Introduction
The purpose of this study was to investigate whether lateral cephalometric radiographs influence orthodontic treatment planning. It aimed to compare the odds of a change in treatment plan in three groups of orthodontists who treatment planned six cases on two occasions, T1 and T2, with the provision of a lateral cephalometric radiograph being varied.
Methods
The records of 6 orthodontic patients were copied onto compact discs and sent to the 199 participating orthodontists. The orthodontists were allocated to 3 groups, A, B, and C. Clinicians in group A were given all records except the lateral cephalometric radiographs at the T1 and T2 planning sessions. Clinicians in group B were given all records except the lateral cephalometric radiograph at T1 and all records including the lateral cephalometric radiograph and tracing at T2. Clinicians in group C were given all records including the lateral cephalometric radiographs and tracings at T1 and T2. All participants were sent records at T1; those who returned the treatment-planning questionnaire were sent the second set of records and questionnaire at T2, 8 weeks later. Invitations to participate were distributed to all specialist orthodontists who were members of the British Orthodontic Society (n = 950). Of these, 199 orthodontists agreed to take part, a response rate of 21%. Of the 199 who agreed to participate, 149 completed the first treatment-planning questionnaire (T1), for a response rate of 75%. Of the 149 who completed that questionaire, 114 completed the second treatment-planning questionnaire (T2), for a 77% response rate.
Results
The availability of a lateral cephalometric radiograph and its tracing did not make a significant difference to any treatment-planning decisions, with the exception of the decision to extract or not between groups B and C for all 6 patients combined, and between groups B and C and groups B and A for patient 4 (Class I incisor relationship on a Class II skeletal base).
Conclusions
For most treatment-planning decisions in these 6 patients, the availability of a lateral cephalometric radiograph and its tracing did not make a significant difference to the treatment decisions. For 1 patient, there was a significant change in the extraction decision when a lateral cephalometric radiograph was provided. This highlights the uncertainty surrounding the necessity for lateral cephalometric radiographs in treatment planning. Further research in this area is encouraged to resolve this dichotomy.
Since the introduction of cephalometry by Broadbent in 1926, the lateral cephalometric radiograph has become a standard tool in orthodontic assessment and treatment planning. This is despite the acknowledged health risks associated with exposure to ionizing radiation, in particular the somatic stochastic effects that increase the risk of cancer during the patient’s lifetime. It is well established that there is significant everyday background radiation that accounts for approximately 87% of radiation exposure. Nevertheless, since radiation is cumulative, health care professionals must limit diagnostic radiation exposure to an absolute minimum, and all exposures should be justifiable in terms of management of the patient. Current guidelines in the United Kingdom for clinical orthodontics give the following indications for use of a lateral cephalometric radiograph.
- 1.
A skeletal discrepancy when functional or fixed appliances are to be used for labiolingual movement of incisors.
- 2.
Patients with moderate skeletal discrepancies in a teaching environment.
- 3.
The location and assessment of unerupted, malformed, or ectopic teeth.
- 4.
Limited serial radiographs for assessing growth and planning joint orthodontic-orthognathic surgery patients.
There is a lack of evidence on the value of lateral cephalometric radiographs in orthodontic treatment planning, although their routine use is widely accepted. Studies have shown intraexaminer and interexaminer variability in treatment planning, even with the same records.
As far back as 1979, Silling et al questioned the need for lateral cephalometric radiographs in certain patients. Han et al found that, in 55% of patients, study models alone provided adequate information for treatment planning, and the incremental addition of other diagnostic records made minimal differences. More recently, Bruks et al noted that, for most patients, the clinical examination, supplemented with study models and photographs, provided adequate information for orthodontic treatment planning. They stressed that individually based selection criteria should be used for radiographic examination. However, Pae et al stated that the lateral cephalometric radiograph might influence treatment planning in patients with bimaxillary protrusion and Class II Division 2 malocclusion. Nijkamp et al, in the most recent orthodontic treatment-planning study, involving 10 orthodontic postgraduates and 4 qualified orthodontists, examined study models and lateral cephalometric radiographs and their tracings of 48 subjects aged 11 to 14 years on 4 occasions at intervals of 1 month. They concluded that cephalometrics does not appear to influence orthodontic treatment planning for Class II Division 1 adolescents.
The aim of our study was to investigate whether lateral cephalometric radiographs influence orthodontic treatment planning. We aimed to compare the likelihood of a change in treatment plan in 3 groups of orthodontists, planning treatment for 6 patients on 2 occasions (T1 and T2), with the provision of a lateral cephalometric radiograph varied. The null hypothesis was that the availability of a lateral cephalometric radiograph does not influence (1) whether to extract, (2) the choice of extractions, (3) the choice of appliances used, (4) whether anchorage reinforcement is required, and (5) whether orthognathic surgery is indicated.
Material and methods
The study was approved by Oxfordshire Research Ethics Committee A on September 23, 2008, and Trust Management Approval and Indemnity was confirmed by the Oxford Radcliffe Hospitals NHS Trust on October 7, 2008.
