Fixed or bonded retainers are routinely placed at the end of orthodontic treatment. Wires of various types and sizes are available, and they can be bonded labially or lingually. This article presents the background for and evolution of multistranded fixed retainers and gives clinical recommendations for their use. Based on my over 20 years’ experience, I recommend a 5-stranded 0.0215-in-diameter wire.
Highlights
- •
Fixed or bonded retainers are routinely placed at the end of orthodontic treatment.
- •
Five-stranded 0.0215-in-diameter wire is recommended for lingual or labial retention.

Today, fixed or bonded retainers are routinely placed at the end of orthodontic treatment. They can be made of a thick 0.030- to 0.032-in wire or a multistranded 0.0215- or 0.0195-in wire. The former is bonded to 2 mandibular teeth (canine-only bonded retainer), and the later is normally bonded to 3 or more teeth (most frequently, the mandibular incisors and canines or the maxillary incisors). This article presents the background for and evolution of multistranded fixed retainers and gives clinical recommendations for their use.
The idea that adhesive materials combined with stainless steel wires might be useful for orthodontic retention was introduced in the mid-1970s. My experience originated from clinical experiments with direct contact splinting. Using sealants and composite resins, we tried to simply splint the contact points of the maxillary and mandibular incisors and canines without the wire, as reported in 1975 at the International Symposium on the Acid Etch Technique in St Moritz, Switzerland. A total of 87 teeth were splinted under rubber dams with emphasis to cover a large incisal-apical distance. Toothpicks were inserted interdentally to make sure that the bonding material did not flow into subgingival areas. The sealant bridges were too weak, and fractures occurred after a few weeks, not only in the enamel-adhesive interface region but also within the material itself. The results with composite materials were better, but breakage was observed whenever segments larger than 2 teeth were splinted. Composite resin splints over 4 or more teeth frequently broke along the enamel-composite resin interface into segments of 1 tooth or 2 teeth. The apparent explanation was that the composite bridges over many neighboring teeth became too rigid and would not allow the individual teeth to exert their normal physiologic mobility. It became evident, therefore, that a bonded retainer must have some elastic properties.
With this working hypothesis, we changed our approach and started to make experiments in which the composite resin was added over thin leveling wires on the lingual surfaces of the teeth, excluding the interdental contacts. Spirals in such wires would potentially give good surface retention, and they could be placed out of contact with the opposing teeth. At first, we tried thin (0.015- to 0.0195-in) 3-stranded wires, but only few years later it was evident that some modification of the original design was needed. Wire breakage and loosening of the retainer wire from the lingual tooth surfaces occurred frequently during the retention period. For this reason, we started comparisons between different types of flexible wires with varying diameters and numbers of strands.
In 1991, we reported that the optimal retainer wire, when the wire is bonded to all teeth in a segment, would be a 5-stranded 0.0215-in wire. This wire had fewer fractures and fewer loosenings than thinner or 3-strand wires of the same thickness, but it was elastic enough to allow for some slight mobility of the individual teeth in a segment. The reduction of wire-fatigue fractures is probably related to the increased flexibility of 5 smaller wires occupying the same diameter as 3 larger wires. Both loosening and wire breakage were observed less frequently with mandibular retainers than with maxillary retainers (over a 3-year period), and most of the maxillary failures occurred mesial or distal to the canines when 6 or 8 teeth were included in the retainer. The most significant side effect was that small spaces tended to open distal to the terminal ends of the retainer wires in some patients who had previously had spacing. This represented a settled occlusion reaching a new equilibrium with the lingual retainer in place.
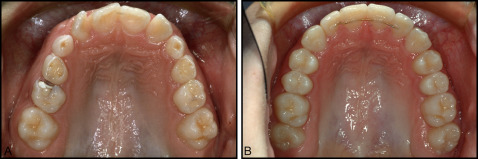
Based on these findings, we have used the 5-stranded 0.0215-in-diameter Penta-One wire, in either stainless steel (Masel Orthodontics, Carlsbad, Calif) or the gold-coated version (Gold’n Braces, Palm Harbor, Fla), as our routine retainer wire for more than 20 years ( Fig 1 ) with excellent long-term success. There was no need to search for another wire type. This is important because other wire models used and reported by other clinicians can lead to more failures, complications, and unwanted side effects. Other authors have reported unexpected movements of anterior teeth to such an extent that retreatment was necessary. These authors used thinner 3-stranded wires, which can have a tendency to unravel or be displaced during retention and introduce torque differences and other peculiar side effects. Such problems do not occur with the 5-stranded 0.0215-in wire if it is carefully shaped and bonded entirely passively. To verify optimal wire fit, we shape the retainer wires on a plaster model because attempts to do this intraorally might introduce imperfections or uncertainty.
For similar reasons, we do not recommend using thin round or rectangular wires for lingual retainers in which several teeth are bonded together. This reflects our original experiments with the contact splints. If the individual teeth in a segment cannot move slightly and independently, the construction becomes too rigid and often results in bond failures between the teeth or the wire and the composite resin. Again, there seems to be a need for a slight tooth mobility for a retainer bonded to several teeth to withstand the forces of occlusion and function. Reports by others have shown that the mobility of the individual teeth in a multistranded bonded retainer decreases with the number of teeth bonded to it, but their mobility will remain within the physiologic range.
Similarly, glass fiber reinforced composite retainers have low flexibility, and a large-scale, long-term clinical study over 2 years recently demonstrated unacceptably high failure rates compared with multistranded retainers (51% vs 12%).
Retainer failure reports by different authors show extremely variable success rates. The apparent simplicity of fabricating and placing a bonded retainer may be misleading, and utmost care throughout the entire clinical procedure should be used if long-term success is the goal. It is not just a coincidence that the best results and the lowest failure rates are found in the studies that are carried out in the private practices of experienced orthodontists. In contrast, the worst results are reported when the retainers are bonded by many dentists having different lengths of experience, or by hygienists and assistants.
The retention protocol must be evaluated on a case-by-case basis. A differential retention approach should be based on the patient’s initial malocclusion characteristics, diagnostic records, habits, cooperation, growth pattern, and age. Our studies have demonstrated that the success rates decreased dramatically when a maxillary multistranded retainer was bonded not only to the 4 incisors, but also to the canines. The critical area is between the lateral incisor and the canine. Therefore, the optimal maxillary retainer for most young and adolescent patients should be a 4-unit retainer, and not a 6- or 8-unit retainer including the canines and the premolars. The maxillary canines normally settle themselves optimally into occlusion with removable retention devices.
Although it may be tempting for less experienced orthodontists to use an 8-unit maxillary fixed retainer, particularly in premolar extraction patients, we caution against this because of our early experiences of unacceptable bond-failure rates when the retainer wire was bonded to the lingual surfaces of the premolars. The alternative—bonding the wire occlusally in the maxillary premolars—presents other problems. In most instances, antagonistic contact cannot be avoided unless a groove is prepared, but this is probably not acceptable in routine situations. In the mesial fissure of the mandibular first premolars, however, it might work well because there is generally enough room owing to the less-prominent lingual cusp.
In the late 1980s, to prevent some space opening in closed extraction sites in adults or when premolars and molars had been moved mesially, and to examine success rates and patient reactions, we started clinical experimentation with short labial retainers. The wires were 0.0215-in 5-stranded stainless steel or gold-coated wires. We found excellent results for short segments (2 teeth) in terms of bonding and retention success and, somewhat surprisingly, outstanding patient acceptance over the 2-year period when they were generally used ( Fig 2 ). However, with longer labial retainers (over 3 or 4 teeth), bond failures increased significantly.





