Fig. 4.1
Dental implants provide an acceptable treatment, in this case replacing the central incisors. (a) The soft tissue emergence profile of the implants. (b) Occlusal view. (c) Radiograph of the final restorations. (d) Completed Restorations
With the continuous success of dental implant restorations, constant innovations have been presented to the dental profession to improve the position of implants, esthetics, and control of occlusion to facilitate ideal restorative procedures.
Initially, implant prostheses were almost entirely screw retained until the early 1990s, when two of the foremost implant manufacturers, Straumann and Nobel Biocare, developed cementable abutment options. Today, implant manufacturers offer several options for screw- and cement-retained restorations. The screw-retained prostheses have the advantage of retrievability over cement-retained restorations; however, screw loosening was an initial issue encountered by many implant restoring clinicians. It is widely thought that this was mainly due to the inadequate tightening of the screw. Torque wrenches were not widely used during restorative procedures, resulting in little, if any, preload being applied to the screw. With no clamping forces, the screw joint would be destined to fail under cyclic loading in the oral environment.
Studies have shown that screw loosening is, in fact, a rare event. Theoharidou et al. published a systematic review on abutment screw loosening in single implant restorations. Their conclusions were that abutment screw loosening occurred as a rare event, regardless of the connection geometry of the implant to abutment, provided proper anti-rotational features and torque were employed. The early failures due to screw loosening led to the use of provisional cements to assist in maintaining the retrievability of cemented prostheses. However, with the current success and predictability of implant restorations, manufacturers are recommending a wide variety of cements, from provisional to definitive resin-based cements. Several authors have suggested that the advantages of cement-retained implant restorations include the following: more passive fit of the casting, improved direction of the load, enhanced esthetics, improved access, progressive loading, and reduced crestal bone loss. Some disadvantages include low profile retention, limited interarch space, retrievability, and presence of cement in sulcus. However, it is more likely that cement-retained restorations have been a restorative treatment of choice by the dental profession due to the familiarized routine of the fabrication of cement-retained tooth restorations. These techniques are well established and were thought to be well understood.
Material Selection: Teeth Versus Implants
Dental cements have been manufactured for use with the natural dentition. The authors have not found any cement that was solely developed for the implant restoration. As a result, the properties of cements are designed to have an interaction with the natural tooth. For example, many release fluoride as an anticaries agent, some cements etch dentine, some chelate to the calcium ion found in tooth tissue, etc. None of these properties are required with dental implants. In fact, some are detrimental with certain implant materials.
Currently there is no ideal cement manufactured for the cementation of implant-supported restorations. The list of available cements is diverse, and it is important that the dental practitioner fully understands that there are different requirements between a natural tooth and the dental implant abutment.
Wadhwani and Schwedhelm summarized in detail the different considerations for material selection specific to teeth and implant-cemented restorations (Table 4.1).
Table 4.1
Some of the differences in cement selection criteria for implant restorations and cement properties for the natural tooth
|
Implant restoration
|
Natural tooth
|
|
|---|---|---|
|
Substructure
|
Metal, ceramic, acrylic
|
Dentine, enamel
|
|
Biological tissue association
|
Peri-implant tissues
|
Periodontal tissues, pulp
|
|
Primary disease issue
|
Peri-implant disease
|
Caries, pulpal, periodontal
|
|
Restorations finish line
|
1–2 mm below the gingiva crest, frequently deeper
|
1/2–1 mm below anterior esthetic sites, often above free gingival margins
|
|
Cementmargin
|
May or may not follow scallop of tissues
|
Preparation follow gingival tissues
|
|
Need forcement seal
|
Questionable
|
Absolute (prevent caries)
|
|
Anticaries agents
|
May be detrimental
|
Desirable
|
|
Corrosion
|
Corrosion of titanium possible
|
Not applicable
|
|
Radiopacity
|
Highly radiopaque
|
Similar to dentine (relatively low)
|
|
Microbial challenge
|
Bacteria found in peri-implant sites
|
Caries-producing bacteria
|
There is no consensus on which cement or material is the most appropriate for cementing implant restorations. Tarica has recorded information on US dental schools and their teaching recommendations for implant restorations.
Survey of US Dental Schools
Two separate surveys in 2008 and 2013 were sent to US dental schools on cementation protocols for implant crown restorations. Although a wide variety of cementation preparations and materials were reported, the surveys revealed some commonly used implant techniques taught at US dental schools. A total of 69 surveys were returned in 2013, representing 65 dental schools and 42 prosthodontic programs. After deleting duplicate responses, 42 surveys were returned from restorative departmental chairpersons, and 27 from advanced prosthodontic residency directors. The new dental schools reported that they did not have a protocol in place yet.
