Abstract
Pre- and postoperative longitudinal assessment of oral functions including masticatory force, masticatory ability with solids, speech intelligibility, and subjective satisfaction was conducted for patients who underwent vascularized osteocutaneous scapula flap reconstruction after mandibulectomy. Postoperative changes in oral function and patient satisfaction were examined in relation to tumour type (i.e., cancerous vs. benign). A change in masticatory force was associated with a reduction in the number of occlusal support zones after surgery and clearly differed by tumour type. Despite all patients showing reduced masticatory force postoperatively, all were satisfied with the improvements in eating and chewing, which were greater in patients with benign tumours than in those with cancerous tumours. Although both groups of patients expressed satisfaction with the aesthetic appearance after surgery, patients with cancerous tumours were more satisfied. However, both groups showed decreased speech intelligibility scores and lower satisfaction with speech after surgery. Preoperative support in the form of reassurance and helping to alleviate anxiety about postoperative appearance would be beneficial for all patients, with additional support provided based on the specific tumour type.
Even minor tissue loss and structural alterations as a result of treatment in the head and neck area may lead to marked dysfunction and disfigurement, with an enormous impact on somatic and psychosocial functioning. The mandible contributes greatly to the functions of mastication, swallowing, and speech, as well as to aesthetic appearance. The treatment of oral cancerous or benign tumours often requires radical surgery involving wide mandibular segmental resection and muscle displacement, and the resulting discontinuity in the mandibular bone coupled with the loss of muscular and soft tissue attachments can cause oral dysfunction and facial deformity ; this in turn can result in psychological problems and reduced quality of life (QOL). Moreover, after hemimandibulectomy, inadequate reconstruction of the bone can produce poor functional results including jaw swing, malocclusion, and the inability to chew solids. Reconstruction with autogenous bone to restore anatomic continuity is important for restoring mandibular function.
Over the past two decades, the fibula free flap has been used widely for oromandibular defect reconstruction. The vascularized osteocutaneous scapula flap has recently been reported to be a reliable, robust, and versatile flap with a long pedicle that has large-calibre donor vessels and minimal donor site morbidity. In addition, the natural scapular angle makes the scapula tip flap ideal for mandibular angle reconstruction. For these reasons, scapula free flap reconstruction is considered an effective option for patients with complex head and neck defects.
In our oral and maxillofacial surgery department, we have been designing surgical procedures to achieve ideal reconstruction—ideal in terms of anatomic continuity and position, as well as restored oral functions, mandibular movement, and facial contour. To prevent poor functional results after segmental mandibulectomy or hemimandibulectomy, we have been using vascularized osteocutaneous scapula flaps to reconstruct discontinuities of the mandible and soft tissue defects. However, if oral surgeons fail to consider the surgical procedure, postoperative oral functions, and postoperative satisfaction in advance, the patient will be dissatisfied, even though the surgical outcome may be ideal from the oral surgeon’s perspective.
To date, there have been relatively few comprehensive longitudinal studies on pre- and postoperative oral functions and QOL following reconstruction, and the studies that have been performed have often included a limited number of patients. In particular, few studies have examined the perioperative outcomes of patients who have undergone mandibular reconstruction with scapular bone.
Many problems have been encountered in understanding and improving postoperative oral functions and patient satisfaction in patients who have undergone mandibular reconstruction after segmental mandibulectomy or hemimandibulectomy. Therefore, in this study, we focused on patients who required scapula bone flap reconstruction and examined the longitudinal changes in the functional outcomes of masticatory force, masticatory ability with solids, and speech intelligibility. In addition, as a partial indicator of health-related quality of life (HRQOL), we targeted subjective satisfaction with eating, chewing, aesthetic appearance, and speech, which are directly affected by mandibulectomy and bone reconstruction.
There are also no previous studies on the differences in oral functions and subjective satisfaction for oral functions between patients with cancerous tumours and those with benign tumours after scapular bone flap reconstruction following mandibulectomy. Investigating the objective values of oral functions and HRQOL after surgery and comparing them between the types of disease to identify whether or not the changing trends improved oral functions and HRQOL is considered important for assessing and reconsidering surgical procedures. Thus, we compared these factors by tumour type (cancerous vs. benign).
Materials and methods
This longitudinal study involved patients who underwent reconstruction with a vascularized osteocutaneous scapula flap after mandibulectomy at a department of oral and maxillofacial surgery in a university hospital between April 2008 and May 2012. The study complied with the principles laid down in the Declaration of Helsinki and approval for this study was obtained from the institutional research ethics committee.
Patients
The main inclusion criterion was a diagnosis of benign primary tumour of the mandible or primary central carcinoma of the mandible and squamous cell carcinoma of the lower gingiva. In this study, we planned to compare the longitudinal differences in oral functions and patient satisfaction between patients with benign tumours and those with cancerous tumours. Because postoperative oral functions and satisfaction vary according to the type of treatment performed, particularly in cancer patients, we also set the following additional inclusion criteria: (1) no induction or adjuvant therapy received at any of the study time points; (2) neck dissection performed from level I to level II or III; and (3) no extensive oral soft tissue resection of, for example, the oral floor or tongue, with the mandibulectomy.
