Surgical alteration of the chin is an important aspect of achieving or restoring global facial balance in the management of dentofacial deformities. In current practice, two procedures are most frequently employed: (1) augmentation with chin implant, and (2) osteotomy and/or ostectomy. Limitations have been identified in terms of what can be achieved with chin implants, particularly when one of the treatment goals is improved muscle function. Chin implants can facilitate lateral contour augmentation, which can be a problem when chin osteotomy is performed alone. Genioplasty by osteotomy-ostectomy is not limited to correction of cosmetic deformities; it can be used to the advantage of the patient to normalize the vertical height of the chin and to ameliorate hyperactivity of the mentalis muscle complex. Functional genioplasty is an osteotomy-ostectomy of the anterior mandible that reduces excessive lower anterior facial height to 55% of total anterior facial height. This procedure is indicated particularly when one factor that contributes to the long-face syndrome is vertical excess of the anterior mandible. The surgical technique involves creation of a tenon and mortise, which not only preserves the insertions of the labiomental muscles and at least some of the suprahyoid muscle but also improves the stability of transosseous fixation. Superior repositioning and advancement of the chin and myocutaneous structures produce both functional and esthetic benefits for the patient. Anatomic placement of fixation devices used in genioplasty is an important long-term consideration.
FUNCTIONAL GENIOPLASTY
The term functional genioplasty seems to represent something of a paradox because, in the past, surgery on the chin has been thought of primarily in the context of cosmesis. In man, changes in form produce attendant changes in function; the functional genioplasty is an example of an operation that can bring about a beneficial change in function by altering the position and form of the chin and its associated myocutaneous structures.
The maxillary component of vertical excess of the anterior face has been described in detail with respect to both diagnosis and treatment, but less attention has been directed to the contribution that is made to this deformity by excessive vertical dimension of the anterior mandible.
Muller has stressed the importance of the state of balance that exists in the normal face between the hard structures of the lower face (namely, the maxilla, the mandible, and the teeth) and the soft tissue elements (namely, the tongue, the labiomental musculature, and the overlying skin). During growth, if the hard tissues and the soft tissues of the lower face are in balance, the lower face will register itself harmoniously in the rest of the face. Artists, among others, have interpreted this harmony as equality in height of the upper face and the lower face. This subjective impression is imprecise; indeed, Fields and associates have shown that experienced clinicians poorly categorize underlying skeletal deformities solely on the basis of evaluation of the soft tissue profiles. Wylie demonstrated radiographically that the upper anterior face, measured from nasion (Na) to anterior nasal spine (ANS), constitutes 45% of the total anterior facial height, and the lower anterior facial height, measured from ANS to menton (Me), constitutes 55%. Delaire has confirmed via architectural and structural craniofacial analysis that these percentages represent constants of ideal vertical facial height.
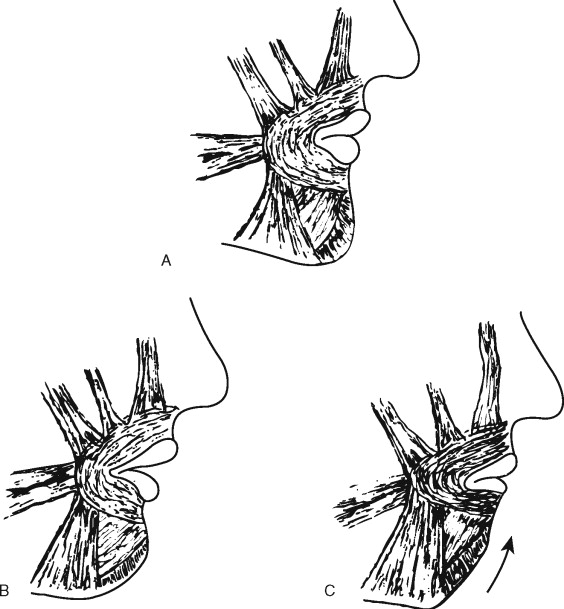
When an anomaly of form and function of the hard or soft tissue elements of the lower face is present during growth, it affects the neighboring structures, which, together, can now produce a progressive regional disequilibrium until maturity is reached. This is the case in the presence or absence of vertical maxillary excess when the ANS-Me distance is excessive. The lips become incompetent in repose and no longer oppose the thrust of the tongue, which now can interpose itself between the teeth. To occlude the lips, active contraction of the labiomental musculature is necessary; this, in turn, ultimately causes flattening of the soft tissue contour of the chin ( Figure 5-1 ). This set of circumstances leads to functional habits that produce clinical problems, the precise definitions of which represent the indications for surgical intervention.