Cement Selection
Some changes were noted in the cement selection between 2008 (Fig. 4.2) and 2013 (Fig. 4.3). Although most institutions taught the use of definitive cement for inserting the final implant prosthesis, there are no standards for cement selection for implant restorations, even within the same institution.
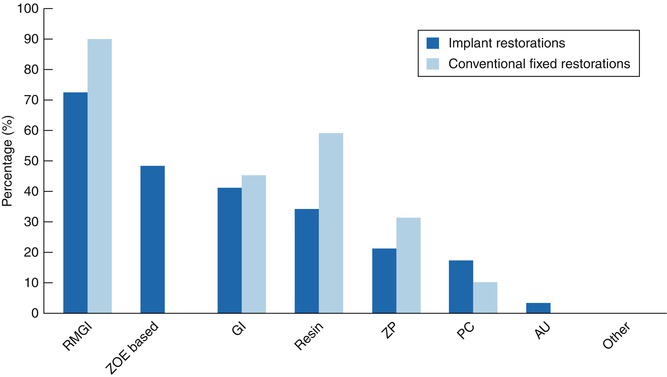
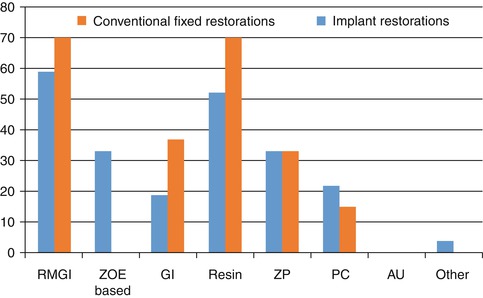
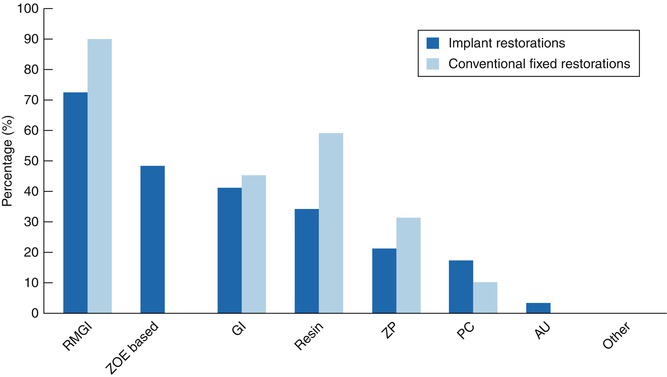
Fig. 4.2
Definitive cements used for implant and conventional fixed restorations by prosthodontic residency directors in 2008. RMGI resin-modified glass ionomer, ZOE zinc oxide eugenol, GI glass ionomer, ZP zinc phosphate, PC polycarboxylate, AU acrylic urethane (Reprinted from the Tarica et al. (2010). Copyright © 2010, with permission from Elsevier)
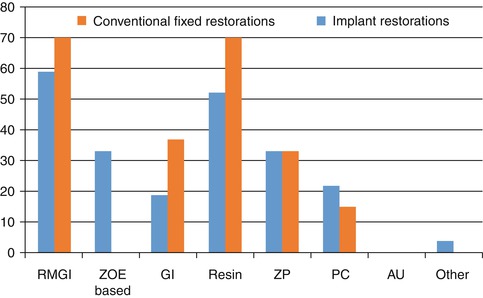
Fig. 4.3
Definitive cements used for implant and conventional fixed restorations by prosthodontic residency directors in 2013. RMGI resin-modified glass ionomer, ZOE zinc oxide eugenol, GI glass ionomer, ZP zinc phosphate, PC polycarboxylate, AU acrylic urethane
A resin-modified glass ionomer cement was found to be the most commonly used among both restorative departments (57 %) and advanced prosthodontic programs (59 %). Advanced prosthodontic programs included glass ionomer (19 %), resin cement (52 %), zinc phosphate (33 %), and polycarboxylate (22 %) cements. The restorative departments taught the use of the following definitive cements: glass ionomer (19 %), resin (33 %), zinc phosphate (19 %), and polycarboxylate cement (17 %).
