History of the Procedure
Genioplasty using a sliding osteotomy via an intraoral approach was introduced more than 50 years ago. Trauner and Obwegeser and Converse and Wood-Smith described the technique for correction of microgenia in 1957 and 1964, respectively. This occurred along with the development of maxillary and mandibular osteotomies for orthognathic surgery. Later, attention was turned to slight modifications, such as performing an ostectomy for correction of macrogenia. In the 1980s, plate and screw fixation was introduced. This was an improvement over previous wire fixation for segment stabilization.
Genioplasty using alloplastic implants became an alternative method for increasing chin projection as various people published on this technique from the 1970s through the 1990s. Several implant biomaterials were introduced. They included solid silicone (Silastic), porous polyethylene (Medpor), mesh polymers (Dacron, Mersilene, Supramid), polytetrafluoroethylene and carbon fibers (Proplast), expanded polytetrafluoroethylene (Gore-Tex), and hydroxyapaptite. Silicone and porous polyethylene preformed implants are the main ones used today. In the future, tissue engineering may offer the ability to generate contoured facial implants composed of immunocompatible cells and a matrix construct.
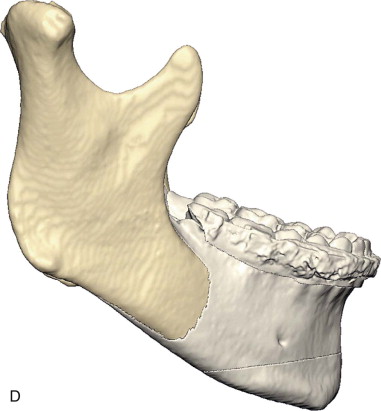
Recently, two- and three-dimensional digital imaging and planning programs have been developed (e.g., Dolphin Imaging). This technology enhances the surgeon’s ability to plan treatment and communicate with the patient. The surgeon performs the virtual treatment objective on a computer, and the patient views his or her morphed profile photograph. As the patient views the simulated profile change, he or she can appreciate and participate in treatment choices.
History of the Procedure
Genioplasty using a sliding osteotomy via an intraoral approach was introduced more than 50 years ago. Trauner and Obwegeser and Converse and Wood-Smith described the technique for correction of microgenia in 1957 and 1964, respectively. This occurred along with the development of maxillary and mandibular osteotomies for orthognathic surgery. Later, attention was turned to slight modifications, such as performing an ostectomy for correction of macrogenia. In the 1980s, plate and screw fixation was introduced. This was an improvement over previous wire fixation for segment stabilization.
Genioplasty using alloplastic implants became an alternative method for increasing chin projection as various people published on this technique from the 1970s through the 1990s. Several implant biomaterials were introduced. They included solid silicone (Silastic), porous polyethylene (Medpor), mesh polymers (Dacron, Mersilene, Supramid), polytetrafluoroethylene and carbon fibers (Proplast), expanded polytetrafluoroethylene (Gore-Tex), and hydroxyapaptite. Silicone and porous polyethylene preformed implants are the main ones used today. In the future, tissue engineering may offer the ability to generate contoured facial implants composed of immunocompatible cells and a matrix construct.
Recently, two- and three-dimensional digital imaging and planning programs have been developed (e.g., Dolphin Imaging). This technology enhances the surgeon’s ability to plan treatment and communicate with the patient. The surgeon performs the virtual treatment objective on a computer, and the patient views his or her morphed profile photograph. As the patient views the simulated profile change, he or she can appreciate and participate in treatment choices.
Indications for the Use of the Procedure
Genioplasty is performed to improve facial balance and/or rejuvenate the lower facial third. Evaluation of the chin in three dimensions is important for proper diagnosis and treatment planning. From the frontal view, the chin and inferior border of the mandible should be well defined and provide separation of the lower third of the face from the neck. The chin width should be in balance with the bizygomatic and bigonial facial widths. A narrow chin or a person with jowling and disruption of a smooth jaw line would benefit from lateral augmentation with an alloplast implant.
The chin’s vertical dimension influences vertical facial balance. The middle facial height (glabella to subnasale) and the lower facial height (subnasale to soft tissue menton) should be approximately equal. The lower third can be further subdivided. The upper lip length (subnasale to stomion superius) should be approximately one half the lower lip length (stomion inferius to soft tissue menton). The normal lower lip length is 40 mm (± 2) in females and 44 mm (± 2) in males. The normal hard tissue length of the chin or anterior dental height is measured from the mandibular incisor tip to the inferior border of the mandible. The average height is 40 mm (± 2) in females and 44 mm (± 2) in males.
If there is excessive lower facial height (in the presence of normal vertical maxillary position), a vertical reduction genioplasty with an ostectomy may be indicated. Conversely, if there is deficient vertical height, vertical augmentation of the chin may be indicated with an osteotomy and interpositional bone graft. Asymmetry of the vertical height may require a combination of ostectomy on the excessive side and use of the removed bone as a graft on the deficient side.
