Long, flowing thick hair has been a symbol of male and female power and physical beauty since ancient times. So it is not hard to imagine the loss of self-esteem and unfavorable psychological impact experienced by men and women with significant baldness or alopecia. Until the early 1990s, little could be done in the way of hair transplantation that would look natural, remain undetectable, and allow freedom of styling.
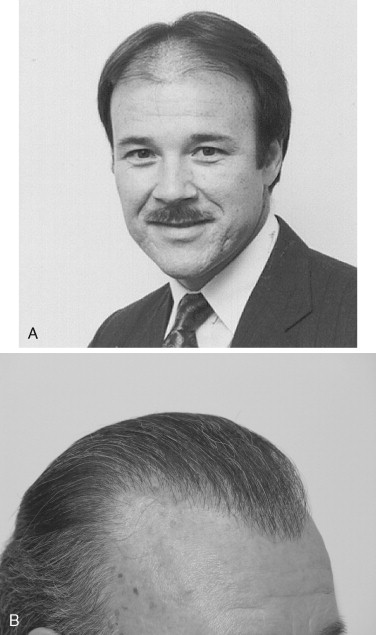
Orentreich in the 1950s pioneered early alopecia research and the early hair transplantation technique, which consisted of large 8 mm punch grafts. Unfortunately, in many patients, these grafts closely resembled tufted baby doll’s hair. These grafts worked well in special circumstances when they were covered by adjacent combed over natural hair with special styling. The modern method of using very small grafts such as the micrograft (1 to 2 hairs) and the minigraft (3 to 5 hairs) did not gain wide acceptance by most hair transplant surgeons until the mid 1990s. The author was introduced to this technique by Paul Straub, MD, second president of the International Society of Hair Restoration Surgeons at his office in Torrence, California, in 1993. I then taught the doctors who performed my own hair restoration. I now have approximately 1,750 micrografts and minigrafts in my frontal and anterior coronal scalp areas, and I feel much better about my appearance because of them ( Figure 30-1, A and B ). Ironically, the micrograft and the minigraft were originally introduced to the medical community by two different Japanese physicians, who published their findings in an obscure Japanese medical journal in the 1930s and 1940s. These techniques were eventually rediscovered years later by other surgeons who were trying to improve the naturalness of their patients’ hair grafts by reducing their size.
This chapter is not meant to be an all-inclusive treatise on alopecia and hair transplant techniques. Instead, it is meant to be an overview of currently accepted theories and techniques in hair transplantation for those surgeons who are contemplating offering these surgical services to their patients. As with any new surgical technique that is added to a surgeon’s practice, appropriate didactic and hands-on training is mandatory.
PATHOPHYSIOLOGY OF ALOPECIA
Current and past research supports the fact that common alopecia or baldness is genetically and hormonally mediated. Without the genetic makeup for baldness and the presence of testosterone with its metabolite dihydroepiandosterone (DHT), the individual will not bald. Both must be present for alopecia to occur. Eunuchs do not express their baldness if it is present because of their lack of testosterone. However, if the testosterone level is restored to normal, even years later, they will express this trait to its full extent. Alopecia is also chronological in nature. The individual’s specific genetic baldness pattern will fully express over time, not all at once. For this reason, no one can predict the pattern or extent of an individual’s alopecia.
CURRENT MEDICAL TREATMENT
Many salves and bogus treatments have been put forth over the years for the treatment of alopecia. However, only two chemical compounds are now FDA approved for this indication. Minoxidil was first introduced as a potent peripheral vasodilator for the treatment of resistant hypertension. During trials of the drug, hypertrichosis was noted in some patients. Later, a multicenter study showed that roughly 8% of patients exhibited complete reversal of their baldness with topical minoxidil. Other patients demonstrated less re-growth. Upon discontinuation of treatment, hair reverted to the pretreatment state within 2 months. The mechanism of action is thought to be related to the vasodilatory effects on scalp skin and is thought to be a possible direct effect of minoxidil in promoting hair growth.