Provisional cements, ZOE based, were widely used by predoctoral (40 %) and postgraduate (33 %) programs. Some institutions explained that they used a provisional cement to maintain retrievability or to ensure that the restoration was satisfactory prior to using a more retentive cement. The survey also asked the respondents what cements were used for conventional fixed restorations. Eighty-seven percent of the restorative departments taught the use of resin-modified glass ionomer, followed by composite resin, glass ionomer, and zinc phosphate. Acrylic urethane cements were also taught by 14 % of the predoctoral programs. Seventy percent of advanced prosthodontic directors taught the use of resin-modified glass ionomer and resin, glass ionomer, zinc phosphate, and polycarboxylate cements. Both predoctoral and postgraduate programs showed an increase in the use of resin cements and slight decrease of use of resin-modified glass ionomer cements between the 2008 and 2013 surveys, for both implant and conventional fixed restorations. With the increased availability of various all-ceramic restorations, this may have led to the increased use of resin cements for conventional fixed restorations and correspondingly to implant restorations. In general, there seems to be a similarity with cements used for implant restorations, which indicates that the same cements were probably selected from convenience, familiarity, and cost. Some of the literature has shown that the retentiveness of a particular cement for natural dentition may not correlate with implant components. Therefore, until more data is available, the clinician may or may not have the expected retention from the same cement for implant restorations.
The last question on the survey asked if there were any changes in cement for specific clinical situations. Of the 20 predoctoral and postgraduate programs that completed this section, the only trend seen was that a resin cement was used for either a zirconium- or aluminum-based abutment. A few responded that they changed cements depending on the type of ceramic used for the restoration. With regard to abutment and/or restorative material and design, the responses were few and, again, ranged from provisional to definitive cements. Since most of the schools did not respond to this question and there was great variability in cement types, it was assumed that, in general, the same cement is used for most all clinical situations.
Implant System Selection
Implants from various implant manufacturers are used at US dental institutions (Fig. 4.4). The 2013 survey showed the implant manufacturers most used, in order, were as follows: Nobel Biocare, Straumann, Biomet 3i, Astra Tech, and Zimmer. Other implant manufacturers were generally used by less than 37 % of dental schools; however, from 2008 to 2013, this group had increased from 21 %.
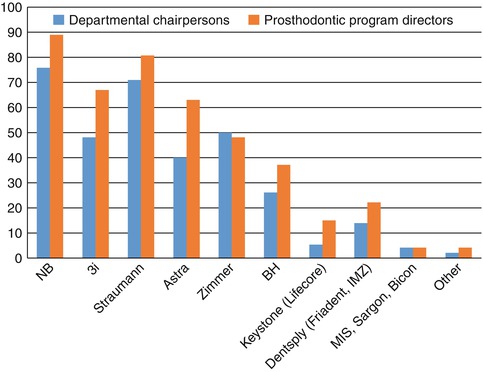
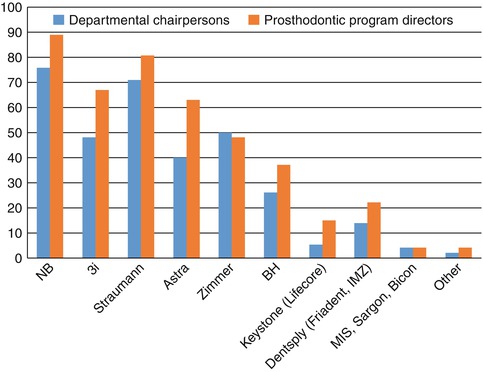
Fig. 4.4
Implant manufacturers used at US dental institutions in 2013. NB Nobel Biocare AB (Gothenburg, Sweden), 3i Biomet 3i Inc (Palm Beach Gardens), Straumann Institut Straumann AG (Basel, Switzerland), Astra Astra Tech Inc (Waltham, MA), Zimmer Zimmer Dental (Carlsbad, CA), BH BioHorizons (Birmingham, AL), Keystone Dentsply (Mannheim, Germany), MIS MIS Implants Technologies Ltd (Shlomi, Israel), Sargon Sargon Dental Implants (Encino, CA), Bicon Bicon (Boston, MA), Other OsseoLink, Global Implant Solutions LLC (Bedford, MA), and Hiossen Inc (Fairless Hills, PA) (Used with permission from Wadhwani et al. (2012). Copyright © Quintessence Publishing Company, Inc., Chicago, IL USA)
Although some schools used up to nine different implant manufacturer systems, most dental schools used only between one to four varieties. Differences also existed among departments in the same school as to the preference of implants used.