We recorded all measurement parameters, described in detail below (i.e., masticatory force, occlusal contact, masticatory ability with solids, speech intelligibility, and patient satisfaction), 1 day before the reconstructive surgery. The postoperative assessment, in which all cases of scapular and mandibular bone union were observed radiologically, was performed 1 year after the reconstructive surgery because this timing was appropriate for postoperative denture-making if patients so desired. Socio-demographic data and disease-related information were obtained from patient medical records. Patients who met the criteria were provided with a detailed explanation of the purpose of the study and written informed consent was obtained from all who agreed to participate.
Reconstructive technique
In cases of segmental mandibulectomy in which we expected to restore occlusal contacts and mandibular position, we prepared a bite plate to record preoperative occlusion. We also prepared a provisional metal plate called a ‘memory plate’ that was bent to bridge the mandibular discontinuity and which was to be replaced by the bone flap. The resected region was simulated in a preoperative three-dimensional model of the mandible. At the memory plate bridge, the bite plate was bitten to stabilize occlusion before placing the vascularized osteocutaneous scapula flap. In cases involving resection of the mandibular condyle where the articular disc could be preserved, we shaped an autologous bone graft into the shape of the condyle and connected it to the articular disc.
Masticatory force
Quantitative evaluation of masticatory function was investigated pre- and postoperatively using chewing gum (70 mm × 20 mm × 1 mm, 3.0 g; Masticatory Performance Evaluating Gum XYLITOL; Lotte Co., Ltd, Saitama, Japan). Before mastication, this chewing gum has a yellowish-green colour. As mastication proceeds, the acidic condition in the mouth changes the colour to red. This gum can be adjusted so as not to adhere to denture materials to allow for easy chewing, even by complete denture wearers with reduced masticatory force.
Patients chewed the gum as much as possible using both sides, without restriction, for 2 min. The chewed gum was collected immediately after chewing and compressed to a thickness of 1.5 mm in a polyethylene film between two glass plates. The a * value (CIE-L*a*b*colour space) was then measured through the polyethylene film using a colourimeter (CR-13; Konica-Minolta, Tokyo, Japan). The colour readings were performed at five points on a single side to determine the mean value. As a previous study has shown that a * values correlate positively with masticatory force and are sufficient for evaluating masticatory performance, we defined these values to indicate masticatory force. If the patient used a removable dental prosthesis in daily life, such as when eating, the gum test was performed without the prosthesis. The postoperative change in masticatory force (%) was calculated as follows: (postoperative masticatory force − preoperative masticatory force)/(preoperative masticatory force) × 100.
Occlusal contact
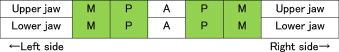
Postoperative occlusal contact status was evaluated based on the number of occlusal support zones, which relate to occlusal contacts. An occlusal support zone was defined as a zone in which a minimum of one tooth in the left or right premolar or molar region is in contact with a tooth in the upper and lower jaw. Antagonist contact in the anterior dentition was not counted as comprising an occlusal support zone. Figure 1 shows a frame diagram of the dentition and occlusal support zones.
For patients using a removable dental prosthesis, we recorded occlusal contacts of natural teeth only without the prosthesis in place. We then recorded the reduction in the number of occlusal support zones postoperatively.
Masticatory ability with solids
Liquid nourishment by feeding tube or consuming pureed food by mouth decreases the enjoyment of eating, and coupled with a lack of textures and mastication, the result is decreased HRQOL. Masticatory ability with solids was evaluated postoperatively using a modification of the method established by Yamamoto et al. Briefly, foods were ordered from soft (category 1) to hard (category 6), and we used the highest category that included more than half of the foods the patient could chew as the score of masticatory ability with solids. The foods included in each category are listed in Table 1 .
| Food categories for masticatory ability with solids | |
|---|---|
| 1 | Pureed food; rice gruel; paste steamed vegetable |
| 2 | Custard pudding; tofu (bean curd); steamed vegetable; soft boiled noodles |
| 3 | Boiled rice; boiled egg; banana; boiled fish |
| 4 | Fresh lettuce; potato croquette; butter cookie; ham |
| 5 | Elastic hard fish sausage; salami; sliced apple; beef steak |
| 6 | French bread; rice cracker; pickled vegetables; peanuts |
Speech intelligibility
Speech intelligibility was evaluated using Furuya’s speech articulation test. Each patient pronounced 100 Japanese syllables listed randomly on a test sheet and five listeners unfamiliar with the patient noted each pronunciation. The speech intelligibility score is expressed as the mean percentage of correct responses from the five listeners.
Patient satisfaction
Patient subjective satisfaction with eating, chewing, aesthetic appearance, and speech was scored using visual analogue scales (VAS).
Statistical analysis
We compared the differences in age between the benign and malignant tumour groups by one-way analysis of variance (ANOVA), and sex, pre- and postoperative occlusal support zones, reduction in the number of occlusal support zones, and denture usage after surgery using the χ 2 test or Fisher’s exact test for categorical data. Differences in the pre- and postoperative oral functions and patient satisfaction according to tumour type (cancerous vs. benign) were analyzed by repeated ANOVA and post hoc comparisons (Scheffé’s F test; 95% significance), respectively. All statistical analyses were carried out using SPSS for Windows version 17 software package (SPSS Japan Inc., Tokyo, Japan). A P -value of <0.05 was considered significant.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