Finasteride was first marketed for the treatment of benign prostatic hyperplasia, a common disorder in men. It is a specific inhibitor of steroid type II 5a-reductase, which converts testosterone to DHT. Besides shrinking the prostate, it was noted that in some patients, this drug would re-grow the hair. The company eventually repackaged the drug in a lower dose form and marketed it for the treatment of baldness.
CURRENT MEDICAL TREATMENT
Many salves and bogus treatments have been put forth over the years for the treatment of alopecia. However, only two chemical compounds are now FDA approved for this indication. Minoxidil was first introduced as a potent peripheral vasodilator for the treatment of resistant hypertension. During trials of the drug, hypertrichosis was noted in some patients. Later, a multicenter study showed that roughly 8% of patients exhibited complete reversal of their baldness with topical minoxidil. Other patients demonstrated less re-growth. Upon discontinuation of treatment, hair reverted to the pretreatment state within 2 months. The mechanism of action is thought to be related to the vasodilatory effects on scalp skin and is thought to be a possible direct effect of minoxidil in promoting hair growth.
Finasteride was first marketed for the treatment of benign prostatic hyperplasia, a common disorder in men. It is a specific inhibitor of steroid type II 5a-reductase, which converts testosterone to DHT. Besides shrinking the prostate, it was noted that in some patients, this drug would re-grow the hair. The company eventually repackaged the drug in a lower dose form and marketed it for the treatment of baldness.
MICROGRAFT AND MINIGRAFT HAIR TRANSPLANT TECHNIQUE
The beauty of the micrograft and minigraft hair graft technique is that it imports an appearance of naturalness throughout the hair transplantation process, whether a small or a large number of grafts are performed per session. Patients with significant frontal or significant vertex alopecia usually will require from 1,200 to 2,000 grafts to give the appearance that their hair density has returned to an acceptable state. This usually is accomplished in two to four sessions, depending on the individual’s unique progression of alopecia.
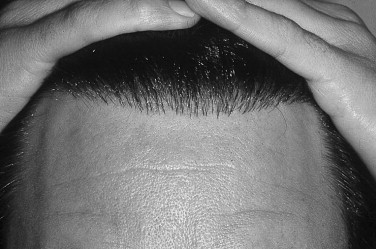
Normally, hairs grow in groups called follicular units with their associated supporting structures, which consist of terminal and vellus hairs, associated sebaceous glands, and the arrector pili muscle. These groups represent small tufts of hair, which can be easily identified with 3 to 10× magnification. The transplant surgeon and his team should try to respect these units and, to the extent possible, transplant them to the recipient site intact. Along the hairline, micrografts allow the gradual thickening of hair, which progresses from anterior to posterior so that the hairline is not a line at all. Instead, it is a zone where artistry and attention to technique will yield undetectable hair transplants, even when the hair is combed straight back ( Figure 30-2 ).
Harvesting of the donor hair is performed in a zone that is located roughly 2 cm to either side of the occipital ridge and then curves at the lateral extent superiorly up to the posterior temporal area. The hair in this area to be harvested is cut to stubble length with scissors. Usually, strips of variable length and approximately 1 to 1.5 cm wide are removed under local anesthesia of lidocaine with epinephrine via the ellipse method or with a multi-bladed harvesting knife to yield the necessary grafts ( Figure 30-3 ). The strips or the ellipse is dissected free of the underlying fascia with blade or scissors dissection, staying deep to the hair bulbs and leaving approximately 2 to 3 mm of fat deep to the bulbs. Hemostasis is attained with electrocautery, and the wound is repaired with a running 4-0 polypropylene running suture that closes only the skin. Some surgeons prefer staples, but these seem to be uncomfortable for the patient. They do prevent damage to the remaining hair follicles. During the next harvest, approximately 3 to 5 months later, the old scar is removed with the newly harvested hair. In this manner, only one scar will result when the process is complete.

Hair transplantation requires a team approach. Therefore, after the strip of harvested hair is removed, it is immediately passed to assistants, who will dissect it into micrografts and minigrafts ( Figure 30-4
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


