Conventional and advanced imaging of the temporomandibular joint (TMJ) is universally recognized as central to the processes of diagnosis and treatment planning. Significant enhancements and advances in imaging technology have resulted in modifications of existing imaging modalities, as well as the introduction of faster image acquisition techniques and image processing algorithms. The objective is to enhance the information obtained without increasing the radiation dose, and also to keep costs low. Additionally, the duration of imaging studies continues to be drastically reduced to minimize motion artifacts. Judicious selection of imaging modalities therefore is advocated. Various techniques have been described in the extant literature with specific indications and contraindications.
Significant limitations have been noted with conventional imaging modalities in that the three-dimensional (3D) aspect of the region of interest is seldom captured satisfactorily with conventional imaging modalities when two-dimensional (2D) representation of the region of interest is achieved. Accurate 3D localization of anatomic variants and pathologic entities is therefore relatively difficult to execute. However, these imaging modalities do provide screening examination of the TMJ in patients with suspected joint disease. Additional diagnostic imaging tests may then be prescribed on the basis of clinical and conventional radiographic examination, as necessary. The concept of a TMJ syndrome may no longer exist in that distinct disorders of joint components versus those of the local musculature are easy to distinguish from one another. This has helped in the decision-making process regarding which imaging modality is best suited for a specific diagnostic task.
This chapter serves to provide an overview of existing imaging modalities, indications and contraindications, and imaging parameters as applicable.
CONVENTIONAL IMAGING
Conventional radiography is the imaging modality that is most commonly used to examine the TMJ. It serves as a non-invasive, cost-effective, low-dose diagnostic tool that is easily accessible to the practitioner. Various projections are used to view the TMJ from multiple loci in space. The objective is to obtain non-distorted, possibly superimposition-free diagnostic radiographs with clear visibility of anatomic detail. Routine projections include transcranial, transmaxillary, panoramic, pseudotomographic, lateral oblique, submentovertex (basal), and reverse Towne’s views. In addition, conventional linear or multidirectional tomography may be used for three-dimensional imaging of the TMJ.
Film-based imaging continues to be routinely employed in clinical practice. The advent of digital imaging in dentistry in the recent past has resulted in an exponential increase in the use of this technology. The numerous advantages of digital imaging are being recognized as the technology continues to gain greater acceptance. Many imaging options are available now; their use is facilitated by faster and more efficient digital sensors with higher quantum efficiency, which enable direct or indirect capture of images. The most commonly used technological devices include solid state sensors such as charge-coupled device (CCD)-based units, complementary metal oxide semiconductor (CMOS)-based units, and others such as photostimulable phosphor (PSP)-based sensors that are widely used in high-volume settings such as a hospital. Solid state sensors offer the highest spatial resolution and require relatively lower doses of radiation for image capture. Smaller pixel sizes result in higher spatial resolution within a particular matrix size. However, these sensors are technique sensitive and have limited latitude. Underexposure or overexposure results in non-optimal image quality. On the other hand, PSP sensors have wider latitude and require exposures comparable with those of film. They are less expensive and can be used to upgrade existing film-based imaging units. Advantages of using digital imaging include the lowering of doses in comparison with earlier-generation film-screen systems, the ability to process images to tease out the signal of interest (post-processing) without having to re-expose the patient for possible retakes, the ability to transmit, archive, and retrieve images efficiently and in a timely manner with no change in image quality, and the ability to synthesize or reformat images in other planes with the use of image processing algorithms. Such processing and synthesis of 3D volumes are not possible with film-based images unless they are digitized. All advanced imaging modalities use direct capture electronic sensors.
ADVANTAGES AND DISADVANTAGES
Conventional imaging modalities are less expensive and more easily accessible, and they entail lower radiation doses, when compared with some advanced imaging modalities such as CT. However, image acquisition in 2D results in loss of perception of depth. Regional anatomy superimposed on the regions-of-interest precludes complete evaluation of the TMJ. In addition, the potential exists for image distortion, non-uniform magnification, and the generation of artifacts and other processing errors. Multiple radiographs generally are acquired using differing projection geometry, in order to visualize the entire joint and to localize pathology. A single radiograph is seldom diagnostic of TMD because the information that is captured is limited to two planes as dictated by the specific projection geometry.
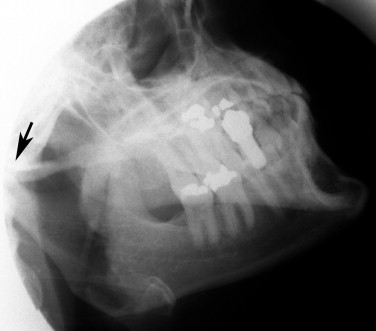
TRANSCRANIAL
This used to be a very popular imaging method before the advent of advanced imaging modalities that use low radiation doses, such as cone beam computed tomography. In settings where access to such modalities does not exist, the transcranial image serves to provide a better view of the lateral aspect of the TMJ by virtue of projection geometry than is provided by the medial or central portion. However, most osseous lesions are known to start in this region. Significant superimposition of the mediolateral poles of the condyle occurs in this 2D projection, in addition to other overlying anatomy in the path of the beam as it traverses the skull. Adequate contrast and density are critical for obtaining a diagnostically acceptable image. The lateral portion of the condyle is nearer to the plane of the film and hence appears with relatively greater clarity. This principle is used in most conventional projections, with the anatomy of interest placed close to the image receptor ( Figure 44-1 ).