Abutment Selection
Schools were asked for their preference to abutment selection. Restorative chairpersons and prosthodontic residency directors responded that they mostly used either prefabricated abutments or the computer-aided, custom-milled abutments. Since the recent expense in gold and the introduction of computer-milled, custom abutments, the survey indicates that traditional custom cast, UCLA-type abutments, are used infrequently.
Abutment Modifications
The survey also included the different surface preparations to either the implant abutment or the restoration prior to final cementation. Most institutions kept the preparation simple with either no modification or only one modification prior to inserting the definitive implant prosthesis. The most common procedure for both predoctoral and postgraduate programs was application of airborne-particle abrasion aluminum oxide to the internal surface of the implant restoration prior to cementation (Fig. 4.5).


Fig. 4.5
An example of abutment modifications. This abutment has been air abraded and also has an axial groove placed. This would represent two modifications
The department chairpersons also indicated that students applied a ceramic primer to the intaglio of the restoration (35 %). Thirty-three percent indicated that grooves were added to the implant abutment to increase the resistance to retention and total convergence angle for the definitive implant cement-retained restorations. Other procedures taught by less than 14 % of predoctoral programs were polishing or abrading the implant abutment with a rotary instrument and the application of a metal primer, tin-plating, or placing a vent hole. Fifty-two percent of the prosthodontic residency directors applied a ceramic primer to ceramic restorations (Table 4.2). In a 2008 survey, only 3 % had reported placing a primer to ceramic restorations. This may indicate an increased use and confidence in cementing all-ceramic restorations on zirconium abutments. Nineteen percent of prosthodontic residency directors reported the placement of grooves on the implant abutments, as well as airborne-particle abrasion of the implant abutment. They also indicated that they polished the abutment, abraded the abutments with a rotary instrument, or used tin-plating to prepare the abutment or restoration prior to cementation. None of the postgraduate programs placed vent holes to aid in cementation. Some schools commented that they prepared the abutment and restoration the same way as cementing to natural dentition.
Table 4.2
Frequency (%) of preparations for implant abutment and/or restoration prior to definitive cementation by department chairpersons (n = 42) and prosthodontic residency directors (n = 27)
|
Abutment modifications 2013
|
Departmental chairpersons
|
Prosthodontic residency directors
|
|---|---|---|
|
Airborne-particle abrasion of internal surface of restoration
|
25 (60 %)
|
15 (56 %)
|
|
No modifications or preparations
|
7 (17 %)
|
2 (7 %)
|
|
Grooves placed on abutment
|
14 (33 %)
|
5 (19 %)
|
|
Airborne-particle abrasion of abutment
|
6 (14 %)
|
7 (26 %)
|
|
Polishing abutment
|
2 (5 %)
|
4 (15 %)
|
|
Application of metal or ceramic primer
|
15 (35 %)
|
14 (52 %)
|
|
Abrading abutment with rotary instrument
|
0
|
1 (4 %)
|
|
Tin-plating
|
0
|
1 (4 %)
|
|
Placement of vent hole
|
1 (2 %)
|
0
|
|
Other
|
0
|
0
|
Immediate Provisionalization
This was taught to predoctoral students in about 55 % of the dental schools and 70 % of the postdoctoral prosthodontic programs. For both pre- and postdoctoral programs, the preferred design for immediate provisionalization was screw-retained restorations. For the few that cemented their provisional restorations, many schools noted that a temporary abutment was placed and the restoration was temporarily cemented.
Management of the Screw Access Channel
Both predoctoral and postdoctoral programs used various types and number of materials to fill the screw access hole. However, most taught their students and residents to fill the screw access completely to the top of the abutment. In 2008, 71 and 86 % of restorative and prosthodontic programs indicated that they teach their students/residents to fill the screw access opening completely. In 2013, the numbers declined slightly to 69 and 67 %, respectively. The survey did not ask for a specific reason; however, more schools may be concerned about controlling the flow of material during cementation. Several different materials and combinations of materials were used to fill the abutment screw access hole. Most schools seemed to use two to three materials, with a range of one to five for predoctoral and one to eight different materials for prosthodontic directors. The major difference between the surveys conducted in 2008 and 2013 was the increased use in PTFE tape as a material to fill the screw access. Table 4.3 shows the most frequently used combination of materials in 2008—note that PTFE (Polytetrafluoroethylene tape or plumbers tape) did not appear on this list. Both restorative and departmental chairpersons and prosthodontic residency directors most frequently filled the screw access hole with a cotton pellet followed by composite, or PTFE tape followed by composite.
