Fig. 10.1.
a Freely developing a given potential, unimpeded and unobstructed by external forces, while receiving sufficient, continuous nutrition in well-calculated doses – this is the objective of any life form. What is true of large plants is equally true of the life of any single cell, and of any bone as a whole, and of any individual bone cell. A lack of nutrients and the displacement by competitive growth of indigenous as well as exogenous organisms can cause the bone’s chance of survival to deteriorate. To our eyes, this tree appears to be vertical, although the tree trunk is actually not oriented at a 90° angle to the ground. b The effects of asymmetrical muscle power are similar – to stay within the same metaphor – to those of a strong earthquake that changes the orientation of objects relative to the ground. External physical factors may cause firmly anchored trees to grow in a slanted direction. The cause of asymmetries in humans is usually located inside the affected organism itself and it may be definitively forgotten. Often long forgotten sufferings remain persistent in single muscles contractions throughout life
In actual reality, the small shift between Fig. 10.1a and Fig. 10.1b requires extremely rapid and adequate adaptation, the extent of which is always difficult to perceive: With trees, the balancing mass is hidden underground. In the human body, any asymmetries that exist may be concealed from sight by the soft tissues.
10.2 Introduction
The chewing function can only be fully restored if adjustments are made to obtain a balanced mastication pattern. Traditionally, it has been attempted to achieve this goal by orthodontic, conservative and prosthetic means. Today the spectrum also includes implantological options. We believe that questions relating to masticatory function will define the future of dental implantology and of dentistry at large. Current periodontological, orthodontic and prosthetic concepts need to be thoroughly reviewed and modified based on the realization that any teeth as well as periodontal and bone structures can only be preserved in a lasting manner if all essential functional requirements are satisfied. These requirements will be discussed in the present chapter.
Early intervention is a prime prerequisite for effective functional rehabilitation. All specialists involved in the treatment must respect the overriding importance of the functional treatment objective. The scientific foundations for the treatment rationale described in this chapter are easy to understand (Planas 1992). In this chapter, the reader will learn why the restorative dentist must aim to achieve a stable masticatory function, what he must do to preserve it, and why he should make the necessary adjustments even in situations where the treatment requirements to achieve this goal are extensive.
Patients seeking dental treatments are usually better aware than the dentist what type of problem they actually have. However, since they can neither describe nor demonstrate the problem, they tend to defer to the dentist’s judgement. The fact that the thoughts of today’s dentists are inordinately centred on technical terms does not help to bridge this communication gap either. People who walk with a limp can communicate their problem better both because they can observe themselves better and because the problem is also visible to others. Unilateral chewing patterns are not usually visible to outsiders, and they cannot be corrected as long as the pathways for bilaterally balanced movements are blocked by muscles and/or hard-tissue structures. Sometimes one cannot help getting the impression that all basic knowledge that a student naturally possesses on entering a dental school is effectively buried under a flood of knowledge by the time he or she eventually graduates. In a sense, novices have a better intuitive knowledge of how “chewing” works.
In the present chapter, we can only explain the key features of the therapeutic strategy and discuss the basic considerations involved. Practice and experience as well as an uncompromising treatment strategy are the quintessential requirements for successful outcomes. We used to apply the minimal therapeutic solutions taught at the universities and imposed by health insurance providers ourselves for many years. We therefore had ample opportunity to see what disadvantages they involve in the medium and long term. Today we decline any treatment requests that are not aimed at establishing a balanced masticatory function. Surprisingly, the conventional strategy of offering restorative treatment in a piecemeal manner without an overall concept for the masticatory apparatus at large has been used throughout history. Based on this strategy, the patient is left without a balanced masticatory function until he or she has finally reached the point where a complete denture is inserted. This is the first time when a balanced masticatory function is actually established, if only to ensure that the denture is acceptably retained. With the help of BOI implants, we are today able to implement fixed enossal support in a timely, reliable and comprehensive manner. They enable us to intervene in any phase of the gradually progressing collapse of masticatory function without regard to the amount of vertical bone available.
Mastication therapy is the only reliable way to preserve bone by adequate function.
BOI implants offer absolute freedom in the spatial positioning of superstructures, thereby giving us an opportunity to define the position and orientation of masticatory surfaces solely by functional considerations. The treatment objective is to create a laterally oriented masticatory function that is balanced on both sides of the jaw.
