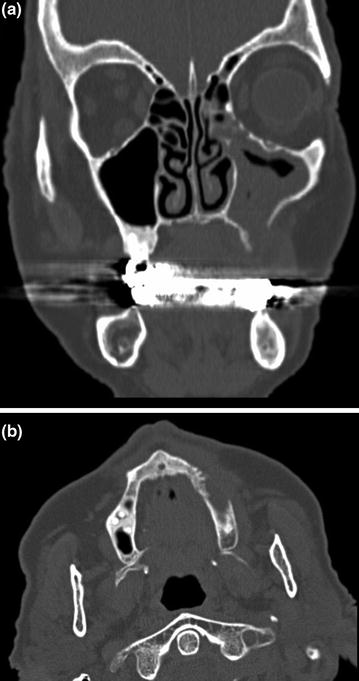

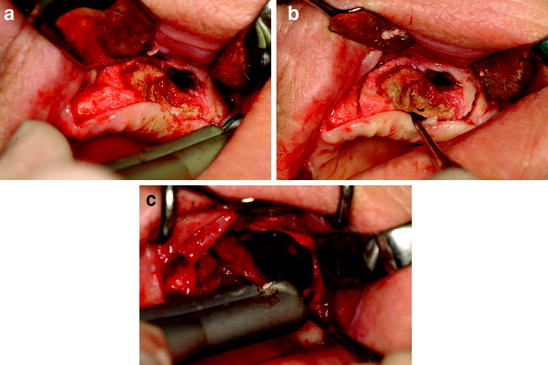
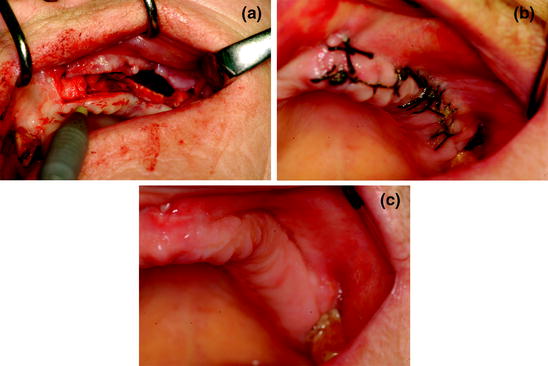
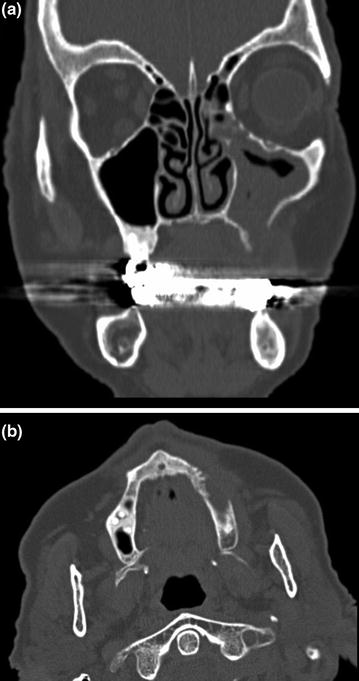
Fig. 12.7
a Computed tomography scan of the maxillofacial region, with radiographic evidence of involvement of the left maxillary sinus (stage III BIONJ) in a 72-year-old woman with osteoporosis and rheumatoid arthritis who had been treated with corticosteroids and alendronate for 10 years. b Computed tomography scan of the maxillofacial region, with radiographic evidence of bone necrosis in the patient described in (a)

