This case report describes the treatment of a 33-year-old white man who had a skeletal Class III and dental Class II subdivision malocclusion caused by a retrognathic maxilla, with severe maxillary crowding, a highly placed maxillary left canine, mild mandibular crowding, and a bilateral posterior crossbite. Treatment was performed with a modified surgery-first approach, which included a short presurgical alignment phase for the correction of the significant maxillary crowding while controlling the incisal angulation, followed by LeFort I maxillary advancement surgery. The short presurgical orthodontic phase aimed at eliminating the anterior dental interferences before the maxillary advancement, and the use of the inherent increased bone turnover in the postsurgical phase helped to reduce the total orthodontic treatment time to 12 months. Pleasing esthetic results and a good functional occlusion were achieved.
Highlights
- •
Surgery-first is a new option to expedite treatment for orthognathic surgical patients.
- •
This approach is impossible in some patients because of occlusal interferences.
- •
We present a presurgical orthodontic phase to selectively eliminate anterior dental interferences.
- •
Significant crowding was resolved with temprorary anchorage devices to control maxillary incisor inclinations.
- •
This approach can be an alternative to reduce total treatment time in orthognathic surgery.
Presurgical orthodontic treatment has been found to be the most time-consuming stage for patients undergoing orthognathic surgery. This phase can vary widely from 7 to 47 months. A long period of presurgical orthodontic movement usually does not help the patient’s chief complaint, which often is a facial deformity. Presurgical orthodontic treatment accentuates the skeletal deformity and further antagonizes the patient, who desires his or her facial esthetics to be normal.
Recently, there has been much interest in shortening the total treatment time for patients undergoing combined orthodontic and orthognathic surgical treatment. Using the surgery-first approach, many authors have demonstrated a reduction of up to 50% in the total treatment time. The surgery-first approach can be used to treat a variety of malocclusions with different degrees of complexity. Certain criteria, such as mildly crowded anterior teeth, a flat to mildly accentuated curve of Spee, normal to slightly proclined or retroclined incisors, and minimal transverse discrepancies, are ideal for a surgery-first approach. In contrast to conventional orthodontic-orthognathic surgery, the presurgical occlusal relationship in a surgery-first approach often does not reflect the true underlying skeletal discrepancy. In such cases, obtaining near-normal inclination of the maxillary and mandibular incisors with respect to their basal bones before surgery becomes particularly important if the maxillomandibular complex is to be positioned optimally without compromising the surgical results.
A contraindication for the surgery-first approach is found when the planned postsurgical occlusion results in an interference between the anterior teeth, precluding a stable occlusion. In these patients, presurgical orthodontic treatment is required to eliminate these interferences. However, the goal of this presurgical phase is only to eliminate this interference without extending treatment to achieve full leveled and aligned arches. This can be considered a modified surgery-first approach, where the arches are set up to achieve a transitional Class I malocclusion (Class II molar relationship if the maxillary premolars are extracted) after surgery. Hence, the presurgical phase is dramatically reduced, usually limited to 6 months.
This case report demonstrates how the total treatment time can be reduced by combining a limited presurgical orthodontic phase for the correction of maxillary crowding while controlling the maxillary incisors’ inclination with a modified surgery-first approach. This short orthodontic presurgical phase also eliminates the anterior interferences to obtain a stable occlusion after surgery.
Diagnosis and etiology
A 33-year-old white man came to the orthodontic clinic at the University of Connecticut complaining that he wanted his bite fixed. His medical history was noncontributory, and the temporomandibular joint examination was normal, with no mandibular shift.
The pretreatment facial examination showed a concave soft tissue profile ( Fig 1 ). The ratio of lower anterior facial height to upper anterior facial height, and the ratio of lower facial height to throat depth, were within normal limits. The nasolabial angle was obtuse, and both upper and lower lips were retrusive with respect to the E-line. No interlabial gap was present at rest. Increased buccal corridor spaces and 60% occlusogingival length of the maxillary incisors were visible upon smiling. The maxillary and mandibular dental midlines were coincident with the facial midline.