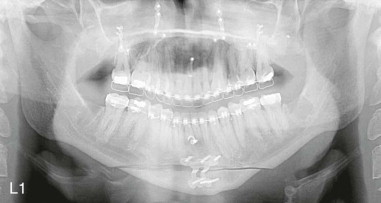
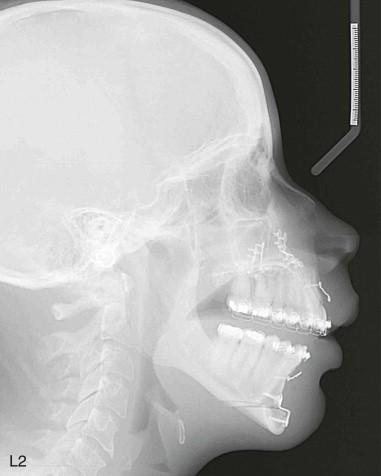
Chin projection should be in balance with the entire profile. The anteroposterior chin position can be assessed with cephalometric analysis. The bony chin position can be assessed with NB : pogonion and A : pogonion relationships to the lower incisor. The lower incisor tip and pogonion relationship to the NB line should be 2 : 1 to 1 : 1. The lower incisor tip should be on or 1 to 2 mm posterior to the line through A : pogonion. These analyses assume that the maxilla and mandible are in the proper anterior-posterior relationship to one another and that the lower incisor inclination is normal. Subnasale perpendicular can be used to assess the soft tissue chin position. Soft tissue pogonion should be 3 mm (± 3) behind this line. Generally, a stronger chin is considered masculine, and a retrusive chin is considered feminine.
These cephalometric analyses provide only some guidance. It is important to assess chin projection with other factors, such as chin shape, depth of the labiomental fold, lower lip position, and mandibular anteroposterior position. Cultural differences and trends are also important to keep in mind. For instance, a well-defined chin and jaw line with stronger projection often is seen as esthetic for females in Western culture. A weaker chin generally is considered more esthetic in Asian cultures.
An osteotomy is more versatile than an implant in altering the three-dimensional position of the chin. It can manage a sagittal and vertical deficiency or excess. It can also correct an asymmetric chin, such as that seen in hemifacial hyperplasia. An osteotomy is more commonly used as an adjunct to orthognathic surgery. If bimaxillary surgery is being performed, chin projection can be influenced by clockwise or counterclockwise rotation of the maxillomandibular complex. This may help avoid a genioplasty procedure altogether, especially in a patient with good chin shape to begin with.
Alloplast implants are limited to the correction of a sagittal and/or transverse chin deficiency. Implants offer several advantages, including ease of placement, cosmetic enhancement in chin projection and lateral jaw line contour (by effacing the pre-jowl sulcus), and structural stability. It is technically easier to widen the chin with an implant than an osteotomy and bone graft. Alloplast augmentation typically is used in the context of facial cosmetic surgery. For instance, an implant can be used to augment a deficient chin at the same time a nasal dorsal hump reduction is performed. The extended pre-jowl genial implant can be used for rejuvenation of the lower third of the face, either alone or as an adjunct to rhytidectomy, platysma plication, or neck liposuction. An implant improves structural support to the overlying lax or ptotic soft tissue. This has the effect of improving chin-neck esthetics and effacing a deep pre-jowl sulcus. The patient shown in Figure 29-1 has had an extended silicone genial implant placed in conjunction with a facelift and submental liposuction.


Limitations and Contraindications
Anatomic, physiologic, and psychological limitations should be considered when assessing a patient for genioplasty.
The locations of the inferior alveolar nerve and canine root apices, in addition to the vertical height of the chin, need to be assessed when an osteotomy is planned. Low-lying inferior alveolar nerves, long canine roots, and a vertically short chin make it more difficult to perform an osteotomy and have a decent-sized genial segment to advance. A sliding osteotomy can lead to notching of the inferior border of the mandible in these situations. In older individuals with prominent jowls, a sliding osteotomy also may deepen the pre-jowl sulcus and worsen the effects of aging in this area. An implant with a pre-jowl extension is likely a better choice in these situations.
In certain situations implants may not be a good choice. In younger individuals, an implant may contribute over time to more resorption of the underlying bone. Patients with labial incompetence and lip strain or hyperactive chin musculature may be more prone to bone resorption under the implant or displacement of the implant due to excessive forces. Some believe that a large augmentation is better served by osteotomy rather than an implant.
Medical conditions that can contribute to complications should be considered. The immunocompromised patient may not be a candidate for elective surgery. Diabetic control should be optimized before proceeding. If the patient is anticoagulated, this may pose a problem if medication cannot be safely discontinued before surgery. Tobacco use may complicate healing and should be discontinued. Surrounding soft tissue, odontogenic, or periodontal infection should be treated beforehand.
With any elective surgery, the patient’s chief complaint must be fully understood and addressed. The risks of the procedure and alternatives to care should be discussed and informed consent obtained. If the patient is mentally or emotionally unstable, he or she may not be a candidate for surgery. Also, if an adolescent does not have adequate family support and is poorly motivated for care, the procedure should not be performed.