10.3 Decompensation of the Masticatory Apparatus
It is always necessary to analyse the aetiology of diseases or dysfunctions before any considerations related to the treatment as such can be made. A wide variety of parameters – including the size of teeth, the size and position as well as the foundations and suspensions of the basal jaw segments, the occlusal plane, the quality and length of the chewing muscles, body posture and mimic muscles – are intertwined in a biophysical continuum that remains to be investigated in detail. These parameters come in countless configurations. In this way, the functional spectrum of human development has to be extremely broad to allow “serial production” of functional individuals even under the most adverse of conditions and the most inappropriate of configurations. In engineering terms, one could say that the production-related and structural tolerance limits are used to the fullest extent possible. These processes are driven by growth and function. Once the endpoint of growth has been reached, the only force that continues to influence morphology in constructive manner is the force of function. In addition, degenerative and hormonal influences are gradually coming to the fore as well.
Once the endpoint of growth has been reached, functionally viable results will be present even though the departure points may have been extremely different or unfavourable. However, not all of these results are stable. Some of them are “just about” balanced rather than “well” balanced. The chances that these results can remain stable for a lifetime are slim. The phase of growth is followed by a phase of decompensation that will last for the rest of the patient’s life and is triggered by asymmetrical function – that is to say, by the fact that elements of the skeletal system are utilized in a non-balanced manner.
The main factors responsible for the progressive decompensation of the masticatory system are illustrated in the following subsections. The important part for the daily requirements of diagnosis and treatment in the dental office is to identify the temporal sequence and relative importance of these various factors in each patient’s gradual decompensation of the masticatory function. We are talking about the impact of joints, muscles and masticatory surfaces, but we are also talking about the “sloth factor” as a basic principle of all human existence. With regard to our topic at hand, this means that an individual will always prefer the “easier” chewing side, even though a voluntary effort to use the side where chewing is harder would actually be the gentlest treatment imaginable.
10.3.1 Avoidance Patterns
Reflexive avoidance of pain has the greatest effect on function and, by implication, on form. According to Kawamura (1974), masticatory movements are regulated by the following factors:
1.
Muscle-related factors
A.
Muscle spindle mechanisms in muscles attached to the mandible
B.
Stimuli coming from Golgi’s corpuscles in the muscles attached to the mandible
C.
Afferent stimuli coming from the neck muscles
D.
Pain in the muscles attached to the mandible
2.
TMJ-related factors
A.
Stimuli coming from mechanoreceptors in the articular capsule
B.
Afferent stimuli coming from accessory ligaments
C.
Pain originating from joint structures
3.
Oral, facial and perioral soft-tissue sensations (pain, stiffness, mechanical sensations and thermal stimuli)
4.
Tooth-related factors
A.
Toothaches and periodontal pain
B.
Stimuli coming from the periodontal ligament
5.
Pharynx-related factors: Pain, hypomobility, injuries, thermal stimuli
Premature contacts associated with tilted and/or elongated teeth may gradually give rise to deviations that change the position of the mandible relative to the teeth in the maxilla, causing the chewing activity as well as the activity of chewing muscles to shift towards other jaw regions without causing acute pain.
Most denture-related pressure sores, but also periodontally induced tooth mobility and destruction, will massively regulate the masticatory force downward, something that is ultimately also tantamount to pain avoidance.
10.3.2 Unilateral Chewing and Side Switching
Any edentulous spaces, tilted teeth and/or premature contacts will reduce the efficiency of chewing, a greater effort is required to achieve the same chewing results on the affected side as on the intact side. The brain will quickly register this imbalance and switch the chewing load to the intact side. The teeth of the support zone on the working side are rather prone to intrusion, whereas the contralateral teeth are more likely to hypererupt over time due to the smaller intrusive effect of the chewing muscles on the non-working side. At the same time, the teeth on the working side of the maxilla will migrate somewhat in a centrifugal direction, while the contralateral teeth are more likely to undergo medialization. This process is clinically and radiographically evident as a midline shift towards the working side. As the functional masticatory angle of Planas (AFMP, angles fonctionnels masticatoires de Planas) on the non-working side changes as a result of mesialized and elongated teeth, the chewing pattern becomes unilateral for good. The greater the bilateral discrepancy in terms of AFMP angles, the more pronounced the unilateral pattern. The patient will increasingly have trouble chewing on the non-working side as the extent of mouth opening required on that side to do so will increase steadily. Interestingly, the chewing side is not defined by the absolute value of the AFMP angle but by the relative difference between both angles. Patients with deep-bite relations may thus reveal a large AFMP angle because their occlusal relations do not permit any flat lateral chewing movements in the first place.