TRANSCRANIAL
This used to be a very popular imaging method before the advent of advanced imaging modalities that use low radiation doses, such as cone beam computed tomography. In settings where access to such modalities does not exist, the transcranial image serves to provide a better view of the lateral aspect of the TMJ by virtue of projection geometry than is provided by the medial or central portion. However, most osseous lesions are known to start in this region. Significant superimposition of the mediolateral poles of the condyle occurs in this 2D projection, in addition to other overlying anatomy in the path of the beam as it traverses the skull. Adequate contrast and density are critical for obtaining a diagnostically acceptable image. The lateral portion of the condyle is nearer to the plane of the film and hence appears with relatively greater clarity. This principle is used in most conventional projections, with the anatomy of interest placed close to the image receptor ( Figure 44-1 ).

TRANSMAXILLARY OR TRANSORBITAL
In order to better view the medial and central portions of the condyles, it is recommended that an additional coronal view of the TMJ be acquired. This can be achieved with the use of transmaxillary or transorbital projections. Anteroposterior projection geometry places the TMJ closer to the plane of the receptor ( Figure 44-2 ).

REVERSE TOWNE’S PROJECTION
Another projection that is commonly used to evaluate the condyle is reverse Towne’s view, which is a posteroanterior (PA) projection. A PA view is preferred because of the relative proximity of the condyles to the plane of the receptor (film or digital sensor), which results in an image with relatively greater detail. The patient opens the mouth, allowing translation and rotation of the condyle out of the glenoid fossa. This motion may be limited in trauma. However, if obtained accurately, the view facilitates acceptable evaluation of the medial and lateral poles of the condyle without a corrected axis view, but with a good overview of the subcondylar and upper ramal regions to help rule out fractures. Localization of fractures is facilitated because any displacement along the mediolateral axis can be evaluated ( Figure 44-3 ).

SUBMENTOVERTEX (SMV) PROJECTION
The angulation of the condylar axis with respect to the mid-sagittal plane can be determined with use of the basal projection, also known as the SMV. The base of the skull is imaged, and the condyles are captured on this projection. However, significant superimposition of the floor of the middle cranial fossa onto the TMJ does not permit a meaningful evaluation. This projection has limited applications. An SMV is used to acquire corrected axis tomograms of the TMJ. The mediolateral axes of the condyles are plotted in conventional tomography software to assist with generation of slices parallel to the long axes ( Figure 44-4 ).

