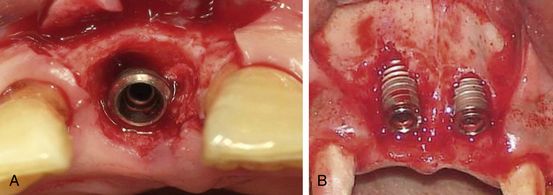
Fig 9.1 (A) Implant placement into an infected socket should be avoided. The tooth number 45 which needs extraction, showed signs of active infection presented with pain on percussion before the extraction. Though, all measures were taken to avoid the infection to the implant, such as prophylactic antibiotics, socket debridement, and flushing the socket with clindamycin before implant insertion, (B) there was infection to the immediately inserted implant, which presented with persistent pain and extraoral swelling even 1 week after (C) the implant placement. (D) When the implant was ultimately removed, the swelling and pain subsided within 24 h with the same antibiotics and analgesics.
Option 2 – extraction, socket grafting, and delayed implant insertion in healed socket
The tooth is extracted and the socket is grafted using appropriate bone substitute to regenerate the adequate bone dimensions at the extraction site. The grafted socket is left to heal for 4–6 months before implant insertion.
Indications
1. Tooth without any active infection.
2. Osseous topography of the extraction socket is not favourable for immediate implantation (large osseous defect).
3. Inadequate bone volume apical to the extraction socket to adequately stabilize the implant.
4. Inadequate band of thick, stable, and keratinized marginal tissue around the extraction socket.
Option 3 – extraction and immediate implant insertion with submersed healing
Immediate implantation in the extraction socket is performed with or without simultaneous bone grafting and covered with the soft tissue flap for submerged healing. The site is re-exposed to uncover and restore the implant after 3–4 months.
Indications
1. Tooth without any active infection.
2. Osseous topography of the extraction socket is favourable for immediate implantation with (small osseous defect) or without (no osseous defect) simultaneous bone grafting.
3. Adequate bone volume apical to the extraction socket is present to stabilize the implant.
4. Adequate zone of thick, stable, and keratinized marginal soft tissue around the extraction socket.
5. The inserted implant achieves adequate primary stability (20–25 Ncm).
Option 4 – extraction and immediate implant insertion with non-submersed/open healing
The dental implant is immediately inserted in the extraction socket and a gingival former, emerging out of the soft tissues, is placed on top of the implant and the flap is sutured around it. The site is left to heal for 4 to 6 months before the implant is restored.
Indications
1. Tooth without any active infection.
2. Osseous topography of the extraction socket is favourable for immediate implantation.
3. Adequate bone volume apical to the extraction socket to stabilize the implant.
4. Adequate zone of thick, stable, and keratinized marginal soft tissue around the extraction socket.
5. The coronal advancement of the flap to achieve primary closure may result in shifting of thick, stable, and keratinized marginal soft tissue to the ridge crest.
6. The inserted implant achieves adequate primary stability (30–35 Ncm).
Option 5 – immediate implantation with nonfunctional loading of the implant
The implant is immediately inserted in the extraction socket and a provisional prosthesis is fixed over the implant, and flap is sutured around it. The prosthesis is kept out of occlusion (nonfunctional loading), which is replaced with a definitive prosthesis, in functional occlusion, after 3–4 months.
Indications
1. Tooth in the aesthetic region.
2. Tooth without any active infection.
3. Osseous topography of the extraction socket is favourable for immediate implant insertion.
4. Adequate bone volume apical to the extraction socket to stabilize the implant.
5. Adequate zone of thick, stable, and keratinized marginal soft tissue around the extraction socket.
6. The coronal advancement of the flap to achieve primary closure can result in shifting of thick, stable, and keratinized marginal soft tissue to the ridge crest.
7. The inserted implant achieves adequate primary stability (>35 Ncm).
Option 6 – immediate insertion with functional loading of the implant
The implant inserted in the extraction socket of low stress aesthetic region and achieves higher bone-implant surface percentage and primary stability (more than 35 Ncm). or, multiple implants are immediately inserted in the extraction sockets with high primary stability and a splinted provisional prosthesis, in functional occlusion, is immediately fixed over these implants, which is later replaced with a long-term definitive prosthesis after the soft tissue is healed in 2–3 weeks.