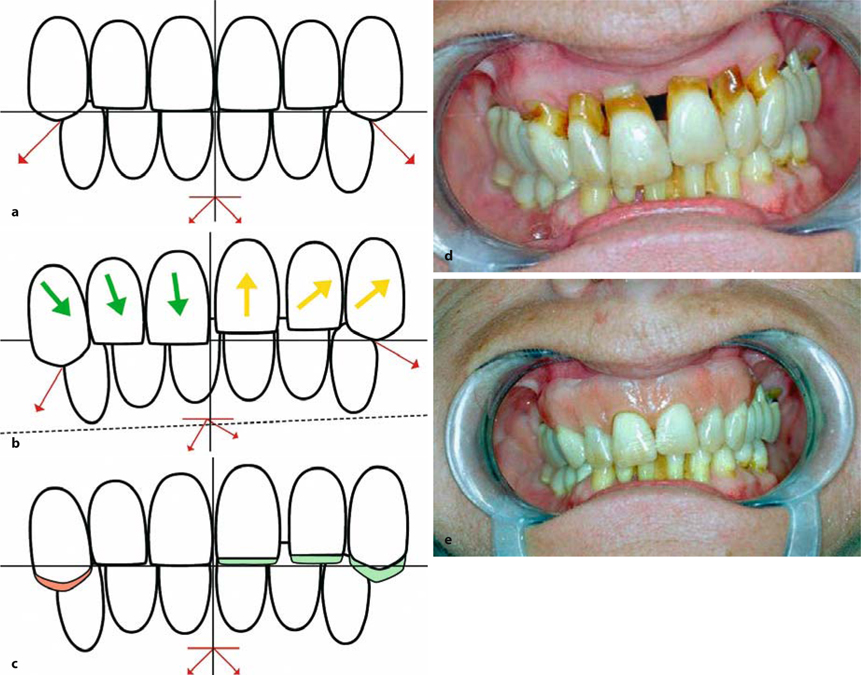
Fig. 10.2.
a Baseline situation with aligned midlines and symmetrical AFMP angles. For maintaining equal mastication on both sides of the jaw, it is not really important to have smaller or larger AFMP angles. It is only important that the angle shows the same value on both sides, b In the event that one side develops out to become the preferred chewing side (here right side of picture), the midline shifts to the working side. Teeth on this side are intruded and flared lateral, while the dentition on the non-chewing-side are elongating and move medially (green arrows). The occlusal plane descends, and the AFMP angle increases on the non-working side, c In order to correct this, material must be added to the crowns on the working side. At the same time grinding of medialized cusps on the non-working side is performed. This way the bite is being lifted “unilaterally„ on the working side, d Typical clinical situation after a unilateral chewing pattern has been present for many years. Teeth 21 and 22 were intruded by the masticatory force while teeth 11 and 12 became elongated. e In the absence of gingival recession, or if the dental necks are covered by an epithesis (as in this figure), the true relationships are actually not too obvious. Dentists are used to an overly narrow field of vision. Deviations of the masticatory plane are more obvious when viewed from a distance
Developments such as these can be readily verified in the OPG if they only are present long enough. Not only does the midline shift become evident, but the condyles obtain different shapes due to the loading imbalance. The condyles on the working side will be large and rounded, while those on the non-working side will be flattened towards the anterior. More importantly, the long distance they have to cover as they advance forward will make them smaller on the whole. The articular eminence will become flatter as well.
If the alternative chewing side is missing already and the chewing ability on the preferred side is lost into the bargain, the patient will quickly seek implant treatment. In this situation, many patients report that the loss of one specific tooth has left their chewing ability seriously impaired. Their dentists, on the other hand, will often find it hard to understand or downright illogical why one specific tooth should have had such far-reaching consequences when multiple teeth are missing. The dentist should consider himself warned by such statements. After all, any kind of dental treatment should always aim to establish a complete set of masticatory surfaces that interact equally well throughout. The patient should be advised to have the restorative treatment performed comprehensively rather than unilaterally. This is the only way to treat the unilateral pattern with a relatively good chance of success, thereby greatly enhancing both the longevity of the implants and the outcome of the restorative treatment at large. In crestal implantology, a terminal implant in the first premolar position is sometimes added due to the heavy dependence of these designs on the vertical thickness of the available bone structure. Some authors even recommend placing any implant-supported crowns slightly below the level of occlusion. While we shall ignore for the purpose of this discussion whether treatments of this type make any sense at all, they are clearly unnecessary and indeed counterproductive with BOI implants. After all, it is virtually always possible to place these designs in the tuberosity area to obtain technical abutments in these positions, so that a functional occlusal table can be established that extends right to the position of the first molar. In this way, it is always possible to establish a uniform mastication pattern characterized by masticatory surfaces of equal length and width on both sides of the jaw. The development of a preferred chewing side cannot be avoided if the APFM is too different over a period of time. On the other hand, absence of distal balance on one side will also trigger the development of a preferred chewing side even in cases with symmetrical AFMP angles. We learn from this that gaps in the arches are often less determining for the deterioration of the chewing pattern than differences in AFMP angles (with subsequent vertical differences between the sides) and differences in the situation of distal balance. In fact a preferred chewing side will intrude the teeth in both arches of this side and lead to elongation on the opposite site. This alone prevents balance when the individual tries to use the non-chewing side during mastication.