INDICATIONS
Indications for functional genioplasty are as follows:
- I.
Vertical excess of the lower anterior facial height in which the following clinical signs and radiographic findings are present:
- A.
Clinical signs
- 1.
Lip incompetence when the lips are in repose and a normal relationship of the maxillary incisor tooth to the upper lip exists
- 2.
Open mouth posture with interposition of the tongue between the teeth
- 3.
Elevation of the mental soft tissues to obtain lip closure
- 4.
Thinning of the alveolar bone overlying the facial surfaces of the roots of the anterior mandibular teeth
- 5.
Flattening of the contour of the anterior surface of the soft tissue profile of the chin
- 1.
- B.
Radiographic findings
- 1.
ANS-Me distance, which constitutes more than 55% of the total anterior facial height, in the absence of vertical maxillary excess
- 2.
ANS-Me distance, which persists in constituting more than 55% of the total anterior facial height after predicted or actual appropriate correction of vertical maxillary excess, open bite, or anteroposterior dentofacial deformities
- 1.
- A.
- II.
Residual and associated deformities or cleft lip/cleft palate, particularly in the case of insufficient cheiloplasty in which the upper lip is too short. Superior repositioning of the mental osseous and the myocutaneous tissues can aid in achievement of lip competence and development of the upper lip
- II.
Requirement for a complimentary procedure to adjust lower anterior facial height when maxillary and mandibular osteotomies are performed for correction of anteroposterior and transverse maxillofacial deformities
- IV.
As an aid in stabilization of orthodontic treatment results by normalization of the osseous and myocutaneous elements of the lower face
- V.
As a complementary procedure with partial anterior glossectomy to aid in the management of dental open bite
INDICATIONS
Indications for functional genioplasty are as follows:
- I.
Vertical excess of the lower anterior facial height in which the following clinical signs and radiographic findings are present:
- A.
Clinical signs
- 1.
Lip incompetence when the lips are in repose and a normal relationship of the maxillary incisor tooth to the upper lip exists
- 2.
Open mouth posture with interposition of the tongue between the teeth
- 3.
Elevation of the mental soft tissues to obtain lip closure
- 4.
Thinning of the alveolar bone overlying the facial surfaces of the roots of the anterior mandibular teeth
- 5.
Flattening of the contour of the anterior surface of the soft tissue profile of the chin
- 1.
- B.
Radiographic findings
- 1.
ANS-Me distance, which constitutes more than 55% of the total anterior facial height, in the absence of vertical maxillary excess
- 2.
ANS-Me distance, which persists in constituting more than 55% of the total anterior facial height after predicted or actual appropriate correction of vertical maxillary excess, open bite, or anteroposterior dentofacial deformities
- 1.
- A.
- II.
Residual and associated deformities or cleft lip/cleft palate, particularly in the case of insufficient cheiloplasty in which the upper lip is too short. Superior repositioning of the mental osseous and the myocutaneous tissues can aid in achievement of lip competence and development of the upper lip
- II.
Requirement for a complimentary procedure to adjust lower anterior facial height when maxillary and mandibular osteotomies are performed for correction of anteroposterior and transverse maxillofacial deformities
- IV.
As an aid in stabilization of orthodontic treatment results by normalization of the osseous and myocutaneous elements of the lower face
- V.
As a complementary procedure with partial anterior glossectomy to aid in the management of dental open bite
TREATMENT PLANNING
A complete architectural and structural craniofacial analysis ( Figure 5-2 ) is carried out to determine the degree to which the individual patient varies from his or her “ideal.” This analysis demonstrates all of the maxillofacial deformities and imbalances that require correction.