Indications
1. Immediate implant inserted into the extraction socket in the area of low occlusal forces such as aesthetic region and that achieves adequate BIC percentage and primary stability, e.g. long implant in the maxillary anterior tooth socket, stabilized in the high density nasal floor (< ?xml:namespace prefix = "mbp" />
2. Multiple diseased teeth without any active infection in the aesthetic region.
3. ‘All-on-4’/‘All-on-6’ implant technique done with immediate implantation.
4. Multiple implants in extraction sockets with immediate full-arch restoration.
5. Immediate implantation with implant overdenture, immediately delivered.
6. Osseous topography of the extraction sockets is favourable for immediate implant insertion.
7. Adequate bone volume apical to the extraction sockets to stabilize the implants.
8. Adequate zone of thick, stable, and keratinized marginal soft tissue around the extraction sockets.
9. The coronal advancement of the flap to achieve primary closure can result in shifting of thick, stable, and keratinized marginal soft tissue to the ridge crest.
10. The inserted implants achieve high primary stability (more than 35 Ncm).
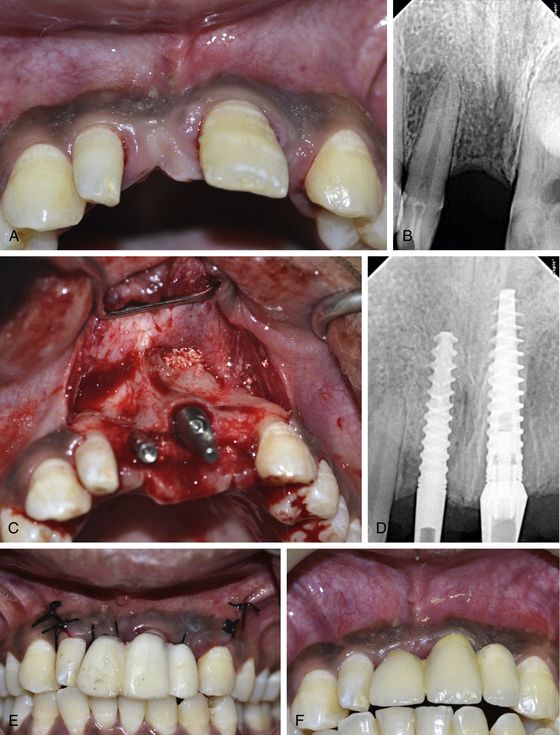
Fig 9.2 (A–D) Teeth are extracted and implants are immediately placed in the sockets of anterior maxilla with apex stabilized in the high density nasal floor to achieve adequate BIC percentage as well as to achieve adequate primary stability of the implants. (E) The inserted implants are immediately restored with a splinted functional prosthesis which is later replaced with the definitive one after the soft tissue (F) healed in 4 weeks.
Deciding factors for implant treatment modality in extraction
1. Osseous topography of extraction socket (bone defect) – Bone defects can be of different types and sizes as long as the implant is positioned within the bone envelope and interdental bone peaks are present. The mode of implant therapy largely depends on the number of intact bony walls the extraction socket contains (
2. Bone dimensions (height and width) – Treatment modality largely depends on the three-dimensional bone dimensions of the socket and the available bone volume apical to the socket to engage the widest and longest possible implant with adequate initial stability and BIC percentage. As a general rule, a minimum 3–5 mm of bone height apical to the extraction socket, should be available to adequately engage the implant apex (
3. Bone density – The density of the bony walls of the socket as well as of the bone apical to the socket also plays a key role in achieving the adequate primary stability of the implant. An implant inserted in the extraction socket achieves less BIC percentage when compared to the implant inserted in the healed socket/bone. Further, if the bone density in the socket area is low, achieving adequate primary stability of the implant can be a challenge for the surgeon, and can lead to micromovements of the implant during its healing phase and subsequent failure. To overcome this complication, the implant surgeon should follow the following guidelines when inserting the implant in the extraction socket in the areas of low-density bone:
4. Occlusal forces The implants inserted in the extraction sockets of maxillary and mandibular anterior regions usually can immediately be restored with nonfunctional loading to fulfil the aesthetic demands of the patient, as the occlusal forces in this region are very low, compared to the posterior segments. The immediate restoration/loading of the single implant should be avoided in the posterior segment.