The clinical patients ( Table I ) were chosen from the cohort of patients undergoing orthodontic treatment at the John Radcliffe Hospital, Oxford, United Kingdom. Patients with congenital anomalies—eg, clefts—and those with incomplete records were excluded. Six patients consented to participate; their ages ranged from 12 to 28 years.
| Patient | Age (y) | Malocclusion |
|---|---|---|
| 1 | 12 | Class II Division 1 on a skeletal II base; overjet, 9 mm |
| 2 | 16 | Class III on a mild skeletal III base |
| 3 | 28 | Class II Division 1 on a skeletal I base; overjet, 10.5 mm |
| 4 | 15 | Class I on a skeletal II base |
| 5 | 17 | Class I on a skeletal I base, impacted UL3, missing UR2 |
| 6 | 13 | Class II Division 2 on a skeletal II base |
The records of the 6 orthodontic patients were replicated. These included (1) a summary of the clinical findings, (2) photographs of the angle trimmed study models, (3) standard clinical photographs comprising 4 extraoral and 5 intraoral views, (4) a lateral cephalometric radiograph and a panoramic radiograph, and (5) a tracing of the lateral cephalometric radiograph.
These items were recorded on 2 sets of compact discs for posting to the participating orthodontists; 1 set contained all records, and 1 omitted the lateral cephalometric radiograph and tracing.
One hundred ninety-nine orthodontists were self-selected by replying to either a global e-mail sent to all specialists on the British Orthodontic Society (BOS) mailing list or to a subsequent written invitation and reply slip distributed with the BOS newsletter in November 2008.
The orthodontists were listed consecutively in the order they replied and then randomized in blocks of 3 by using computer-generated random numbers, with 1 orthodontist allocated to each of the groups: A, B, or C ( Fig ).
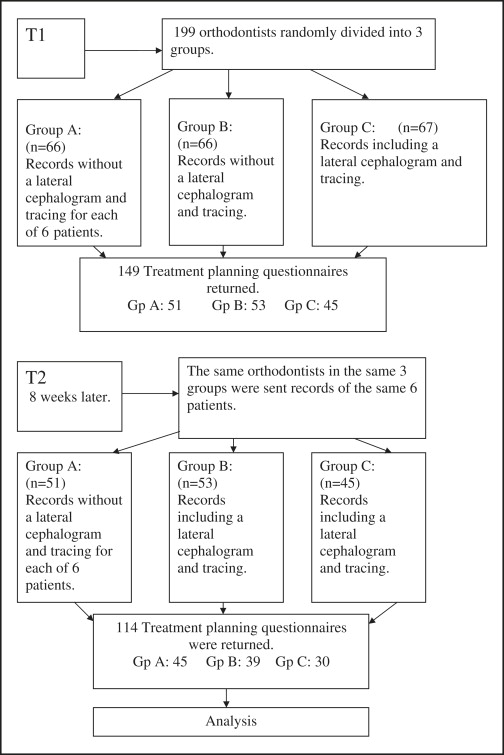
All participants were sent records at T1, and those who returned the treatment-planning questionnaire were sent a second set of records 8 weeks later at T2 ( Fig ). At T1, they were unaware that a second set of records would be sent. Clinicians in group A did not have the lateral cephalometric radiographs and tracings at T1 and T2. Clinicians in group B did not have a lateral cephalometric radiograph and tracing at T1, but all records, including the lateral cephalometric radiograph and tracing, were sent at T2. Clinicians in group C were given all records, including the lateral cephalometric radiographs and tracings, at T1 and T2. A reminder e-mail or letter was sent to each nonresponding orthodontist 3 or 4 weeks after sending the records at both T1 and T2.
Included with each compact disk was a treatment-planning questionnaire that asked a number of questions, including the following.
- 1.
Would you extract teeth in this patient? If yes, which teeth?
- 2.
What appliance type would you use: removable, functional, fixed, or a combination?
- 3.
Should anchorage be reinforced?
- 4.
Would you recommend orthognathic treatment?
- 5.
Would you like to provide any additional information about the treatment plan?
- 6.
What, if any, additional information would you have found helpful?
- 7.
How long has it been since you qualified as an orthodontist?
A feasibility study was initially undertaken. This involved the 6 patients’ orthodontic records sent on a compact disk, along with the questionnaire, to 10 orthodontists. The main study began after some minor amendments to the questionnaire.
The results were examined by using 2 statistical packages, SPSS for Windows (version 14, SPSS, Woking, United Kingdom) and Stata (version 10.0, StataCorp, College Station, Tex).
Chi-square tests (for 2 × 2 tables) were carried out for each treatment decision to test for differences in the percentages of changed decisions for the 3 groups of orthodontists. This was carried out for the 6 patients collectively and also for each patient individually. Each test yielded a P value that indicated whether there was a significant difference between the groups for that particular treatment decision.