Fig. 12.8
Clinical features of maxillary BIONJ (same patient as in Fig. 12.7)
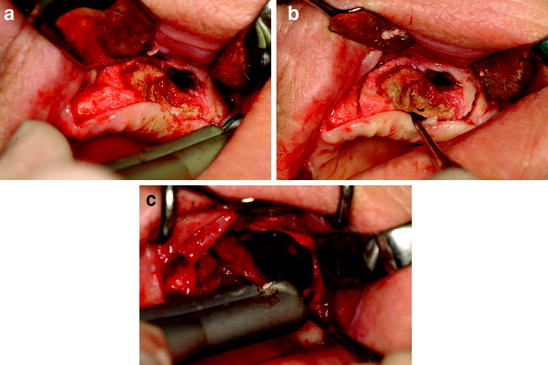
Fig. 12.9
a Clinical aspect of necrotic bone after surgical flap opening. b Surgical resection of necrotic bone and surrounding apparently healthy tissue with Er:YAG laser. c Er:YAG laser vaporization of the bone margins
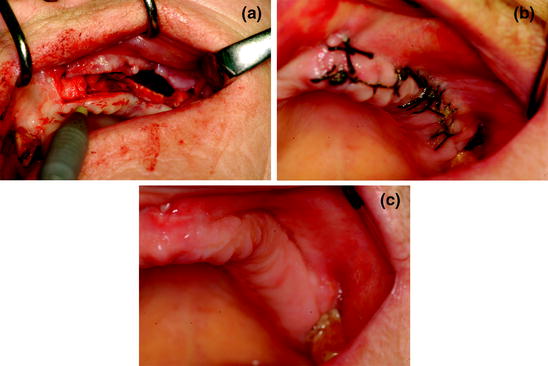
Fig. 12.10
a Biostimulation of the surgical area using low-level laser therapy (Nd:Yag laser). b At 1-week follow-up. c At 1-month follow-up, there is complete mucosal healing
12.4 Laser and Preventive Measures
Many expert panels have developed various documents on preventive strategies. These documents are aimed at specialists involved in the multidisciplinary management of BIONJ patients. Dental surgical procedures (tooth extractions, bone remodeling of severe exostoses, endodontic surgery) and urgent periodontal treatment (scaling and root planing) should be completed before the commencement of bisphosphonate therapy.
Surgical trauma is a recognized predisposing factor to BIONJ development, although there are also significant percentages of spontaneous forms, as reported in the literature [40]. Tooth extractions and oral surgical interventions should thus be avoided (unless urgently necessary) because they increase the risk of BIONJ, by about eight-fold in both cancer and non-cancer patients [41] When a surgical procedure becomes unavoidable, antibiotic treatment with amoxicillin (2 g/day) 3 days prior to and 2 weeks after the intervention must be prescribed [42]. Laser treatment for bactericidal as well as biostimulatory effects can improve the outcome of dental invasive procedures by inducing bone and mucosal healing (Figs. 12.11, 12.12, 12.13) [43, 44].




Fig. 12.11
Clinical features of stage II BIONJ in a 66-year-old periodontopathic patient with multiple myeloma who had been treated with zoledronate for 9 months

Fig. 12.12
Teeth extraction, vaporization, and decontamination of bone using an Er:YAG laser (non-contact mode)

Fig. 12.13
a Biostimulation of the surgical area using low-level laser therapy (Nd:Yag laser). b At 2-months follow-up, there is complete mucosal healing of the site shown in (a)
12.5 Conclusions
Despite the many reports in the literature, optimal BIONJ therapy remains an unresolved issue and there are no evidence-based guidelines. The current discussion revolves around two opposite approaches: invasive versus non-invasive treatment. Regardless of the chosen strategy, the main objectives of treatment are to alleviate pain, reduce infection, stabilize disease progression, and, of course, obtain closure of the exposed bone.
Antibiotic therapy represents a non-invasive, valid solution to manage the symptoms of BIONJ, but the long-term results regarding complete mucosal healing are worse than those obtained through a surgical approach. However, the elderly or cancer patients may be debilitated by their malignancy, chemotherapy, or comorbidities and thus unable to tolerate the side effects of prolonged therapeutic antibiotic schedules. In these cases, LLLT (associated with medical therapy) may be more beneficial in the treatment of BIONJ lesions, especially when surgery is not an option. The diffuse forms of BIONJ require extensive bone resection after a careful evaluation of the patient’s general conditions, including disease evolution, age, performance status, and life expectancy. However, a review of the literature showed less satisfactory results for stage III lesions than for lower stages. Based on this result, patients with minimal bone exposure should be considered as candidates for conservative surgical strategies.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