Technique: Advancement Sliding Osteotomy
Step 1:
Incision and Dissection
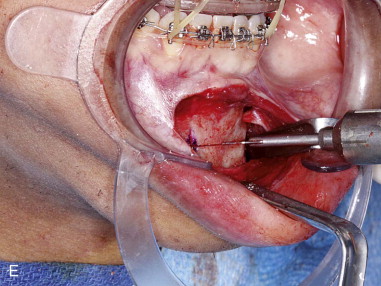
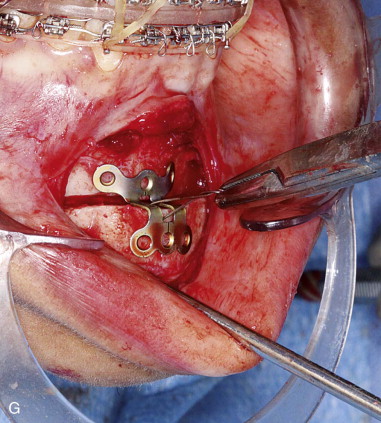
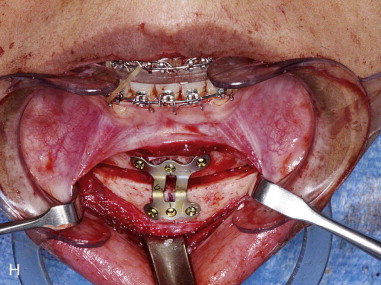
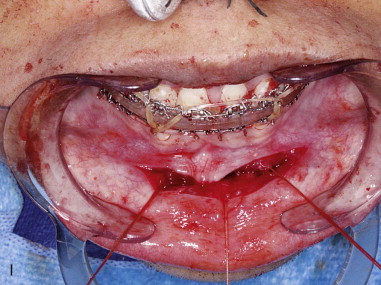
A local anesthetic with a vasoconstrictor is infiltrated into the submucosal tissue of the chin. It is helpful to place the patient in maxillomandibular fixation with elastics to stabilize the mandible during the procedure. Double skin hooks are used initially to retract the lower lip. Sometimes a self-retaining cheek retractor is useful for lip retraction instead.
After vasoconstriction has occurred, an incision is made through the lip mucosa from canine to canine, half-way between the depth of the vestibule and the wet-dry line, using a #15 blade and/or needle point electrocautery. The incision should traverse the mentalis muscle at an oblique angle so that an adequate portion is left attached to periosteum for muscle resuspension on closure.
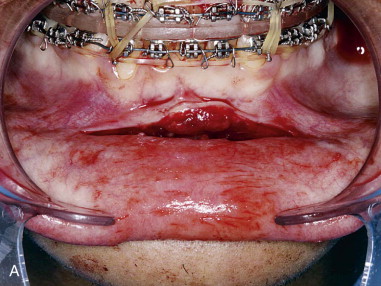
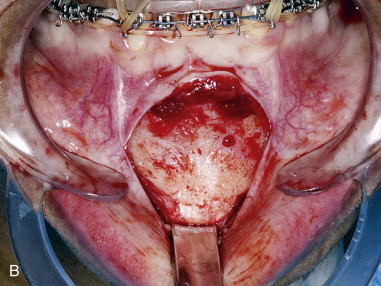
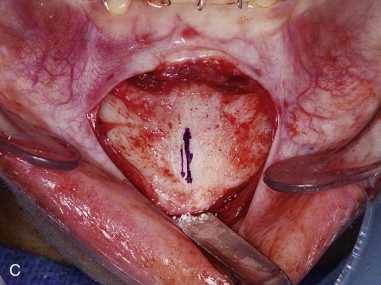
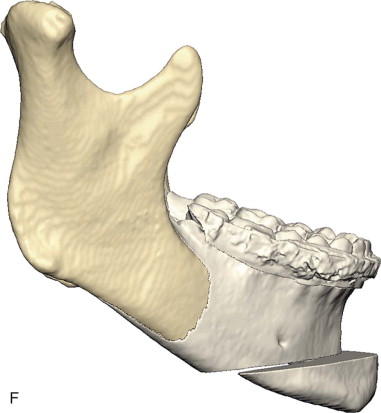
Subperiosteal dissection is performed with a #9 periosteal or larger Cobb elevator to fully expose the symphysis down to the inferior border. Elevate the periosteum and muscle overlying the incisor roots on the anterior mandible to make resuspension of the muscle easier when closing. Subperiosteal dissection is then carried posteriorly into the molar region, keeping the elevator along the inferior border well below the mental nerve. The dissection is finally carried superiorly to identify and expose the mental nerve where it exits the foramen. Avoid excessive dissection along the inferior border. It is important to maintain adequate soft tissue attachment for blood supply to the advanced genial segment. This, hopefully, minimizes long-term bone resorption ( Figure 29-2, A and B ).


Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