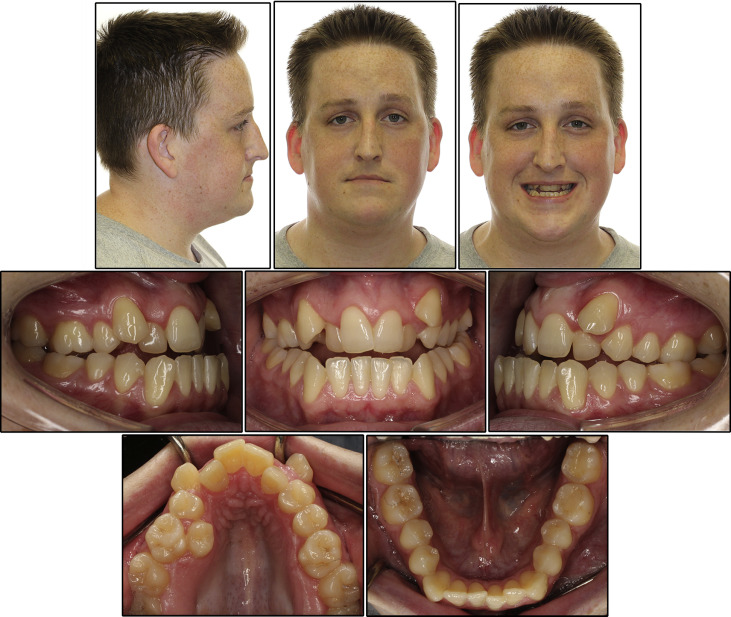
The intraoral examination showed that the patient had a full complement of teeth ( Figs 1 and 2 ). The molar relationships were Class I on the left side and Class II on the right side ( Fig 2 ). The maxillary arch was constricted transversely, resulting in a crossbite from first molar to first molar and 18 mm of crowding. The maxillary left canine and right second premolar were ectopically placed. The mandibular dental arch had mild crowding of 4 mm. He had a negative overbite of −2 mm and a negative overjet of −3 mm ( Fig 2 ).
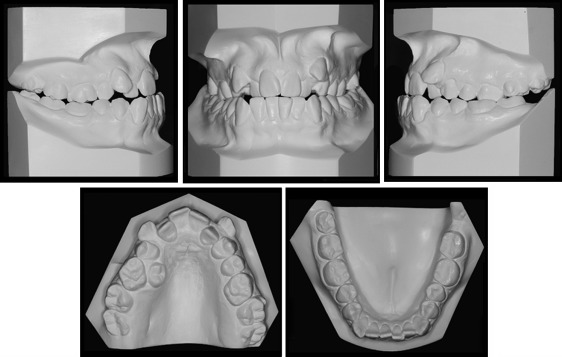
The cephalometric analysis showed a moderate skeletal Class III relationship (ANB angle, −1.2°; Wits appraisal, −4.9 mm) with a normal mandibular plane angle (SN-Go-Gn, 33°), an increased interincisal angle (U1-L1, 152°), and retroclined maxillary incisors (U1-NA, 2.7 mm and 11.9°) and mandibular incisors (L1-NB, 3.8 mm and 17.2°) ( Fig 3 and Table ).
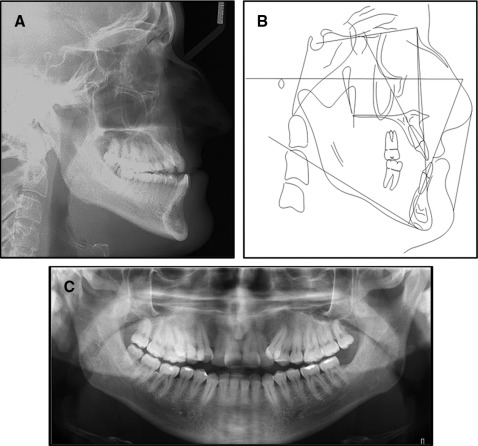
| Norm | Pretreatment | Posttreatment | |
|---|---|---|---|
| SNA (°) | 82 ± 2 | 84.8 | 90.3 |
| SNB (°) | 80 ± 2 | 86.4 | 86.6 |
| ANB (°) | 2 ± 2 | −1.2 | 3.6 |
| Occlusal plane to SN (°) | 14 | 9.2 | 6.4 |
| Pog-NB (mm) | 3 | 0.9 | 1.2 |
| MP-SN (°) | 33 | 33.9 | 31.7 |
| Maxillary incisor-NA (mm) | 4 | 2.7 | 3.6 |
| Maxillary incisor-NA (°) | 22 | 11.9 | 20.2 |
| Mandibular incisor-NB (mm) | 4 | 3.8 | 6.6 |
| Mandibular incisor-NB (°) | 25 | 17.2 | 26.7 |
| IMPA (°) | 95 | 77.3 | 88 |
| Interincisal angle (°) | 130 | 152 | 129 |
| Convexity angle NA-APo (°) | 2.5 | −3.4 | 6.4 |
| Upper lip protrusion (UL-SnPg′) (mm) | 3 | −5.6 | 0.3 |
| Lower lip protrusion (LL-SnPg′) (mm) | 2 | −1.5 | −1.2 |
| Wits appraisal (mm) | −1 | −4.9 | 1.9 |
The patient was diagnosed with a skeletal Class III and dental Class II subdivision right malocclusion with a retrusive maxilla, severe maxillary crowding, mild mandibular crowding, and a bilateral posterior crossbite.