Table 4.3
Frequency (%) of usage of various materials for filling screw access opening
|
Material
|
Departmentalchairpersons 2008
|
Departmentalchairpersons 2013
|
Prosthodontic residencydirectors 2008
|
Prosthodontic residencydirectors 2013
|
|---|---|---|---|---|
|
Cotton Pellet
|
24 (77 %)
|
28 (67 %)
|
17 (59 %)
|
16 (59 %)
|
|
PTFE
|
0
|
20 (48 %)
|
0
|
14 (52 %)
|
|
Gutta-percha
|
12 (39 %)
|
5 (12 %)
|
9 (31 %)
|
6 (22 %)
|
|
Light-cured temp.
|
12 (39 %)
|
9 (21 %)
|
8 (28 %)
|
17 (63 %)
|
|
Composite
|
16 (52 %)
|
17 (40 %)
|
18 (62 %)
|
22 (81 %)
|
|
Acrylic
|
0
|
1 (2 %)
|
0
|
3 (11 %)
|
|
Rubber material
|
13 (42 %)
|
15 (36 %)
|
12 (41 %)
|
17 (63 %)
|
|
Amalgam
|
1 (3 %)
|
0
|
1 (3 %)
|
4 (15 %)
|
|
Glass ionomer
|
1 (3 %)
|
1 (2 %)
|
1 (3 %)
|
0
|
|
Cavit
|
7 (23 %)
|
10 (24 %)
|
1 (3 %)
|
3 (11 %)
|
|
IRM
|
1 (3 %)
|
2 (5 %)
|
0
|
0
|
|
Other
|
1 (3 %)
|
1 (2 %)
|
4 (14 %)
|
3 (11 %)
|
Summary
No ideal cement exists, but what is apparent is that little, if any, thought is provided to the choice of material used. Within the dental schools, it appears arbitrary, with the choice for implant restoration commonly reflecting the choice for cementation of crowns and bridges on natural teeth. This oversight is problematic, especially as some cements are detrimental to the materials used in implant. There appears to be little consensus on the most appropriate abutment management also, with differences in different departments even within the same institution. There is a clear need to develop protocols more closely related to scientific enquiry than anecdotal processes.
Understanding and Controlling Cement Flow
Cementation as a means of attaching a restoration—such as an inlay, onlay, crown, or bridge—to a natural tooth has been used for close to 100 years. The process serves to unite components of the same or different materials together. The cementing media used can result in a union that is primarily frictional (e.g., zinc phosphate cement), where some form of mechanical or micro-mechanical interlocking occurs, adhesive in nature where a chemical bond unites the structures (e.g., self-etching resin systems and dentine), or both, depending on the materials joined.
With the advent of dental implants and the subsequent introduction of the cement-retained implant restoration came the emergence of new issues that are not commonly seen to occur when restoring teeth. The cement-retained implant restoration may be more vulnerable to the effects of cement flowing into the soft tissues and residual excess cement on the implant restoration when compared to a tooth. Although there are tens of thousands of articles written on cements, highlighting tensile, shear strengths, their properties, and clinical applications, very little is reported about the way in which cements flow during the cementation process, how to optimize their application, or the amount of cement required to achieve the ideal cementation results.
The occlusion of the cemented crown can be altered by the quality and quantity of cement applied to the internal aspect of the crown. This has been reported by several who have studied cement application techniques with respect to vertical displacement.
Having a sealed restorative margin is considered a prerequisite for a tooth to eliminate ingress of bacteria that could cause subsequent caries. With implant restorations, a bacterial marginal seal provided by cement lute may not be a great concern, especially when one considers the success that screw-retained restorations have, where no seal exists. Marginal adaptation of an implant crown has not been shown to be problematic; Jemt found no issue with the exposed set cement that filled the marginal space between the implant abutment and crown. Marginal seal may, however, be important with respect to cement lute washout during (contamination from crevicular fluids) and after luting (dissolution of the cement) the restoration. Residual excess cement extrusion from around the margin of the cemented restoration of implants is a problem that has also been described in the literature.
Survey: How Much Cement Should We Use?
A recent survey of more than 400 dentists evaluated cement application techniques specifically for implant crowns. The data revealed a large difference in application technique and site. Most dentists (55 %) applied cement on the internal surface with a brush, 28 % of those surveyed applied cement arbitrarily by loading the inside of the crown, and a smaller proportion (17 %) preferentially loaded the internal margin of the crown (Fig. 4.6
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