LATERAL OBLIQUE VIEWS
The lateral oblique view of each condyle/ramus, a commonly used projection before the introduction of panoramic radiography, can capture relatively good images of the TMJ, one at a time. In the absence of a panoramic imaging unit, this view provides an excellent option for viewing the condyles and the ramus. The glenoid fossa usually is superimposed by overlying anatomy. The central beam is directed at the midpoint of the ramus ( Figure 44-5 ).
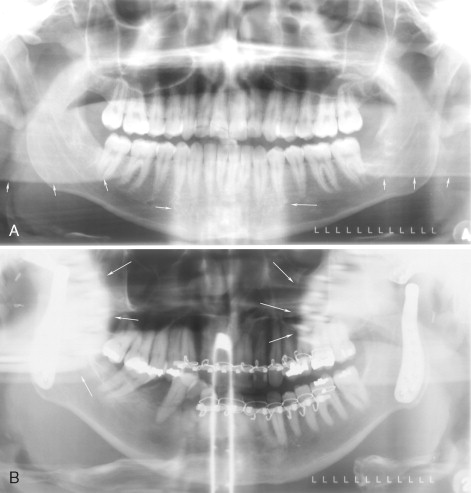
PANORAMIC RADIOGRAPHY
Panoramic radiographs are used as screening tools to evaluate the TMJ. The inherent distortion, magnification, presence of superimposing ghost artifacts, double shadows, and so forth, prevent a thorough and quantitative examination of the osseous TMJ components. However, this view allows bilateral visualization of both TMJs, enabling comparison. The patient’s position in the focal trough of the panoramic unit, as well as the choice of imaging parameters such as the configuration of the focal trough itself, assumes significance in this context. Alterations in imaging geometry have been implemented in some panoramic units to limit exposure to the TMJ. Variable magnification of the images in all three axes has been documented to severely impair the ability to make measurements for diagnosis or for treatment planning purposes. Soft tissue components of the TMJ are not captured adequately, and direct visualization of these structures is not possible, as on any other conventional 2D radiographs. Modifications of the focal trough, as well as changes in the configuration of motion of panoramic imaging units, have been introduced to generate local views of TMJs, as well as pseudotomograms. Pseudotomograms are full-thickness images that appear very similar to tomograms. Many modern panoramic units offer different TMJ imaging options, including true linear tomographic capabilities with corrected axis acquisition capabilities. However, these usually are time-consuming procedures that require limited stabilization and positioning devices; in addition, they generate artifacts that may be seen on linear tomography ( Figure 44-6 ).
CONVENTIONAL TOMOGRAPHY
LINEAR TOMOGRAPHY
Conventional tomography is a process by which slices of regions of interest are generated, one at a time, through different types of simultaneous motion of the x-ray source and the receptor (film or digital). Synchronous movement of these two elements about a center of rotation effectively captures a slice of the region of interest placed at this point. Slice thickness varies inversely with the angle circumscribed by the x-ray source during translational or rotational motion. The more complex the motion, the more effective will be the blurring of superimposing anatomy, thus improving visualization detail. However, it should be borne in mind that a decrease in slice thickness beyond a certain value (2-3 mm) will adversely affect contrast as the thickness of imaged tissue lessens. Artifacts are known to degrade image quality in simple motion configurations such as the linear mode. Many panoramic units offer this basic capability for generating linear tomograms. One slice is generated at a time. The procedure is very technique sensitive and time consuming. However, it does provide an accurate evaluation of the osseous components of the TMJ. Most panoramic units with true tomographic imaging capabilities offer special positioning devices and programs to correct for the mediolateral angulation of the condylar axis, in order to help generate a true orthogonal view of the anatomy. The condylar angle is assessed with respect to the mid-sagittal plane with the use of an SMV view that is acquired first.
MULTIDIRECTIONAL TOMOGRAPHY
Multidirectional tomography units use complex motions such as tri-spiral, hypocycloidal, and figure of eight to generate tomographic slices with minimal artifacts and smaller slice thicknesses. Computer-driven platforms are used for this purpose. Laser positioning lights and the registration of appropriate coordinates in the x, y , and z axes are possible with such units. This is advantageous for long-term follow-up studies, for which some reproduction of imaging geometry may be required. An SMV may be generated and imported into the software with a flatbed scanner to compute the correction needed to generate orthogonal tomograms. Conventional tomography permits accurate measurement of the regions of interest because magnification is known a priori and stays constant over the entire image. Another advantage is that cross-correlation between sagittal and coronal slices can be made as multiple images are captured on film, side by side. Slice thicknesses and the number of slices required to capture the anatomy of interest can be programmed into the unit. A slice thickness of at least 2 to 3 mm is recommended to maintain contrast.
ADVANCED IMAGING MODALITIES
Three-dimensional imaging finds numerous applications in diagnostic imaging of the TMJ, owing to its capability of demonstrating depth-specific information in an interactive manner. Most such imaging is done to evaluate internal derangement because it is a very common problem in about 50% of the population. Anterior disc displacement is more common and is followed by anterolateral positioning. Disc displacement patterns vary to a large extent. Other pathologic entities such as degenerative joint disease, ankylosis, tumors, and developmental anomalies often necessitate 3D imaging. Attempts have been made to quantify osseous changes within the joint via image processing of conventional radiographs. Advanced imaging modalities provide diagnostic information that also can be quantified to characterize pathology and thus determine the optimal mode of intervention. In addition, soft tissue components can be adequately visualized with the use of appropriate techniques.
COMPUTED TOMOGRAPHY
Computed tomography (CT) uses an image-forming algorithm to reconstruct a three-dimensional volume from multiple 2D images of the TMJ. The patient is positioned on the gantry; the x-ray sources and the electronic detector array rotate around the patient and undergo translation as images are continuously acquired. Direct acquisition in most units occurs in an axial plane, but coronal acquisition also can be achieved. The patient will have to be placed in an uncomfortable position for direct coronal capture to occur. However, images can be synthesized or reformatted in any plane such as sagittal or coronal. This process is referred to as multiplanar reformatting (MPR). An entire region of interest thus can be examined in a single procedure. MPR reduces the resolution of images slightly but is deemed adequate for diagnosis. Earlier generations of CT units used less efficient modes of image collection, resulting in longer study times. The potential for motion artifact existed in such cases. Later generations of imaging units are capable of much quicker image generation, such as spiral CT, in which the gantry continues to translate as the x-ray sources and detector array rotate around the patient, thus generating a spiral motion and significantly reducing image acquisition times. Newer units have superior detector technologies and are capable of relatively high spatial resolution. Contrast resolution offered by CT is the highest that can be achieved. Examination of osseous structures with CT, therefore, is considered optimal. However, spatial resolution is still lower than that of digital radiography (DR) in that pixel sizes of the sensors in a CT unit are larger.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