Treatment objectives
The overall treatment objectives for this patient were to align the maxillary and mandibular dental arches, improve the maxillary and mandibular incisor inclinations, correct the bilateral posterior crossbite, obtain ideal overjet and overbite, achieve a good functional occlusion, and improve the skeletal and soft tissue profile.
Treatment objectives
The overall treatment objectives for this patient were to align the maxillary and mandibular dental arches, improve the maxillary and mandibular incisor inclinations, correct the bilateral posterior crossbite, obtain ideal overjet and overbite, achieve a good functional occlusion, and improve the skeletal and soft tissue profile.
Treatment alternatives
Based on the treatment objectives, the following alternatives were presented to the patient.
- 1.
Conventional surgery approach: extraction of the maxillary first premolars and distalization of the maxillary right first molar, followed by orthognathic surgery and postsurgical orthodontic treatment. The advantage of this approach was that teeth could be moved into ideal positions with respect to their respective bones before surgery, making this approach more predictable. The disadvantage was that it could have taken about 2 years.
- 2.
Modified surgery-first approach: orthognathic surgery would be done soon after a short initial alignment period of 4 to 6 months. This period was necessary because of the severe crowding in the maxillary arch, to eliminate any dental interference after maxillary advancement. The expected total treatment time for this approach was 1 year. Because of the short expected total treatment time, the patient chose this option.
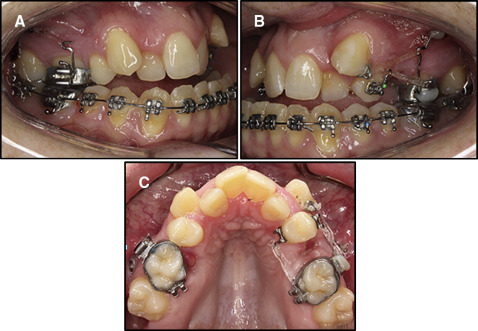
Treatment progress
After the initial appointment for records, the patient was referred to the Division of Oral Surgery for extraction of the maxillary right second premolar, left first premolar, and all third molars. Because of a communication mistake, instead of the maxillary left first premolar, the maxillary left second premolar was extracted. Active orthodontic treatment was started by banding the maxillary first molars and bonding the mandibular arch with a 0.022-in preadjusted edgewise orthodontic appliance (MBT; 3M Unitek, Monrovia, Calif). To maintain the maxillary incisor inclination and resolve the crowding, miniscrews of 2 mm in diameter by 9 mm in length (Lomas system; Mondeal Medical Systems, Tuttlingen, Germany) were placed bilaterally in the infrazygomatic region of the maxilla ( Fig 4 , A and B ). The maxillary left first molar was indirectly anchored to the miniscrew with a sectional 0.019 × 0.025-in stainless steel wire segment ( Fig 4 , B ). Open twin brackets with an attached power arm were bonded on the maxillary left first premolar on both the labial and lingual sides, and 100 g of distalizing force was applied by connecting the power arm of the bracket to the maxillary molar with an elastomeric chain ( Fig 4 , B and C ). A lingual cleat was bonded on the distoincisal line angle of the labially placed maxillary left canine, and a distal tipping force of 50 g was applied by connecting it to the miniscrew with an elastic thread ( Fig 4 , B and C). A power arm was attached to the maxillary right first molar, and a distalizing force of 150 g was applied only on the buccal side by connecting the power arm to the infrazygomatic miniscrew ( Fig 4 , A ). In the mandibular arch, leveling and alignment were started with a 0.016-in nickel-titanium archwire that was upgraded to a 0.016 × 0.022-in stainless steel archwire for the next 3 months. The patient was prescribed 20 minutes of daily use of an intraoral vibrating device (AcceleDent; OrthoAccel Technologies, Bellaire, Tex) throughout the treatment.