10.3.3 Restricted Movement
Problems related to mastication may be caused by restricted movements. Muscle parts unused over longer periods yield the same effect as dissected or paralysed muscles. Malpositioned teeth will block regular movements and give rise to cramps or atrophy of muscles. Having been present for a long time, these problems will persist even after the cause has been removed (e.g. after tooth loss). Restricted chewing movements may occur at any time and have to be treated without delay.
The diagnosis is simple:
-
On being asked to perform chewing movements with the oral cavity empty, the patient will reveal one of the following movement patterns:
-
Pure chopping movements
-
Advancing movements (anterior chewing pattern)
-
Unilateral lateral movements
-
Bilaterally balanced grinding movements
Pure chopping movements and advancing movements are mainly observed in situations of deep bite/vertical overbite (i.e. in cases of primary TMJ dysfunction). Unilateral lateral movements are observed in the presence of discrepant AFMP angles. Bilaterally balanced grinding movements are only observed when the AFMP angles are about equal.Precautions must be taken to prevent restricted chewing movements in the treatment phase. -
-
When the dentist inserts the prosthetic super-structure, he or she must look beyond occlusal parameters but ensure that a uniform mastication pattern is within reach for the patient. Due to peripherally or centrally induced persistent muscle dysfunctions, patient with pre-existing functional disorders are rarely able to perform bilateral grinding movements right away after, even if “all” interferences have been eliminated and the AFMP angles optimally adjusted. These patients need to undergo periodic treatment sessions to relax their muscles and practise appropriate chewing movements under physiotherapy guidance. We found that a period of 3–4 weeks between adjustment sessions is better than applying changes at shorter intervals. The muscles need this time to establish a new (pre-)final balance, arrange for sufficient blood supply and drainage and build up forces.Physiotherapists like to perform their treatments at short intervals (either daily or every other day), presumably to optimize their schedules. We do not think that these short intervals are appropriate when the objective is to stabilize the masticatory pattern. In our experience, it is better to perform physiotherapeutic sessions once a week, with chairside subtractive/additive adjustments after every three to four sessions. The muscles associated with seriously dysfunctional dentitions simply need more time to adapt and to recover a desirable level of masticatory forces. Physiotherapeutic sessions performed at shorter intervals raise the overall costs without achieving their objectives more effectively or even faster.
-
More information on position-related problems can be obtained by observing the closing movement of the jaws. If this movement proceeds smoothly without involving midline deviation, then the midline is presumably correct. A twitching movement, by contrast, indicates that the habitual occlusion is at variance with the retral and horizontal TMJ positions. These muscle twitches indicate the presence of an abnormal intercuspidation pattern. While anatomical landmarks are also informative, they are not altogether reliable, considering that all cranial structures are mobile relative to the centre of the skull. Both the labial frenulum and the line of the median raphae may change relative to the centric position of the mandible.
-
If the bone volume in the maxilla is small and asymmetrical, or if the configuration of BOI implants is asymmetrical, then the implant-restoration will not be uniformly stable against the cranially oriented chewing pressure. The same is true if the chewing forces are not balanced on both sides of the jaw at the start of treatment. From a clinical viewpoint, the resultant implant-restoration systems will be asymmetrically intruded once they are osseointegrated. This may quickly give rise to a slanted masticatory plane and discrepant AFMP angles with all the functional consequences described for this type of situation.
-
Once the teeth have erupted, their arrangement will be defined by occlusal and masticatory parameters during normal physiological development. In this process, the bony macrotrajectories are reconfigured in such a way that tooth position remains relatively stable. In the presence of excessive muscle forces, the teeth participating in mastication may change their position such that the bony macrotrajectories take over from the occlusal structure as the main determinant. In these situations, individual teeth will change their position and acquire non-physiological contact positions or lose contact with their antagonists. This process may occur at any age. In many cases, the enhanced muscle tone is due to psychological tensions. Hypertonia of the internal chewing muscles cannot be visually detected. The reader is referred to Chapter 17 for a detailed discussion of craniomandibular syndromes in patients with psychological disorders (Chapter 17).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