Binary logistic regression was used to compare the odds of a change in treatment plan between T1 and T2 for the 3 groups and to ascertain whether any differences were significant. This was carried out for each treatment-planning decision for all 6 patients individually. The odds ratio (OR) indicates how much more, or less, likely 1 group of practitioners were to change their decisions compared with another group. ORs that were statistically significantly greater than 1 represented a group that was statistically significantly more likely to change a decision than the comparison group; conversely, an OR that was statistically significantly less than 1 represented a group that was significantly less likely to change a decision than the comparison group.
A generalized estimating equation (GEE) approach was also used to calculate ORs for the likelihood of changing each treatment decision for all 6 patients combined. The use of a GEE model permitted the calculation of robust standard errors to account for the clustering of patients within participants, since each orthodontist examined 6 sets of patient records. Routine statistics assumes that the observations are independent, and, since each respondent examined 6 sets of records on 2 occasions, the data were not strictly independent; hence the decision to use the GEE.
Results
Invitations to participate were distributed to all specialist orthodontists who were members of the BOS (n = 950). Of these, 199 agreed to take part, for a response rate of 21%. Of the 199 who agreed to participate, 149 completed the T1 treatment-planning questionnaire, for a response rate of 75%. Of those 149, 114 completed the T2 treatment-planning questionnaire, for a 77% response rate. The overall response rate—ie, those who completed T2 as a percentage of those who initially agreed to take part—was 57%.
Table II shows the percentages of changed decisions for all 6 patients combined and for the patients individually. For the 6 patients combined, the extraction pattern showed the highest variability (42.9% of the respondents changed their decision). The next highest percentage of changed decisions related to whether anchorage reinforcement was needed (24%), followed by the decision to extract (19.7%). The individual group (A, B, and C) changes showed similar patterns, although there were some variations in the order of the changed decisions ( Table II ).
| All 6 patients | Extraction decision | Extraction pattern | Removable appliance decision | Functional appliance decision | Anchorage reinforcement decision | Orthognathic surgery decision |
|---|---|---|---|---|---|---|
| Overall | 19.7% | 42.9% | 7.5% | 10.0% | 24.0% | 9.8% |
| Group A | 17.9% | 41.4% | 8.8% | 11.2% | 24.4% | 8.1% |
| Group B | 24.4% ∗ | 46.2% | 4.8% | 10.5% | 21.1% | 8.9% |
| Group C | 15.9% ∗ | 40.9% | 8.9% | 7.8% | 27.1% | 13.4% |
| Patient 1 | ||||||
| Overall | 26.9% | 41.1% | 9.7% | 31.3% | 25.7% | 0% |
| Group A | 26.2% | 35.7% | 9.1% | 31.8% | 26.3% | 0% |
| Group B | 34.2% | 51.4% | 5.1% | 34.2% | 24.3% | 0% |
| Group C | 17.9% | 35.7% | 16.7% | 26.7% | 26.9% | 0% |
| Patient 2 | ||||||
| Overall | 3.6% | 23.4% | 6.3% | 0.9% | 19.4% | 6.1% |
| Group A | 2.3% | 27.9% | 11.4% | 2.3% | 18.6% | 7.9% |
| Group B | 5.3% | 18.4% | 2.6% | 0% | 11.4% | 2.9% |
| Group C | 3.3% | 23.3% | 3.3% | 0% | 30.0% | 7.7% |
| Patient 3 | ||||||
| Overall | 18.5% | 67.6% | 1.8% | 0% | 25.6% | 23.3% |
| Group A | 26.8% | 73.0% | 0% | 0% | 17.1% | 15.0% |
| Group B | 10.8% | 65.7% | 0% | 0% | 27.3% | 31.4% |
| Group C | 16.7% | 63.3% | 6.7% | 0% | 36.4% | 25.0% |
| Patient 4 | ||||||
| Overall | 21.8% | 56.9% | 6.3% | 2.7% | 23.5% | 7.2% |
| Group A | 14.3% ∗ | 46.3% | 11.4% | 4.5% | 30.6% | 5.6% |
| Group B | 35.9% ∗ | 64.1% | 2.6% | 2.6% | 16.7% | 2.9% |
| Group C | 13.8% ∗ | 62.1% | 3.4% | 0% | 23.1% | 14.8% |
| Patient 5 | ||||||
| Overall | 27.3% | 49.5% | 3.6% | 0% | 26.1% | 9.1% |
| Group A | 24.4% | 56.1% | 4.8% | 0% | 26.7% | 11.8% |
| Group B | 33.3% | 52.6% | 0% | 0% | 25.8% | 3.2% |
| Group C | 23.3% | 36.7% | 6.7% | 0% | 25.9% | 13.0% |
| Patient 6 | ||||||
| Overall | 20.4% | 20.6% | 17.0% | 25.0% | 24.2% | 13.5% |
| Group A | 14.6% | 12.5% | 16.3% | 27.9% | 28.6% | 9.4% |
| Group B | 26.3% | 26.3% | 17.9% | 25.6% | 21.9% | 12.5% |
| Group C | 20.7% | 24.1% | 16.7% | 20.0% | 20.8% | 20% |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