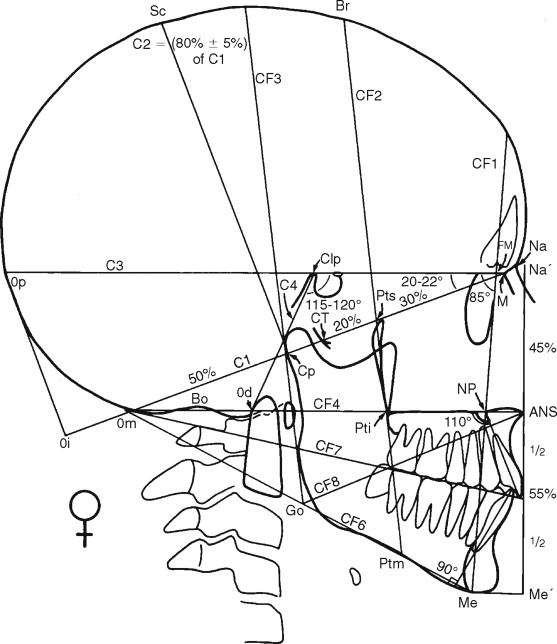
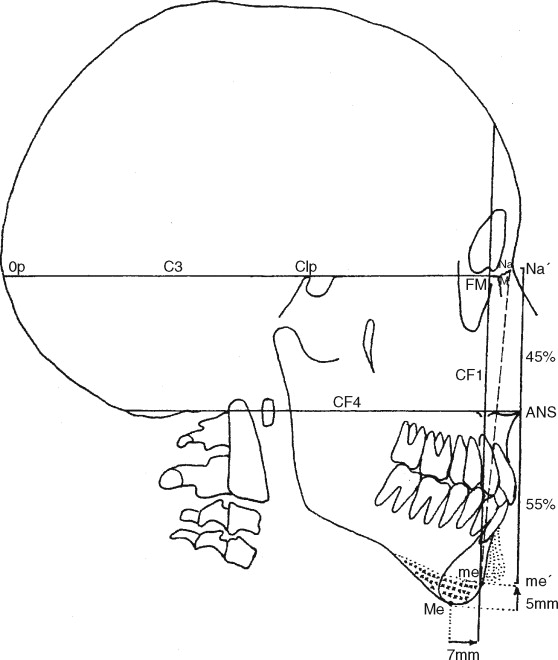
Although the principles and details of this analysis have been presented in previous articles, a brief review is presented here of those points and lines that are relevant to determination of the amount of osseous resection and chin advancement that will be required at surgery ( Figure 5-3 ).
Line C3.
The superior line of the cranial base is traced from point M , the junction of the nasomaxillary and nasofrontal sutures, to point Clp, the apex of the posterior clinoid process; it is extended until it intersects the external surface of the occipital bone at point Op, the most posterior extremity of the occipital bulbosity.
Line CF1.
The anterior line of craniofacial balance is traced through point FM, the frontomaxillary articulation, perpendicular to line C3 in adult males but at an angle of 85 degrees in women and children.
Line CF4.
The craniopalatal line is traced parallel to line C3 through point ANS, to a point just below the lowest point of convexity of the squamous occipital bone.
Line CF5.
The line of theoretical facial height is traced, by convention, perpendicular to line CF4 through point ANS. It is extended superiorly to point Ná, the projection of point Na, then inferiorly to point mé, the location of which is determined by the following formula:
This formula is derived from the fact that the upper anterior facial height, Ná − ANS, constitutes 45% of the total anterior facial height.
Once the Ná − mé distance has been calculated, the arc of a circle (center Na, radius Ná − mé) is traced via architectural and structural analysis. When this arc intersects, line CF1 is the “ideal” position of menton (point me). Both the amount of bone to be resected for the vertical correction and the distance by which the chin should be advanced can now be determined by comparing the ideal position of menton (me) with that of the patient’s real menton (Me).
This tracing maneuver is not valid when vertical maxillary excess, a significant open bite, or important anteroposterior deformities are present. In these cases, it is best to carry out the prediction tracing for correction of the major deformity, after which it is possible to apply the method described above to determine the amount of discrete osseous reduction and advancement of the chin.
In the particular case of open bite, it is possible to gain an appreciation of the amount of bone that ultimately will have to be resected by tracing the arcs of two circles—one with the center point I (the incisal tip of the mandibular incisor tooth), the other with the center Me (real menton), both with radius <SPAN role=presentation tabIndex=0 id=MathJax-Element-1-Frame class=MathJax style="POSITION: relative" data-mathml='ANS−me2+3mm’>ANS−me2+3mmANS−me2+3mm
ANS − me 2 + 3 mm
. Three millimeters must be added to the <SPAN role=presentation tabIndex=0 id=MathJax-Element-2-Frame class=MathJax style="POSITION: relative" data-mathml='ANS−mé2′>ANS−mé2
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