5. Primary stability of dental implant The mode of implant therapy in the extraction socket largely depends on the primary stability of the implant inserted in the fresh extraction socket.
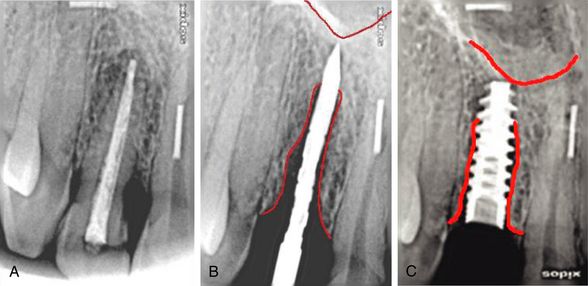
Fig 9.4 (A–C) The apex of the implant should be engaged into 3–5 mm healthy bone apical to the extraction socket to achieve adequate primary stability.
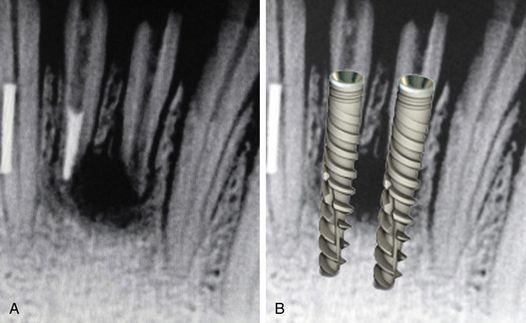
Fig 9.5 (A and B) If any noninfected periapical cyst/radiolucency related to the extracted tooth is present, the implant should further be engaged 3–5 mm apical to the radiolucent area.
If achieving the primary closure of the soft tissue looks difficult and the clinical situation of the inserted implant is not favourable for nonsubmerged healing, one can harvest a thick epithelialized connective tissue graft from the patient’s palate and suture over the inserted submerged implant. Alternatively, the implant surgeon can use the nonresorbable cytoplast barrier membrane to cover the socket opening. This membrane can be left exposed in the oral cavity and immobilized by figure of eight sutures.
9. Oral hygiene – Oral hygiene of the patient should be improved before implant insertion in the extraction socket by scaling, root planing, etc. For such cases, the closed healing protocol should be preferred to avoid any postimplantation infection.
10. Aesthetic and functional demands of the patient – If conditions are favourable, the immediate implant should be preferred in the aesthetic region. It can be immediately restored (nonfunctional) to fulfil the aesthetic demands of the patient. If the implant does not achieve adequate primary stability (more than 35 Ncm) it can be left with submerged healing, and a fixed prosthesis bonded to the adjacent teeth can be given for the aesthetic purposes.
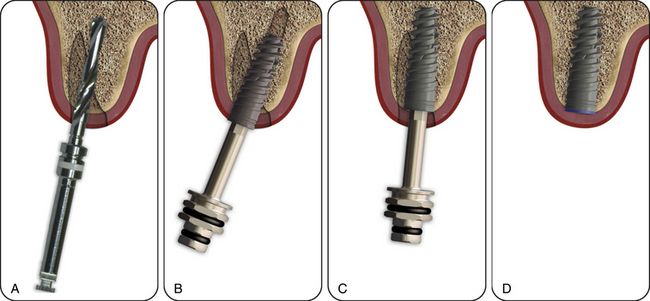
Fig 9.6 The implant with deeper threads with high pitch value, and sharp cutting blades at the apex should be preferred in immediate implantation cases to achieve adequate primary stability. (A–D) The sharp cutting blades at the implant apex also help in directing the implant to the correct three-dimensional positions during insertion.
(Courtesy: Alpha-Bio, Israel)
Special armamentarium required for immediate implantation in the extraction socket
The implant surgeon should have the armamentarium for atraumatic extraction to preserve the hard and soft tissue architecture of the socket for ideal implant placement. The implant surgeon needs to have the set of periotomes and luxators for atraumatic extraction (
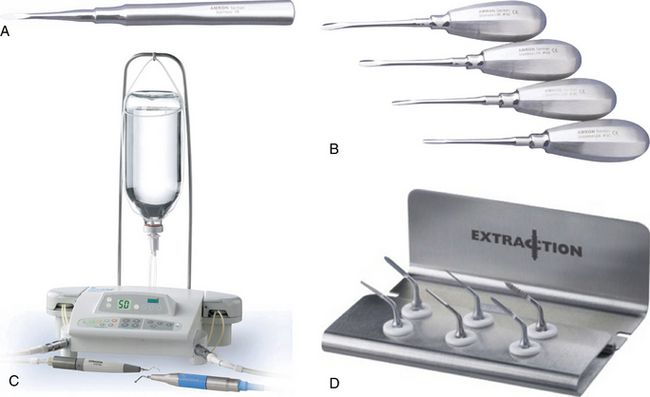
Fig 9.7 Use of (A) periotomes, (B) luxators is highly recommended for atraumatic extraction of the tooth planned for immediate implantation. (C) The piezotome with (D) its special extraction kit offers several advantages for atraumatic extraction of the tooth planned for immediate implantation
(Courtesy: Amron Instrument Company, and Setlec, France).
Grafting the peri-implant socket spaces (jumping distance of osseointegration)
Following tooth extraction, however, a socket often presents dimensions that may be considerably greater than the diameter of a conventional implant. Hence, following implant installation a gap may occur in the marginal part of the recipient site. There are many schools of thought on whether to graft or not to graft these spaces, but as the various studies and clinical trials have shown, any space between implant surfaces and the socket wall which is more than 2 mm may lead to the soft tissue ingrowths, and hence need to be grafted. But if the space is less than 2 mm, the bone will grow to fill the space. This distance is called the ‘jumping distance of osseointegration’.
Extraction socket seal classification – Unlike sockets which are oval and tapered along their length, implants are round. Due to this geometric discrepancy the implant may not completely fill the extraction socket. Krauser and Hahn classified and graded the implant socket on the extent to which an implant occupies the space created by extraction (
Immediate or early loading of the implant inserted in a fresh extraction socket
Based on past studies and clinical trials, the implant inserted in the fresh extraction socket can immediately be restored with functional or nonfunctional loading, especially in the area of high aesthetic concern (maxillary and mandibular anteriors) and lower occlusal stress. Immediate loading of implants requires an understanding of the biology of the recipient tissues, the surgical trauma, the wound-healing process, and the occlusion of the prosthetic reconstruction.
Wound-healing studies have demonstrated osteocoating after 1–2 weeks following the insertion of implant with an osteophilic surface. Implant loading after 2 weeks may therefore turn into a feasible protocol. Certainly, early loading after 6 weeks has become routine.
Loading classification for the immediately inserted implant
1. Conventional loading – The implant is loaded after 3 – 6 months of subgingival healing.
2. Immediate restoration – The implant is restored out of occlusion, within 48 h of insertion.
3. Immediate loading – The implant is restored in occlusion, within 48 h of insertion.
4. Early loading – The implant is restored in occlusion, after 48 h of insertion and before 4 months have elapsed.
5. Delayed loading – The implant is restored after 3 – 6 months.
6. Progressive loading – Light contact at first and gradual loading to full occlusion.
Risk factors for immediate implantation and functional loading
Consensus conference on immediate loading
Primary and secondary implant stability
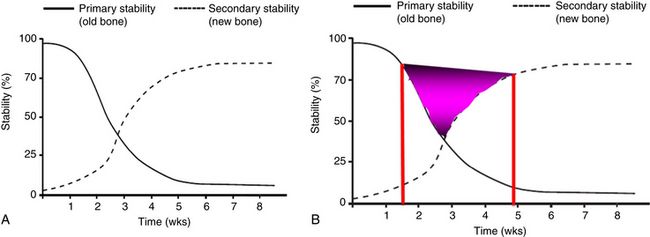
Osseointegration requires bone apposition on the implant surface, without any micromovement. During implant insertion, any stability that the, implant achieves is completely mechanical and is called the primary stability of the implant. Further, during the biological processes of osseointegration of the implant, the surrounding bone physiologically changes in the multiple phases of bone resorption and new bone apposition over the implant surface. During the healing period, however, the biological processes of osseointegration change to a mixture of mechanical and biological stability (secondary stability). Any micromovement of the implant during this phase may lead to the failure of implant osseointegration with the bone. The primary or mechanical stability changes to the secondary or biological stability, once the osseointegration of the implant is completed. Based on different studies this process may, however, take 4 to 6 months (
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses